Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6636
Review Article(ISSN: 2637-6636) 
Periodontal Infections in Children Volume 4 - Issue 5
Satarupa Bhattacharyya1 and Sayan Bhattacharyya2*
- 1BDS, Dental Surgeon, Kolkata
- 2Assistant Professor, Microbiology, All India Institute of Hygiene and Public Health (AIIH&PH), India
Received: September 22, 2020; Published: September 29, 2020
*Corresponding author: Sayan Bhattacharyya, Assistant Professor, Microbiology, All India Institute of Hygiene and Public Health (AIIH&PH), Kolkata, India
DOI: 10.32474/IPDOAJ.2020.04.000197
Abstract
Periodontal infections are very common in children and should be properly diagnosed and treated after obtaining proper history. They can arise due to multiple factors, of which an important role is played by various bacteria. Familial and genetic factors are also important. Timely treatment is essential for best outcome. In this review article authors have tried to summaries available information about the condition.
Keywords:Periodontal disease; infection; gingivitis; plaque
Introduction
In medical dictionaries, the word periodontium is said to be derived from the Greek term’s peri-, which means “around,” and -odons, which means “tooth.” Hence, literally, it means that which is around the tooth. Periodontium includes the tissues that surround and support the teeth. Those tissues are gingiva, cementum, periodontal ligaments, and alveolar bone [1]. Periodontal diseases consist of a group of conditions that are considered nowadays ubiquitous among children, adolescents, and adults [2] . The term “periodontal diseases” includes any inherited or acquired disorders of the tissues that are investing and supporting the teeth (gingiva, cementum, PDL, and alveolar bone) [2]. Another researcher defined periodontal diseases as chronic infectious disorders caused primarily by bacteria . Also, destructive forms or type of lesions are lesser in younger children than older children or adults [3]. Children and adolescents can have any of the several forms of periodontitis as discussed in the proceedings of the 1999 International Workshop for a Classification of Periodontal Diseases and Conditions (like aggressive periodontitis, chronic periodontitis, and periodontitis as a manifestation of systemic diseases) [3]. However, aggressive periodontitis is more commonly seen in younger children and chronic lesions in younger children [3].
Classification and Types
An up-to-date classification of the periodontal diseases allows
the clinician to consider the full range of periodontal disorders that
can affect the patient and provides a basis for their diagnosis and
subsequent management [4]. Hence, nowadays researchers classify
the following types of periodontitis in children:
a) Gingival diseases, Plaque-induced gingivitis, Gingival
diseases associated with dental plaque only (without/with
local factors which predispose to plaque retention), Gingival
diseases modified by systemic factors, Gingival diseases
modified by medications, Gingival diseases modified by
malnutrition, Non-plaque induced gingival lesions, including:
those of specific bacterial, viral, fungal or genetic origin;
lesions of systemic conditions; traumatic lesions or foreign
body reactions
b) Chronic periodontitis.
c) Aggressive periodontitis.
d) Periodontitis as a manifestation of systemic diseases,
associated with hematological disorders, Associated with
genetic disorders.
e) Necrotising periodontal diseases, Necrotising ulcerative
gingivitis, Necrotising ulcerative periodontitis.
f) Abscesses of the periodontium, Gingival abscess,
Periodontal abscess, Peri coronal abscess
g) Periodontitis associated with endodontic lesions.
h) Developmental or acquired deformities and conditions,
Localised tooth-related factors that modify or predispose to
plaque-induced gingival diseases/periodontitis, Mucogingival
deformities and conditions around teeth, including gingival
recession and gingival overgrowth, Mucogingival deformities
and conditions on edentulous ridges
i) Occlusal trauma
Gingivitis in children
Gingivitis of varying severity is found very commonly in children and adolescents [3]. Gingivitis was added as a new category of periodontal infections in 1999. Plaque-induced gingivitis is common in young as well as older age groups and modifying factors can be identified from the history and examination that can influence the natural course and management [4]. Plaque displays typical properties of biofilms or microbial communities ; the plaque ecology is a very important determinant in disease development [5]. People now opine that gingivitis may be more important than previously thought. From the Fifth European Workshop in Periodontology in 2005, it was concluded that gingivitis and periodontitis are an extension of the same broad inflammatory disease [6]. However, there is a wide range in individual susceptibility and not all individuals with gingivitis will progress to destructive periodontitis. It is also significant that the terminology has changed from ‘adult periodontitis’ to ‘chronic periodontitis’ because this highlights the increased international awareness that periodontitis is not just confined to adults over the age of 35 years, but can begin in early teenage years and progress slowly throughout the teens [6,7]. A subgingival calculus, smoking and Diabetes mellitus are plausible predisposing factors (6). A diverse microbial flora can be found in the subgingival plaques in this condition, and a bacterium, Tannerella forsythensis has been significantly associated with loss of attachment and the conversion of periodontally healthy sites to diseased sites over a three year period in adolescents, in a study [8].
Aggressive periodontitis
The term ‘ Early onset periodontitis’ is now replaced with ‘Aggressive periodontitis’. It is a rapidly developing disease with family history, and mainly occurs in people lesser than 30 years [6]. Aggressive periodontitis can be localized or generalized. Localized aggressive periodontitis (LAgP) patients have interproximal attachment loss on at least two permanent first molars and incisors, with attachment loss on no more than two teeth other than first molars and incisors. Generalized aggressive periodontitis (GAgP) patients show generalized interproximal attachment loss including at least three teeth that are not first molars and incisors [3]. LAgP occurs in children and adolescents without clinical evidence of systemic disease and is characterized by the severe loss of alveolar bone around permanent teeth. Linkage studies of the Brandywine population (a segregated group of people in Maryland that represents a relatively closed gene pool) have found a gene conferring increased risk for LAgP on chromosome 4 [3]. A number of functional defects have been reported in neutrophils from patients with LAgP. These include anomalies of chemotaxis, phagocytosis, bactericidal activity, superoxide production, FcgIIIB (CD16) expression, leukotriene B4 generation, and Ca2+–channel and second messenger activation [3]. The defect in chemotaxis is considered to be an intrinsic defect by some investigators.
Plaque associated gingivitis
In children, the most common form of infection belonging to the classification of periodontal disease, is plaque-associated gingivitis , which is usually reversible when the plaque is removed but, in a few cases, leads to a more serious teeth destruction with bone loss [9]. Chronic gingivitis is common in children. It usually causes gum tissue to swell, turn red and bleed easily. Gingivitis is both preventable and treatable with a usual routine of brushing, flossing and professional dental care in children. However, if left untreated, it can finally progress to more serious forms of periodontal disease [10].
Microbial aetiology
Microbial dental plaque and the presence of periodontal pathogens are required for the beginning of periodontal disease, but the host defense mechanism is also an important factor that affects the progression and severity of periodontitis in individuals affected by systemic diseases [6]. Some of the periodontal pathogens present in periodontal pockets in children are Actinobacillus actinomycetemcomitans, Prevotella intermedia, Eikenella corrodens and Capnocytophaga sputigena [11]. Aggressive form of periodontal infection with tooth loss is uncommon in children, and generally indicates a systemic illness [11]. Such diseases are usually hematological and genetic disorders. The types of hematological disorders are:
a) Acquired neutropenia
b) Leukemias
c) Other
The types of genetic disorders are:
a) Familial and cyclic neutropenia
b) Down syndrome
c) Leukocyte adhesion deficiency syndrome
d) Papillon-Lefèvre syndrome
e) Chédiak-Higashi syndrome
f) Histiocytosis syndromes
g) Glycogen storage disease
h) Infantile genetic agranulocytosis
i) Cohen syndrome
j) Ehlers-Danlos syndrome (Types IV and VIII)
k) Hypophosphatasia
l) Others.
Pathogenesis of periodontitis
Dental plaque in LgAP has predominantly A actinomycetemcomitans ,releasing virulence factors like leukotoxin, lymphocyte suppression factor, fibroblast and keratinocyte inhibitor, collagenase, and lipopolysaccharides [12]. P gingivalis also has host specific proteases called gingipains that causes its virulence [12]. In CP (Chronic periodontitis) and GAgP, the plaque bacteria are more in variety and diversity, and consists of P gingivalis, P intermedia, T forsythia, Eubacterium sp and F nucleatum [12]. Generalized AP shows equal number of A actinomycetemcomitans, Campylobacter rectus, and Spirochetes [13]. The serum level of antibody IgG2 reactive against A. actinomycetemcomitans is generally higher in LAP than in GAP and CP patients [12]. Hence the bacterium definitely plays a role. Gingival problems that are commonly seen in children and adolescents, and their pathogenesis are as follows:
Eruption Gingivitis: Some gingival inflammation normally accompanies eruption process . Poor oral hygiene by neglect or as a consequence of malalignment of the erupting teeth will aggravate gingival inflammation . Usually, the condition will subside as the oral hygiene improves and the tooth reaches normal occlusion . Plaque control regimen is the treatment of eruption gingivitis [14].
Pubertal Gingivitis: Pubertal gingivitis , which is also called steroid hormone-related gingivitis is defined as exacerbation of gingivitis by fluctuation in gonadotrophic hormone levels during puberty . A similar condition is seen during pregnancy and in females taking contraceptives. The phenomenon of this condition can be explained as any increase in the levels of oestrogen and progesterone in the gingival tissues resulting in vasodilatation and proliferation, increase in gingival vascularity, and increase in susceptibility of inflammation in the presence of local factors [14].
Acute necrotising ulcerative gingivitis is somewhat rare in children. It is illustrated in Figure 2. Generalized Aggressive periodontitis is highlighted in Figure 3.
Diagnosis
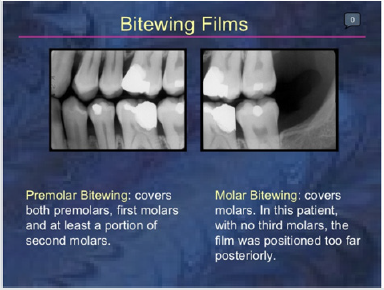
Diagnosis of periodontitis in children is mainly clinical based on appearance of lesions and family illness. However, radiographic investigation should be performed when it is clinically required iand affects patient prognosis and management [12]. Although panoramic radiography gives important information on unerupted permanent and missing teeth, the alveolar bone levels are best assessed and viewed by intraoral periapical and Bitewing radiography [12]. Figure 1 illustrates Bitewing radiograph.
Treatment
Plaque control program can be planned based on the chronological age and manual dexterity of the child and can be done by caregiver if necessary [12]. Scrub technique of tooth-brushing technique has been found to be useful in children, but the modified Bass technique can be taught to adolescents with expertise [15]. Periodontal lesions predominantly are interdental, and older individuals can be advised use of interdental cleaning aids [16]. Nowadays, Triclosan with copolymer and dentifrices containing Fluoride have been documented to significantly reduce attachment loss in adolescents aged 11–13 years [12]. Keyes’s technique involving a paste of baking soda, salt, and hydrogen peroxide as a dentifrice and subsequent irrigation with saturated salt solution carried out with a regimen of tetracycline hydrochloride orally, is old and has been prescribed to patients having AgP ;it has shown good results also [17]. Scaling and root planning can definitely reduce microbial load and bring down Cytokine levels, but not in Aggressive periodontitis where motile bacteria are involved and recolonization with reinfection is very common [12,18]. Systemic antibiotics are indicated where A. actinomycetemcomitans is involved and recolonization occurs very frequently. The dosage should be adjusted as per the child’s weight and age. As per adult doses and individuals weighing 40 kg and more, Tetracycline in 250 mg qid and doxycycline in 100 mg od doses have the ability to concentrate in the gingival crevice fluid and inhibit the growth of A. actinomycetemcomitans. It exhibits anticollagenase effect also, which can thereby inhibit tissue destruction and aid in bone regeneration.
Maintenance
Periodic review is essential to prevent recurrences in such cases, especially AgP (20). Qualitative chair side diagnostic aids for guessing the risk for future attachment loss for severe cases of CP and AP consists of the use of chair-side assays such as ELISA for detecting the presence of A. Actinomycetemcomitans, P. gingivalis and P. intermedia in plaque samples, and Benzoyl-DLarginine- napthylamide assay for trypsin and other end products of proteolytic enzymes in plaque samples containing P. gingivalis, T. forsythia, and Treponema denticola . X ray can also be required for assessment and review.
Discussion
CP usually has a slower progression rate and a better prognosis . It responds to therapy better ,as compared to AgP [12]. Considering the multifactorial aetiology and predisposing factors that lead to the development of AgP in the susceptible host, special care needs to be taken that all facets affecting the diagnosis and therapeutic outcomes are addressed well [12]. AgP affects young individuals with early loss of teeth which influences quality of life. Early diagnosis with meticulous therapeutic intervention and monitoring of the child and adolescent is therefore advised with thorough periodontal examination and early intervention [12].
Conclusions
Periodontitis is very common in children. Knowledge of the different types of periodontitis is optimal for correct diagnosis and therapy.
References
- Hayat Al-Ghutaimel, Hisham Riba, Salem Al-Kahtani, Saad Al-Duhaimi (2014) Common Periodontal Diseases of Children and Adolescents. International Journal of Dentistry 2014(1): 850674.
- Oh TJ, Eber R, Wang HL (2002) Periodontal diseases in the child and adolescent,” Journal of Clinical Periodontology 29(5): 400–410.
- Joseph VC, Research, Science and Therapy Committee Guidelines of the American Academy of Periodontology (2003) Periodontal Diseases + of Children and Adolescents. J Periodontol 74(11): 1696-1704.
- Clerehugh V (2008) Periodontal diseases in children and adolescents. Br Dent J 204(8): 469–471.
- Marsh PD (2005) Dental plaque: biological significance of a biofilm and community lifestyle. J Clin Periodontol 32(Suppl 6): 7–15.
- Kinane DF, Attstrom R (2005) Advances in the pathogenesis of periodontitis. Group B consensus of the fifth European workshop in periodontology. J Clin Periodontol 32(Suppl 6): 130–131.
- Clerehugh V, Lennon M A, Worthington H V (1990) 5-year results of a longitudinal study of early periodontitis in 14- to 19-year-old adolescents. J Clin Periodontol 17: 702–708.
- Hamlet S, Ellwood R, Cullinan M (2004) Persistent colonisation with Tannerella forsythensis and loss of attachment in adolescents. J Dent Res 83: 232–235.
- Vagdouti T, Tsilingaridis G. Periodontal Diseases in Children and Adolescents Affected by Systemic Disorders - A Literature Review. Gum disease in children 4: 55.
- Kini V, Patil RU, Pathak S, Prakash A, Gupta B (2016) Diagnosis and management of periodontal disease in children and adolescents: A brief review. J Dent All Sci 5(2): 78-83.
- Schenkein HA, Van Dyke TE (1994) Early-onset periodontitis: Systemic aspects of etiology and pathogenesis. Periodontol 2000 6: 7-25.
- Al- Ghutaimel H, Riba H, Al- Kahtani S, Al- Duhaimi S (2014) Common Periodontal Diseases of Children and Adolescents. Int J Dent 2014: 850674.
- Clerehugh V, Tugnait A (2001) Diagnosis and management of periodontal diseases in children and adolescents. Periodontol 2000 26: 146-168.
- Kinane DF (1998) The role of interdental cleaning in effective plaque control: Need for interdental cleaning in primary and secondary prevention. Lang NP, Attström R, Löe H (Eds.), Proceedings of the European Workshop on Mechanical Plaque Control, Quintessence, Chicago, USA pp. 156-68.
- Keyes PH, Wright WE, Howard SA (1978) The use of phase-contrast microscopy and chemotherapy in the diagnosis and treatment of periodontal lesions – An initial report (I). Quintessence Int Dent Dig 9: 51-56.
- Renvert S, Wikström M, Dahlén G, Slots J, Egelberg J (1990) Effect of root debridement on the elimination of Actinobacillus actinomycetemcomitans and Bacteroides gingivalis from periodontal pockets. J Clin Periodontol 17: 345-350.
- Gordon JM, Walker CB, Murphy JC, Goodson JM, Socransky SS (1981) Concentration of tetracycline in human gingival fluid after single doses. J Clin Periodontol 8(2): 117-121.
- Deas DE, Mealey BL (2010) Response of chronic and aggressive periodontitis to treatment. Periodontol 2000 53: 154-166.
Editorial Manager:
Email:
pediatricdentistry@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...