
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6636
Case Report(ISSN: 2637-6636) 
Pulpotomy in Young Permanent Teeth with Signs of Apical Periodontitis: Case Series Volume 8 - Issue 4
Zivile Grabliauskiene and Greta Lodiene*
- Department of Dental and Oral Pathology, Lithuanian University of Health Science, Lithuania
Received: July 19, 2022; Published: August 03, 2023
*Corresponding author: Greta Lodiene, Department of Dental and Oral Pathology, Lithuanian University of Health Science, Eiveniu 2, Kaunas, Lithuania
DOI: 10.32474/IPDOAJ.2023.08.000294
Abstract
Background: Despite the long-standing concept of pulp tissue necrosis as the main etiologic factor for periapical lesions, there has been new evidence that inflamed vital dental pulps can cause apical periodontitis (AP). Infected pulp could heal when the etiological factor is eliminated. The present cases aimed to assess the outcome of vital pulp therapy (VPT) in permanent teeth with vital pulps and signs of an AP.
Cases presentation: In the first case report a 15-year-old boy presented with a chief complaint of constant pain in #15 tooth, lasting for five days. After the clinical and radiographic examination, a diagnosis of pulp necrosis and symptomatic apical periodontitis was conducted, and the root canal treatment (RCT) was initiated. The pulp chamber roof was removed. No intense bleeding and coherent vital pulp tissue were observed; however, the pulp was in dark red color. VPT (pulpotomy) was decided to be performed. In the second case a 16-year-old girl presented for an annual observation. After clinical and radiographic examination, #45 tooth was diagnosed with caries. The excavation revealed caries lesion reaching the pulp. The exposed pulp was bright red color, no intense bleeding overflowing from the exposure site was observed. VPT (pulpotomy) was a treatment of choice. In both cases a layer of hydraulic calcium silicate cement was applied over the vital pulp tissue. In the second case a periapical radiograph performed after the treatment revealed the large apical radiolucency. The teeth crowns were restored with the glass ionomer cement initially or composite resin permanently, in the first and second case, respectively. At the follow-up visits, the patients reported no symptoms. The dental periapical radiographs showed radiolucency considerably reduced in size and completely healed after one year and two years.
Conclusion: Clinical and radiographic evidence of cases showed the successful use of mineral trioxide aggregate for pulpotomy of mature teeth with vital pulps and signs of apical periodontitis.
Keywords: Vital pulp therapy; pulpotomy; apical periodontitis; mineral trioxide aggregate
Abbreviations: VPT: Vital Pulp Therapy; AP: Apical Periodontitis; RCT: Root Canal Treatment; IP: Irreversible Pulpitis; MTA: Mineral Trioxide Aggregate
Background
Inflamed pulp has the ability to heal when the etiological factor is eliminated. According to the guidelines, vital pulp therapy (VPT) is primarily indicated for immature permanent teeth with reversible pulpitis caused by mechanical pulp exposure during carious excavation operative procedure or a traumatic pulp exposure of healthy teeth with minimal bacterial contamination [1,2]. Considering a mature permanent tooth as a candidate for VPT requires careful assessment of the extent of damage to the pulp tissue using clinical and radiographic measures [3]. The pulp condition, routinely preoperatively suspected of past and present signs and symptoms and reactions to clinical tests, must be confirmed intraoperatively by assessing pulp bleeding, tissue colour and consistency [4]. The critical point in the success of VPT is the continued vitality of the tooth, especially the presence of sufficient blood supply to advance [5]. AP has been demonstrated to be a direct extension of pulpitis into the periapical tissues before total pulp necrosis [6]. Periapical changes, including the sprouting of nerve fibres, appeared following the establishment of irreversible pulpitis after pulp exposure lesions [7]. Therefore, identifying microorganisms in pulpitis, especially with periapical rarefaction and periodontal ligament widening in the radiography, can be promising in diagnosing the severity of inflammation. In addition, it can result in new treatment methods by interfering with the microbiota ecosystem [8,9].
The regeneration and preservation of vital dental pulp with vasculature and nerve components remain one of the significant challenges in modern therapies [10]. The periapical lesion represents a local immune response to the pulp infection. It may be viewed teleologically as a second line of defence, the purpose of which is to localise the infection within the confines of the root canal system [11]. The pulpal and periapical innervation may modulate several aspects of the inflammatory response via the secretion of neuropeptides, a process referred to as neurogenic inflammation, in addition to mediating pain perception [12]. The term neurogenic inflammation has been developed to describe the component of inflammation caused by an appropriate stimulus applied to peripheral neurons, which leads to the release of neuropeptides that alter multiple processes, including vascular permeability and vasodilation at the site of injury [13,14]. For this reason, it is widely accepted that the nervous system contributes to the pathophysiology of peripheral inflammation. A neurogenic component has been implicated in many inflammatory diseases, including oral diseases such as periodontitis and pulpitis [15]. Periapical inflammatory infiltrates, increased osteoclast numbers, and bone destruction is apparent well in advance of total pulpal necrosis, with vital pulp tissue still present in the apical portions of the root canal [16,17]. This finding explains the common clinical observation that vital tissue (and pain) may occur even in teeth with radiographic evidence of periapical bone destruction. Hence, the present cases aimed to assess the outcome of VPT in permanent teeth with signs of an apical periodontitis (AP).
Case 1 Presentation
A 15-year-old boy presented to the dental office of one of the authors (ZG) with a chief complaint of constant pain in #15 tooth, lasting for five days. The tooth was painful on biting. The patient has taken Ibuprofen 400mg, one tab./3 times per day. The patient mentioned that six months earlier, he had suffered a few days of spontaneous pain of this tooth. At that time, he visited a dentist, but the tooth was not painful anymore, was free of caries and the restoration was of good quality. Therefore, the treatment was postponed. Clinical examination of #15 tooth revealed restoration on the distal contact surface and the tooth free of caries. The cold test (Cold Spray, Polydent, Germany) was negative on the observational tooth, whereas positive responses were elicited in the adjacent teeth. Tooth #15 was sensitive to percussion with standard periodontal probing depth (2 mm) around the tooth. Periapical radiographic examination revealed periapical radiolucency and apical root resorption of #15 tooth (Figure 1).
Figure 1: Case 1. Pre-treatment periapical radiograph of tooth 15 showing the periapical radiolucency and inflammatory root resorption.

After clinical and radiographic examination, a diagnosis of pulp necrosis and symptomatic AP was made on #15 tooth and the RCT was initiated. The parents and child were informed of RCT’s risks, complications, and possible outcomes. At the first visit, under dental microscope and rubber dam isolation, an endo access cavity preparation was started using a round diamond high-speed bur (Hager & Meisinger, Germany) with water coolant without local anesthesia. Close to the pulp chamber, the patient complained about the pain. Local anaesthesia was performed using 4% articaine - epinephrine 1:100000 (Ubistesin forte, 3M Science, USA). The pulp chamber roof was removed with sterile round diamond highspeed bur (Hager & Meisinger, Germany). No intense bleeding and coherent vital pulp tissue were observed; however, the pulp was in dark red color. Vital pulp therapy (pulpotomy) was decided to be performed. After explaining the possible risks of VPT, the written informed consent from the patient’s parents was obtained. The pulp tissue was removed with a sterile long-shank, high-speed, round diamond bur (Hager & Meisinger, Germany) until the attached pulp tissue was observed.
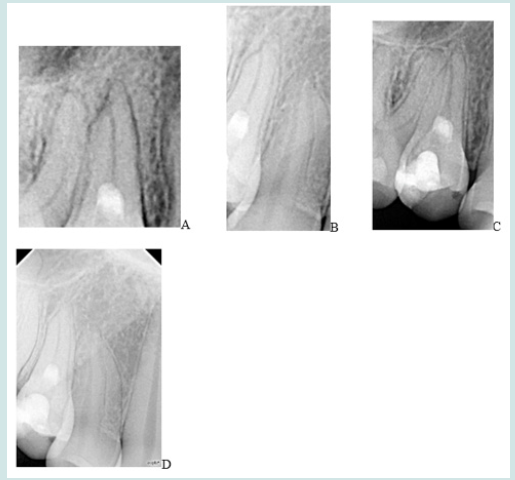
The bleeding was stopped in 2 min. with a cotton pellet soaked in 2,5% sodium hypochlorite solution (Cerkamed, Poland) (Figure 2). A layer of hydraulic calcium silicate cement MedcemMTA (Medcem GmbH, Austria) was applied over the vital pulp tissue and periapical radiograph was performed immediately after the treatment (Figures 3A & 3B). The endo access cavity was sealed with glass ionomer cement (GIC) (i-Fil, Vita Zahnfabrik H. Rauter GmbH & Co. KG, Germany). The patient and his parents received oral hygiene instructions and were informed about the emergency visit in case of pain or swelling. Two weeks later, the patient returned for a permanent restoration. The GIC was removed, leaving a 2mm layer on the Medcem-MTA. The final resin composite (ONE shade, Olident, Poland) restoration was performed, followed by the finishing and polishing procedures. The treated tooth was followed 4, 8,12, 24 months after the treatment. The patient had no complains. Clinical examination revealed no sensitivity to percussion and palpation on #15 tooth. The cold test elicited a negative response. Radiographically, the periapical radiolucency of #15 tooth had significantly decreased over the time with complete healing and no symptoms after 12 and 24 months (Figures 4A-4D).
Figure 3: Case 1. Pulp tissues closed with MTA. (A) intraoral radiograph. (B) periapical radiograph taken immediately after placement of MedCem MTA in the root canal at the first treatment visit.

Figure 4: Case 1. Periapical radiographs of follow-up visits. (A) Follow up after 4- months. (B) Follow up after 8- months. (C) Follow up after 12- months; radiolucency disappeared completely. (D) Follow up after 24- months.
Case 2 Presentation
A 16-year-old girl presented the dental clinic of one of the authors (ZG) for an annual observation. Clinical examination revealed a large carious lesion involving the occlusal and distal surfaces of the right mandibular permanent second premolar. The patient had no complaints. The tooth responded positively to the cold test (Cold Spray, Polydent, Germany) and the periapical radiograph was taken to evaluate the depth of the caries process (Figure 5). As the radiograph was taken to evaluate only the depth of the caries and a tooth responded to the pulp sensitivity test positively, the attention was not paid to the quality of the x-ray although the apex of the tooth and surrounding apical periodontium was not seen. After clinical and radiographic examination, #45 tooth was diagnosed with vital pulp. Under dental microscope, rubber dam isolation and local anesthesia with 4% articaine and epinephrine 1:100000 (Ubistesin forte, 3M Science, USA), caries was excavated. The excavation revealed caries lesion reaching the pulp, but the exposed pulp appeared vital, judged by its appearance, bright red color, and not intense bleeding overflowing from the exposure site. Vital pulp therapy (pulpotomy) was a treatment of choice.
After explaining the possible risks of VPT, written informed consent was obtained from the patient’s parents. With a sterile long-shank, high-speed, round diamond bur (Hager & Meisinger, Germany) the pulp tissue at the exposure site was removed till attached vital tissue was observed, and irrigated with 2.5% sodium hypochlorite solution (Cerkamed, Poland). The bleeding was stopped in 2 min. with a cotton pellet soaked in 2,5% sodium hypochlorite (Cerkamed, Poland) within five minutes. A layer of hydraulic calcium silicate cement MedcemMTA (Medcem GmbH, Austria) was applied over the vital pulp tissue. The cement was covered with chemically cured GIC (i-FIL LC, Vita Zahnfabrik H. Rauter GmbH & Co. KG, Germany), following the final restoration with light-cured composite (ONE shade, Olident, Poland). A periapical radiograph was performed immediately after the treatment (Figures 6) and revealed the large apical radiolucency. At the follow-up visits, the patient reported no symptoms. The dental periapical radiographs showed radiolucency considerably reduced in size (Figures 7A & 7B). After one year, no periapical radiolucency was evident on the x-ray, and intact lamina dura was observed (Figure 7C).
Figure 7: Case 2. (A) Three-month follow-up. The lesion size has been reduced. (B) Fourth month follow-up. (C) One-year followup. The bone destruction has healed.

Discussion and Conclusion
The leading cause of pulp inflammation is microorganisms that usually enter the pulp cavity through caries-damaged tooth. The progression of inflammation likely results in pulp necrosis. Nontreated persisting infection in the root canal system can cause a formation of periradicular lesions [18]. Despite the long-standing concept of pulp tissue necrosis as the main etiologic factor for periapical lesions, there has been new evidence that inflamed vital dental pulps can cause apical periodontitis (AP) the same as necrotic pulp does [19]. The first treatment of choice for teeth with chronic AP is root canal treatment (RCT). RCTs have shown high success rates, with a survival rate of 85- 94% after a 4-year follow-up [20]. Although RCTs have shown high success rates, root canal-filled teeth are more susceptible to complications such as postoperative fractures and reinfections [21] as the protective stress-reducing damping effects and mechanoreceptor functions [22] are lost with the removal of the pulp tissue. Hence, the suggestions of vital pulp therapy as a treatment option in cases of irreversible pulpitis (IP) is widely accepted. Asgary S et al. reported that teeth with IP associated with apical periodontitis, treated by VPT, are more successful at 6- and 12-month recalls compared to RCT [23]. The spread of infection could be successfully halted through the implementation of VPT.
It could be hypothesized that if the AP has been caused by inflammation of the pulp, and the pulp is still vital (although it could be inflamed), can the teeth with radiographical signs of AP treated by VPT procedures? Suppose the bleeding tissues are observed during the treatment. In that case, pulpitis is the possible state of the treated tooth [24], and even with radiolucency in radiography, VPT can be considered the treatment of choice. One but not the slightest reason why pulpotomy should be a treatment of choice - nonvital teeth are more likely to be exposed to higher bite force levels because they are deficient in protective mechanosensation [25] - chewing triggers a unique and complex neural control system. This system protects the structure of the teeth. A tooth’s ability to withstand chewing depends on having a complex neural control system to keep the tooth intact. The cornerstone of this neural control system is the intact dental pulp [25]. It must be mentioned that in the first clinical case, the tooth showed a false negative response to the cold test. This clinical case proves information that the current pulp sensitivity tests are unreliable in determining the pulp’s status because the vascular supply is more critical in determining the pulp vitality than the sensory supply. The pulp can only be healed if the circulating blood flow is healthy. Dental clinicians have an urgent need for more definitive tests [26].
It is essential to follow up clinical cases after the VPT. The teeth with a full pulpotomy performed cannot be evaluated with pulp sensitivity tests. The absence of symptoms, clinical and radiographic signs can assume that the radicular pulp remained vital, and the treatment outcome is successful. Radiographically, there should be no signs of internal root resorption, no new periapical pathosis, and healing of previous periapical pathosis should be observed [27]. Two-year follow-up has been considered adequate for MTA pulpotomy because most complications develop precisely during this period [28]. The follow-up period of the second case should be extended to two years to evaluate the treatments’ outcomes. In both clinical cases coronal pulpotomy was a treatment of choice. According to Riccuci et al. (2019), after pulp exposure in deep carries lesion case, inflammation becomes irreversible and mostly confined to the coronal region immediately beneath the carious exposure (typically limited within 2 mm) and removal of the carious and infected dentin is not sufficient to provide a predictable outcome [29]. If the pulp is irreversibly inflamed, it has to be partially or totally removed for improved treatment outcome. As we don’t know the real pulp inflammation status, for better outcomes, in present cases, the part of detached pulp tissues in the coronal part were removed, what showed that they might be inflamed and infected [30]. These case reports represented a successful coronal pulpotomy in symptomatic and asymptomatic teeth with vital pulps associated with periradicular lesions. After 12 and 24 months, the preoperative periradicular lesions healed with a standard periodontal ligament space and lamina-dura re-established. The outcomes of the present cases reports were in consistent with the previous studies [31]. Clinical and radiographic evidence of cases showed the successful use of mineral trioxide aggregate for VPT of mature teeth with vital pulps and signs of apical periodontitis.
Acknowledgments
The authors wish to thank the participating patients and their parents.
Authors’ Contributions
ZG was involved in collecting the clinical data and drafting and writing the manuscript. GL made substantial contributions to the conception and design, analysis, and interpretation of the data and the manuscript revision. Both authors read and approved the final version of the article.
Funding
The author declares that there is no source of funding related to this study.
Availability of Data and Materials
All data is available in the manuscript.
Ethics Approval and Consent to Participate
Informed consent was obtained from the patient’s parents in written form.
Consent for Publication
Written informed consent for the publication of clinical details was obtained from the patient’s parents.
Competing interests
The authors deny any conflicts of interest related to this study.
References
- (2017) American Association of Endodontics. AAE clinical considerations for a regenerative procedure. American Association of Endodontics.
- (2022) American Academy of Pediatric Dentistry. Pulp therapy for primary and immature permanent teeth. The Reference Manual of Pediatric Dentistry. Chicago Ill American Academy of Pediatric Dentistry pp. 415-423.
- Zanini M, Hennequin M, Cousson P (2019) Which procedures and materials could be applied for full pulpotomy in permanent mature teeth? A systematic review. Acta Odontol Scand 77: 541–551.
- Lin LM, Ricucci D, Saoud TM (2020) Vital pulp therapy of mature permanent teeth with irreversible pulpitis from the perspective of pulp biology. Aust Endod J 46: 154–156.
- Demarco FF, Rosa MS, Tarquınio SBC, Piva E (2005) Influence of the restoration quality on the success of pulpotomy treatment: a preliminary retrospective study. J Appl Oral Sci 13: 72–77.
- Kovacević M, Tamarut T, Jonjić N (2008) The transition from pulpitis to periapical periodontitis in dogs' teeth. Aust Endod J 34: 12-18.
- Kimberly CL, Byers MR (1988) Inflammation of rat molar pulp and periodontium causes increased calcitonin gene-related peptide and axonal sprouting. Anat Rec 222: 289-290.
- Zheng J, Wu Z, Niu K (2019) Microbiome of deep dentinal caries from reversible pulpitis to irreversible pulpitis. J Endod 45: 302–309.
- Lima SMF, de Pádua GM, Sousa MGDC (2015) Antimicrobial peptide-based treatment for endodontic infections--biotechnological innovation in endodontics. Biotechnol Adv 33: 203-213.
- He L, Zhong J, Gong Q, (2017) Regenerative endodontics by cell homing. Dent Clin 61: 143–149.
- Stashenko P (1990) Role of immune cytokines in the pathogenesis of periapical lesions. Endod Dent Traumatol 6: 89-96.
- Jancsó N, Jancsó Gábor A, Szolcsányi J (1967) Direct evidence for neurogenic inflammation and its prevention by denervation and by pretreatment with capsaicin. Br J Pharmacol Chemother 31: 138-141.
- Richardson JD, Vasko MR (2002) Cellular mechanisms of neurogenic inflammation. J Pharmacol Exp Ther 302: 839–845.
- De Swert KO, Joos GF (2006) Extending the understanding of sensory neuropeptides. Eur J Pharmacol 533: 171-181.
- Lundy FT, Linden GJ (2004) Neuropeptides and neurogenic mechanisms in oral and periodontal inflammation. Crit Rev Oral Biol Med 15: 82–88.
- Yamasaki M, Kumazawa M, Kohsaka T (1994) Pulpal and periapical tissue reactions after experimental pulpal exposureinrats. J Endod 20: 13-17.
- Stashenko P, Wang CY, Riley E (1995) Reduction of infection-stimulated periapical bone resorption by the biological response modifier PGG glucan. J Dent Res 74: 323-330.
- Möller AJ, Fabricius L, Dahlén G (1981) Influence on periapical tissues of indigenous oral bacteria and necrotic pulp tissue in monkeys. Scand J Dent Res 89: 475–484.
- Asgary S, Kemal Çalışkan M (2015) Vital pulp therapy of a mature molar with concurrent hyperplastic pulpitis, internal root resorption and periradicular periodontitis: a case report. Iran Endod J 10: 284–286.
- Sjögren U, Figdor D, Persson S, Sundqvist G (1997) Influence of infection at the time of root filling on the outcome of endodontic treatment of teeth with apical periodontitis. Int Endod J 30: 297–306.
- Moussa DG, Aparicio C (2019) Present and future of tissue engineering scaffolds for dentin-pulp complex regeneration. J Tissue Eng Regen Med 13: 58-65.
- Sadaf D (2020) Success of Coronal Pulpotomy in Permanent Teeth with Irreversible Pulpitis: An Evidence-based Review. Cureus 12: 6747.
- Asgary S, Eghbal MJ, Ghoddusi J, Yazdani S (2013) One-year results of vital pulp therapy in permanent molars with irreversible pulpitis: an ongoing multicenter, randomized, non-inferiority clinical trial. Clin Oral Investig 17: 431-439.
- Levy JH (2009) Teeth as sensory organs. Inside Dent 2: 1–9.
- Taha NA, About I, Sedgley CM, Messer HH (2020) Conservative Management of Mature Permanent Teeth with Carious Pulp Exposure. J Endod 46: 33-41.
- Duncan HF, Galler KM, Tomson PL (2019) European Society of Endodontology position statement: management of deep caries and the exposed pulp. Int Endod J 52: 923-933.
- Simon S, Perard M, Zanini M (2013) Should pulp chamber pulpotomy be seen as a permanent treatment? some preliminary thoughts. Int Endod J 46: 79-87.
- Ricucci D, Siqueira JFJr, Li Y, Tay FR (2019) Vital pulp therapy: histopathology and histobacteriology- based guidelines to treat teeth with deep caries and pulp exposure. J Dent 86: 41-52.
- Rivucci D, Loghin S, Siqueira JFJr (2014) Correlation between Clinical and Histologic Pulp Diagnoses. J of Endodontics 40: 1932-1939.
- Asgary S (2011) Calcium-enriched mixture pulpotomy of a human permanent molar with irreversible pulpitis and condensing apical periodontitis. J Conserv Dent 14: 90-93.
- Asgary S, Nosrat A, Homayounfar N (2012) Periapical healing after direct pulp capping with calcium-enriched mixture cement: a case report. Oper Dent 37: 571-575.
Editorial Manager:
Email:
pediatricdentistry@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...







