Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6636
Review Article(ISSN: 2637-6636) 
A Study on the Importance and Performance of Covid Infection Control in Dental Hygienists Volume 7 - Issue 4
Hee Ja Na1* and Shijunfan2
- 1Department of Dental Hygiene, Honan University, Kwangju, Korea
- 2Graduate of Dental Hygiene, Honan University, Kwangju, Korea
Received: April 25, 2022; Published: May 13, 2022
*Corresponding author: Hee Ja Na, Department of Dental Hygiene, Honan University, Kwangju, 62399, Korea
DOI: 10.32474/IPDOAJ.2022.07.000269
Abstract
Objective: This study analyzes the importance and performance of dental hygienists for Covid infection management. It is intended to increase the clinical performance for Covid infection management by dental hygienists and to provide basic data for blocking coronavirus.
Methods: In order to understand the general characteristics of the subjects in this study, mean and standard deviation were obtained, and a variance analysis of job type and covid importance was performed, and an anova-test of covid importance and performance, and multiple regression analysis was analyzed at a significance level of 0.05.
Results: There were 172 subjects for this study; their general characteristics were gender, age, education level, position, number of patients cared for per day, training to treat covid infected patients, necessary level of covid infection education, and method of covid education. The results based on covid cause characteristics, covid dental hygiene, covid prophylaxis, personal protective gear, how to use equipment infected by patients, room aerosol management, personal hygiene, and covid therapy communication were not significant; the average and standard deviation for general dental hygienists in medical waste was 4.024 (1.088). The average and standard deviation for the chief dental hygienist is 3.678 (8.855), the average and standard deviation for the part-time dental hygienist is 3.529 (8.895), f=3.850, p=. As 023, and there is a significant difference at the significance level of 0.05. The p value of the performance of the Covid- cause characteristic was .013, showing a significant difference at a significance level of .05. The degree of performance for medical waste is also p=.008, which is a significant level. There is a significant difference in 05 and the personal hygiene performance is p=as 024. There is a significant difference at the significance level of .05. In the correlation analysis, the importance of covid prevention behavior, personal protective equipment, clinic aerosol importance, personal hygiene importance, covid dental hygiene treatment performance, covid prevention behavior performance, clinic aerosol performance, and personal hygiene performance are highly correlated. In addition, the significance level result for testing the significance in multiple regression analysis for covid importance and dependent variable performance based on individual independent variables, which were determined from the number of patients’ nursing per day was affected satisfactorily with a 05 Independent variable for Covid preventive action performance (t=-2.834, p=.05); Aerosol performance in the clinic (t=3.042, p=.003) has a significant effect.
Conclusion: The average and standard deviation for general dental hygienists in medical waste materials is 4.024 (1.088), The average and standard deviation of the chief dental hygienist is 3.678 (.855) The mean and standard deviation for part-time dental hygienists is 3.529 (8.895), f=3.850, p=.As 023, there is a significant difference at the significance level of 0.05. There is a significant difference in the Anova test between the performance of the characteristics of the covid cause, the performance of medical products, and personal hygiene. In addition, as a result of testing the significance of heavy regression analysis for the number of patients nursing per day along with the importance of covid prevention performance, the degree of covid prevention behavior at a significance level of .05 (t=-2.834, p=).005), room aerosol performance (t=3.042, p=.003) has a significant effect.
Keywords: Infection control; dental occupation; coronavirus-19; dental hygienist; dental clinic; performance; care work
Introduction
According to the recent announcement, dental institutions are paying attention to the very high risk of infection due to the emergence of COVID-19 infections [1]. Dental hygiene is a study of theory and practice, and by acquiring knowledge and skills to become a professional dental hygienist and learn how to apply these skills clinically, hygienists seek to connect theory and practice in patient management and treatment for the dental profession. Dental clinics are always exposed to a wide range of pathogenic microorganisms, and secretions such as blood, saliva, and body fluids, as well as large amounts of aerosol and dust generated during dental treatment can contaminate the interior of dental clinics [2]. Dental care has a high risk of transmission of infectious diseases because the operator, patient, and assistant are within close lines of movement [3]. Infection control measures should be prepared to ensure the safety and health rights of patients and dental workers in dental clinics. Accordingly, in 2006, the Ministry of Health and Welfare worked to prevent infection by preparing sterilization and handling methods for dental materials, medical equipment, and equipment used in dental clinics to prevent cross-infection between patients and medical staff [4]. With the revision of the 2010 Medical Act, the certification criteria for dental hospitals were presented according to the medical institution certification system, and since 2014, infection control for dental hospitals was included, and infection control was divided into three categories [5].
Hospital infection management is used as an important indicator of the quality of medical care along with safety care and should be understood and approached as a basic process of providing quality medical services. In addition, infection control in medical institutions affects medical consumers’ willingness to revisit and is directly linked to patient satisfaction and increased confidence in medical institutions [6]. However, the hassle of preventing infection in the dentist’s office and the lack of time due to the extension of treatment time lowered the infection control practice rate [7], and the cost of infection control was linked to an increase in treatment costs, making it difficult to actively manage infection. In addition, the certification evaluation system is limited to dental hospitals, so regulations on infection control evaluation at dental clinics are still insufficient, and the infection control status varies from medical institution to medical institution depending on the environment or dental worker’s perception and willingness to practice. Infection control can be effective when both medical staff, patients, institutional managers, and infection managers recognize and practice its importance [8]. Recently, basic knowledge has become common through access to the media and educational materials on the risks caused by COVID-19 and the need to prevent infection. However, as clinical practice with a high risk of infection has been suspended, dental hygienists in the first year after graduating from the Department of Dental Hygiene are emerging to address the very urgent issue of strengthening dental clinics infection control education capabilities.
In a study comparing the clinical practical ability of first-year dental hygienists’ infection control education program, according to previous studies applying online non-face-to-face infection control curricula, the dental worker’s performance confidence was improved due to high accessibility and the advantage of repetitive learning [9]. COVID-19 clinical symptoms include fever (over 37.5°C), cough, shortness of breath, chills, muscle pain, headache, sore throat, loss of smell and taste, or pneumonia, fatigue, decreased appetite, phlegm, digestive symptoms (such as nausea, vomiting, diarrhea), confusion, runny nose or nasal congestion, blood, chest pain, conjunctivitis, and skin symptoms. In addition, when a patient complaining of these symptoms visits the dentist, the following response steps are provided. First, wear a mask, and when coughing or sneezing, try not to face people, and when coughing or sneezing without a mask, cover your mouth and nose with a tissue, throw away used tissue in the trash, and if there is no tissue, use a clothes sleeves. After each patient’s treatment, disinfect the surface that the patient has contacted. After using an aerosol generation procedure for all patients, disinfect and ventilate the patient treatment area after completion, and then treat other patients. Drawers and cabinets in the clinic must be covered and placed far away so that droplets or aerosols are not contaminated by splashing. If not used during the procedure but exposed, all consumables and equipment are considered contaminated and disposed or reprocessed appropriately.
If a patient is suspected of COVID-19, dental treatment is postponed and the following measures are taken. Have the patient wear a mask and transfer the patient to an empty space in the clinic). If the patient does not have severe symptoms, send the patient home and guide them to receive screening treatment. It is necessary to accurately identify infected patients and block the infection route, which is practically impossible. Therefore, a system for preventing infection should be applied throughout the treatment so that all patients can be prepared under the assumption that they have an infectious disease [9]. Medical institution management with COVID-19 confirmed cases requires medical staff in contact with confirmed or suspected patients to select and wear appropriate personal protective gear, i.e. full-body suit or long-sleeved gown, disposable gloves, KF94 or above, mask, goggles, or face protective gear, depending on the situation. Medical staff transporting COVID-19 confirmed or suspected patients should wear hand hygiene and personal protective equipment (full body protective clothing, disposable gloves, KF94 or masks of the same level or higher), and goggles or facial protective equipment should be worn if the patient has severe respiratory symptoms such as cough and phlegm. If emergency dental treatment is required for a confirmed or suspected COVID-19 patient, the personnel participating in the treatment should wear personal protective equipment, that is, fullbody protective clothing, disposable gloves, KF94 or masks of the same level or higher according to the guidelines. Dental treatments are provided in individual closed spaces where possible. If possible, avoid using handpieces, 3-way syringe, and ultrasonic scalers as aerosol-producing procedures.
It is preferable that the aerosol generation procedure is performed in a negative pressure isolation room. Dental treatment is limited to essential treatment, and participating medical personnel are also limited to essential personnel. The patient considers making an appointment as the last schedule during the treatment time. During the patient’s treatment, other patients are not treated together. If there is a possibility of contact with blood or body fluids, mucosa, damaged skin, or contaminated skin, wear gloves and use them for disposable use. When wearing gloves, take them off immediately after use, and replace them for each patient. After removing the gloves, perform hand hygiene immediately. If contact with blood, body fluids, secretions, and exudates is expected, wear a suitable gown for work to protect the skin and prevent contamination of the clothes. Wear a disposable vinyl apron when there is a risk of exposure of clothing to blood, body fluids, secretions and exudates in treating patients, and a longsleeved waterproof gown if fluids can splatter widely. Hand hygiene is performed by taking off your gown before leaving the patient’s surroundings or hospital room. Disposable aprons or gowns are changed for each procedure or patient. Select appropriate personal protective gear according to treatment, procedure, and activity. When using personal protective equipment, observe proper steps in wearing and take off. Following their use, the equipment should be properly collected to prevent outsiders from being exposed from personal protective clothing. If there is a possibility of contact with blood or body fluids, mucosa, damaged skin, or contaminated skin, wear gloves and use them for disposable use. When wearing gloves, take them off immediately after use, and replace them for each patient.
After removing the gloves, perform hand hygiene immediately. If contact with blood, body fluids, secretions, and exudates is expected, wear a suitable gown for work to protect the skin and prevent contamination of the clothes. Wear a disposable vinyl apron when there is a risk of exposure of clothing to blood, body fluids, secretions and exudates in treating patients, and a long-sleeved waterproof gown if fluids can splatter widely. Take off your gown and perform hand hygiene before leaving the patient’s surroundings or hospital room. Change disposable aprons or gowns for each procedure or patient. Treatment equipment and instruments shall be disinfected after use in accordance with the manufacturer’s recommended instructions using approved disinfectants from the licensing authority. Use disposable appliances or articles if possible. Treatment instruments for patients contaminated with blood, body fluids, secretions, and excrement are handled to prevent skin or mucosal exposure and contamination of clothing, or the spread of pathogens to other patients and the environment. Reused appliances shall be properly cleaned and disinfected for other patients, and reprocessing methods shall be in accordance with the type, use, manufacturer’s recommendation, hospital guidelines or regulations, and disposable disposables shall be discarded after use. The equipment cleaning staff shall wear personal protective gear when cleaning. Check the disinfectant manufacturer’s recommendations and thoroughly comply with the recommended criteria such as the disinfectant dilution and application time, the duration of the disinfectant validity, and the effective concentration. Waste disposal shall be governed by the medical waste disposal regulations. Waste is treated separately from the place of origin for proper and safe handling. Sharp tools, such as needles and blades, shall be collected in non-piercing waste-only containers, and containers shall be placed where the articles are used. Solid, non-sharp infectious wastes are collected in a waste container that does not open and remains closed. The patient’s bodily fluids or excrement are disposed of in the sewage system in accordance with the sewage discharge regulations. However, care should be taken not to contaminate the surrounding environment or humans in the process of disposing of body fluids or excrement [10].
The Ministry of Health and Welfare of Korea announced infection control rules in 1992, began national measures for hospital infection monitoring, and identified the incidence rate and infection control status of domestic hospitals [11]. In the early 2000s, when there were no dental infection control standards, the Ministry of Health and Welfare announced the prevention standards for dental infections in 2006 and the safety of patients through infection control [12-14]. While this effort continues [15] with the certification evaluation being conducted for dental institutions, based on the certification tool, hygiene recognition and practice, medical waste disposal and the environment, as well as [16] the management status of other specific items, such as wearing personal protective gear being investigated [17]. Along with these, the concept of infection prevention should be applied based on the design of the structure of each clinic, with it being necessary to recognize and prevent the movements that contribute to cross-infection of each patient every day after treatment [18,19]. Dental clinics are contaminated with large amounts of aerosol and dust produced by tooth deletion, prosthetics production, intraoral surgery, and scaling. Therefore, it is necessary to partition treatment space considering the treatment path and contamination occurrence and manage the environment and facilities with cleaning and ventilation. It will also be necessary for dental institutions to investigate the importance of infection management through unit chair management and water pipe management by occupation, gender, and position [20-22]. The purpose of this study was to provide basic data for effective and practical infection control guidelines for dental care by identifying the actual status of dental infection control, and the importance and performance of dental infection control.
Materials and Methods
This study conducted a research survey on 172 first-year dental hygienists working at Y Dental Clinic, S Dental Hospital, L Dental Hospital, and J Dental Hospital in Gwangju Metropolitan City from May 1 to May 30, 2022. Participants in this study were surveyed by dental hygienists who tested negative after contacting COVID-19 confirmed patients. Survey participants agreed to understand the purpose of the study and participate in the study, and the survey was conducted in a self-fill manner. This study was conducted with the consent of the IRB (NO1041223-HR-04) at Honam University’s Bio Science Ethics Committee. When the sample is selected based on the general significance level of .05 and the effect size of 0.3 power of 0.95, using the G-power 3.1 program, the appropriate number of samples is 172. The questionnaire was measured on the Likert 5-point scale, and 5 points were given to the Likert 5-point scale of ‘very important’ and 1 point to ‘not important at all’, meaning that the higher the score, the higher the practicality. The questionnaire was used by revising and supplementing the importance and performance questionnaire of infection control such as Bae and Askarian [23,24].
Research tool
Using 9 sub-factors of Covid infection management importance, and as guidelines for infection prevention, the questionnaire was prepared based on dental treatment infection prevention standards (Ministry of Health and Welfare, 2022) [25] and Askarian [23] and measured on a Likert 5-point scale, and Cronbach’s alpha was 0.812 as a total question. The first-year dental hygienist’s performance of Covid infection control was also completed with dental treatment infection prevention standards (Ministry of Health and Welfare, 2022) [25] and Askarian [23] to identify 9 sub-factors, and measure these on a Likert 5-point scale; Cronbach’s alpha was 0.767.
Analysis method
The data collected in this study were analyzed using the SPSS 21.0 program. The mean and standard deviation were obtained to understand the general characteristics of the subjects, and gender, age, degree of education, position, number of daily patients, education experience for Covid-infected patients, and necessity of education for Covid-infected patients. Technical statistics on the importance of covid dental hygiene treatment according to age, Anova analysis of covid importance, occupation and covid importance variance analysis, covid infection education and covid performance variance analysis were done along with Anova test, covid importance and performance analysis being performed.
Results
General characteristics of subjects
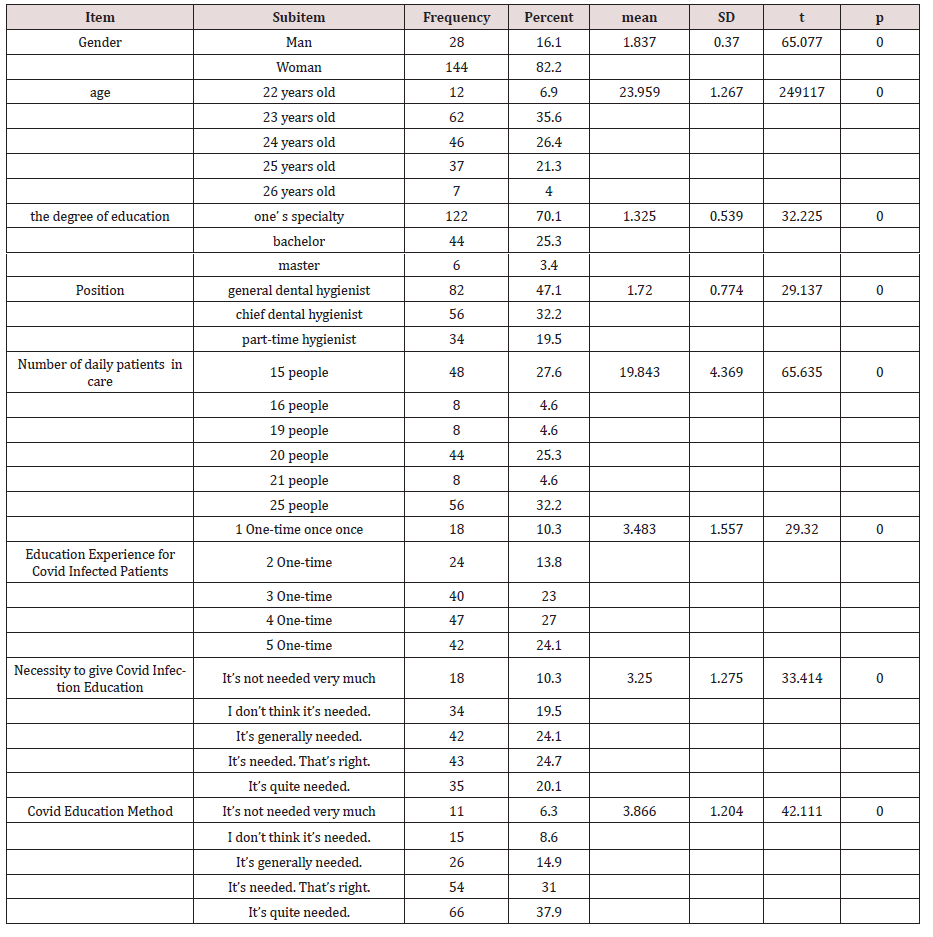
In the general characteristics of 172 subjects in Table 1, 28 16.1% were men, 144 82.2% were women, the average and standard deviation is 6.9% for 22 years olds, 35.6% for 23 years olds, 26.4% for 24 years olds, 21.3% for those 37 years old, 4.0% for those 26 years old, and 23.959 (1.267 = p.0011, p.970. For degree of education: 122, 70.1% had professional bachelors; 44, 25.3% had bachelors; 6, 3.4% had masters. The average and standard deviation is 1.325(5.539), t=32.225, and p=.00. Positions included 82 general dental hygienists with 56, 47.1% being chief dental hygienists; 44, 32.2% being part-time dental hygienists with a 19.5% average and standard deviation being 1.720 (7.774), t=29.137, p=.000. In the frequency of patient care, 15 practitioners treated 48 patients 27.6%; 16 practitioners treated 8 patients 4.6%; 19 practitioners treated 8 patients 4.6%; 20 practitioners treated 44 patients 25.3%; 21 practitioners treated 8 patients 4.6%; 25 practitioners treated 56 patients 32.3%; and the mean and standard deviation for these surveyed was 19.843 (4.369), t=65.635, p=.000. In the experience of staff training to treat patients with covid infection, 18.3% were trained 1 time; 24 staff, 13.8% were trained 2 times; 40 people 23.0% were trained 3 times; 47 people 27.0% were trained 4 times; 42 people 24.1% were trained 5 times; the mean and standard deviation was 3.483 (1.557), t=29.320, and p=.000. On priority for covid education, 18 people 10.3% responded it was not needed very much; 34 people 19.5% responded it’s not needed; for those responding covid education is needed, 42 people 24.1% said it’s usually needed; 43 people 24.7%, responded it’s very needed, and 35 people 20.1% said it’s quite needed. For these survey responses the mean and standard deviation is 3.250 (1.275), t = 33.414. It is 000. In the Covid education method, 11 people 6.3% answered it’s not needed very much; 15 people 8.6% answered it’s not needed; 26 people 14.9% answered yes it’s needed; 54 people 31.0% answered it’s needed very much; 66 people 37.9% answered it’s quite needed. The mean and standard deviation for these responses is 3.866 (1.204), t=42.111, and p=0.000.
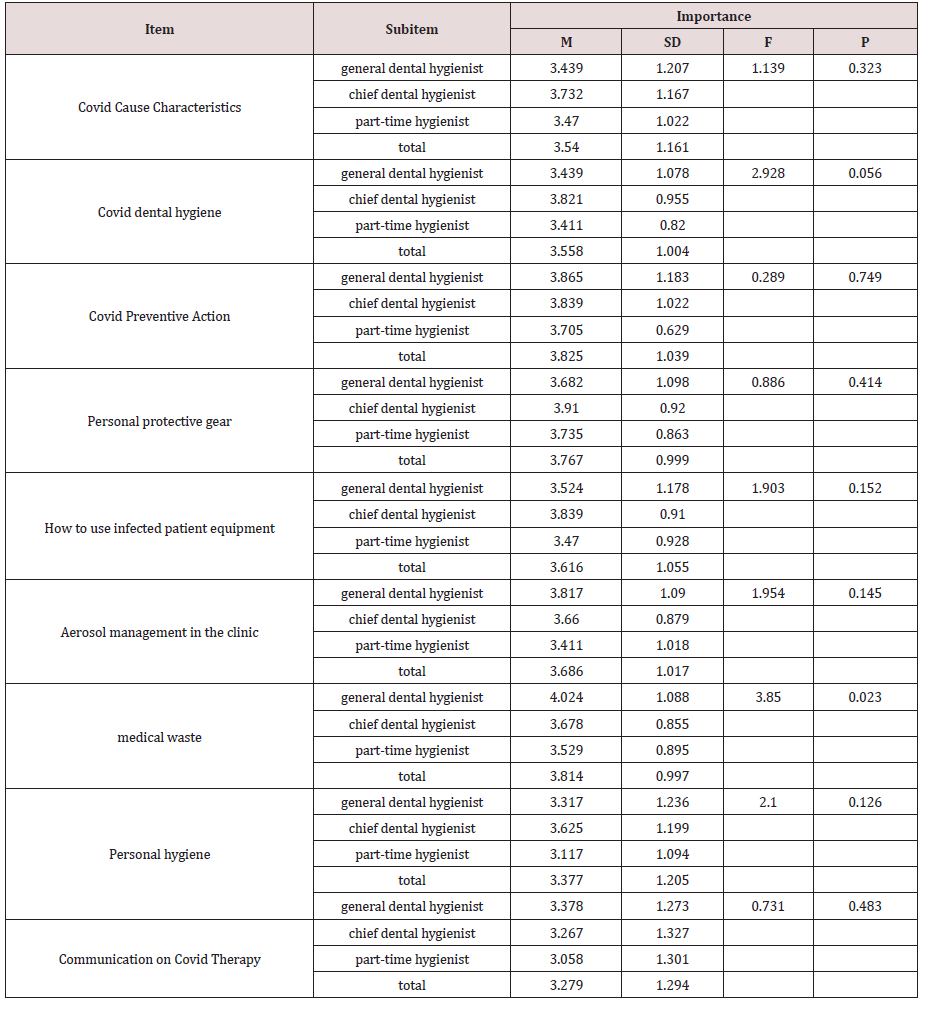
Occupation and Covid Importance ANOVA(Table 2) Covid-cause characteristics by occupation and covid importance variance analysis include a mean and standard deviation for general dental hygienists 3.439 (1.207); the mean and standard deviation for chief dental hygienists 3.732 (1.167); and the mean and standard deviation for part-time dental hygienists 3.470 (1.022); from these f=1.139, p=.The average and standard deviation for general dental hygienists regarding Covid Dental Hygiene being 3.439 (1.207) and the average and standard deviation for primary dental hygienists being 3.821 (9.955), and the average and standard deviation for part-time dental hygienists being 3.558 (1.004), f=2.928, p=.The mean and standard deviation for Covid Preventive Behavior regarding General Dental Hygiene being 3.865 (1.183) along with these, the mean and standard deviation for Principal Dental Hygiene is 3.839 (1.022), and the mean and standard deviation for Part Time Dental Hygiene is 3.705 (0.069), f=.289, p=.749. The average and standard deviation for general dental hygienists on use of personal protective equipment is 3.682 (1.098), the average and standard deviation for primary dental hygienists is 3.910 (9.20), and the average and standard deviation for part-time dental hygienists is 3.735 (8.863), f=.886, p=.How to use infected patient equipment. The average and standard deviation for general dental hygienists is 3.524 (1.178), the average and standard deviation for chief dental hygienists is 3.839 (9.910), the average and standard deviation for part-time dental hygienists is 3.470 (9.928), f=1.903, p=.The average and standard deviation for general dental hygienists in the clinic is 3.817 (1.090), the average and standard deviation for primary dental hygienists is 3.660 (8.879), and the average and standard deviation for part-time dental hygienists is 3.411 (1.018), f=1.954, p=.The average and standard deviation for personal hygiene general dental hygienists is 3.317 (1.236), the average and standard deviation for primary dental hygienists is 3.625 (1.199), and the average and standard deviation for part-time dental hygienists is 3.117 (1.094), f=2.100, p=.Covid Therapy Communication The mean and standard deviation for general dental hygienists is 3.378 (1.273), the mean and standard deviation for primary dental hygienists is 3.267 (1.327), the mean and standard deviation for part-time dental hygienists is 3.058 (1.301), f=731 and p=.483. In medical waste, the average and standard deviation for general dental hygienists is 4.024 (1.088), the average and standard deviation for chief dental hygienists is 3.678 (8.855), and the average and standard deviation for part-time dental hygienists is 3.529 (8.895), f=3.850, p=.023, there is a significant difference at the significance level of 0.05 (Table 2).
(Table 2) Covid-cause characteristics by occupation and covid importance variance analysis include a mean and standard deviation for general dental hygienists 3.439 (1.207); the mean and standard deviation for chief dental hygienists 3.732 (1.167); and the mean and standard deviation for part-time dental hygienists 3.470 (1.022); from these f=1.139, p=.The average and standard deviation for general dental hygienists regarding Covid Dental Hygiene being 3.439 (1.207) and the average and standard deviation for primary dental hygienists being 3.821 (9.955), and the average and standard deviation for part-time dental hygienists being 3.558 (1.004), f=2.928, p=.The mean and standard deviation for Covid Preventive Behavior regarding General Dental Hygiene being 3.865 (1.183) along with these, the mean and standard deviation for Principal Dental Hygiene is 3.839 (1.022), and the mean and standard deviation for Part Time Dental Hygiene is 3.705 (0.069), f=.289, p=.749. The average and standard deviation for general dental hygienists on use of personal protective equipment is 3.682 (1.098), the average and standard deviation for primary dental hygienists is 3.910 (9.20), and the average and standard deviation for part-time dental hygienists is 3.735 (8.863), f=.886, p=.How to use infected patient equipment. The average and standard deviation for general dental hygienists is 3.524 (1.178), the average and standard deviation for chief dental hygienists is 3.839 (9.910), the average and standard deviation for part-time dental hygienists is 3.470 (9.928), f=1.903, p=.The average and standard deviation for general dental hygienists in the clinic is 3.817 (1.090), the average and standard deviation for primary dental hygienists is 3.660 (8.879), and the average and standard deviation for part-time dental hygienists is 3.411 (1.018), f=1.954, p=.The average and standard deviation for personal hygiene general dental hygienists is 3.317 (1.236), the average and standard deviation for primary dental hygienists is 3.625 (1.199), and the average and standard deviation for part-time dental hygienists is 3.117 (1.094), f=2.100, p=.Covid Therapy Communication The mean and standard deviation for general dental hygienists is 3.378 (1.273), the mean and standard deviation for primary dental hygienists is 3.267 (1.327), the mean and standard deviation for part-time dental hygienists is 3.058 (1.301), f=731 and p=.483. In medical waste, the average and standard deviation for general dental hygienists is 4.024 (1.088), the average and standard deviation for chief dental hygienists is 3.678 (8.855), and the average and standard deviation for part-time dental hygienists is 3.529 (8.895), f=3.850, p=.023, there is a significant difference at the significance level of 0.05 (Table 2).
Covid infection education and covid performance Anova test
Covid infection education and Covid performance for the Anova test showed no difference in Covid dental hygiene treatment performance, Covid preventive behavior, personal protective equipment use, clinic aerosol performance, and Covid treatment communication performance. The p value was 13.08. There is a significant difference in 05 and the personal hygiene performance is p=As 024, there is a significant difference at the significance level of 0.05 (Table 3).
Correlation between Covid Importance and Performance
In the correlation analysis, the importance of covid prevention behavior, use of personal protective equipment, maintaining clinic aerosol environment, maintaining personal hygiene along with maintaining covid dental hygiene treatment performance and covid prevention performance, as well as checking for personal protective field performance and personal hygiene performance are all highly correlated (Table 4).
Multiple Regression Analysis on the Number of Patients with Covid Significance and Performance Issues on a Daily Basis
The significance level resulting from testing for significance by heavy regression analysis of covid importance factors and performance issues, with the dependent variable and individual independent variable being the number of patients per day: The independent variable that satisfactorily affects 05 is the degree of performance of covid prevention behavior (t=-2.834, p=).005), room aerosol performance (t=3.042,p=.These had a significant effect as seen in 003) (Table 5).
Table 5: Multiple Regression Analysis of the Number of Patients and Covid Significance and Performance on a Daily Basis ---(n=172).

Conclusion
The U.S. Centers for Disease Control and Prevention [26] said that designating infection control personnel procedures and actively operating programs reduced medical infections by 32%, and otherwise increased safety by 18%. In Korea, infection control is also regulated [27] and the level of practice increased [28] when there was educational experience. Therefore, this study sought to provide basic data on 172 dental hygienists working in dental hospitals and clinics to find out the importance and performance for dental hygienists in identifying infection control factors in order to prepare effective and practical infection control guidelines. This study covered (Table 1) General characteristics, the degree of education: 122, 70.1% had professional bachelors; 44, 25.3% had bachelors; 6, 3.4% had masters; the mean and standard deviation for these being 1.325(5.539), t=32.225, and p=.000. The positions include 82, 47.1% being general dental hygienists; 56, 32.2% being chief dental hygienists; and 34, 19.5% being part-time dental hygienists. The average and standard deviation for these was 1.720 (7.774), t=29.137, p=.000, The daily distribution by patient number for nursing is: 15 practitioners treated 48 patients 27.6%; 16 practitioners treated 8 patients 4.6%; 19 practitioners treated 8 patients 4.6%; 20 practitioners treated 44 patients 25.3%; 21 practitioners treated 8 patients 4.6%; 25 practitioners treated 56 patients 32.3%; and the mean and standard deviation for these surveyed was 19.843 (4.369), t=65.635, p=.000. In the experience of staff training to treat patients with covid infection, 18.3% were trained 1 time; 24 staff, 13.8% were trained 2 times; 40 people 23.0% were trained 3 times; 47 people 27.0% were trained 4 times; 42 people 24.1% were trained 5 times; the mean and standard deviation was 3.483 (1.557), t=29.320, and p=.000. On priority for covid education, 18 people 10.3% responded it was not needed very much; 34 people 19.5% responded it’s not needed; for those responding covid education is needed, 42 people 24.1% said it’s usually needed; 43 people 24.7%, responded it’s very needed, and 35 people 20.1% said it’s quite needed. For these survey responses the mean and standard deviation is 3.250 (1.275), t = 33.414. P= 000. Regarding the Covid education method, 11 people 6.3% answered it’s not needed very much; 15 people 8.6% answered it’s not needed; 26 people 14.9% answered yes it’s needed; 54 people 31.0% answered it’s needed very much; 66 people 37.9% answered it’s quite needed. The mean and standard deviation for these responses are 3.866 (1.204), t=42.111, and p=0.000.
However, the first-year dental hygienist still lacks clinical experience and expertise, so the technology to cope with exposure situations for infectious diseases is insufficient. According to previous studies, it is important to increase theoretical knowledge and performance standards that can be directly applied to clinical sites for medical-related infection management, but it is reported that nursing students have lower than needed understanding to perform infection management knowledge correctly [29,30]. Other studies have reported that nursing students’ experience of Level D attachment and removal of personal protective equipment significantly increased their self-efficacy and risk of infection in nursing practice [31]. In this study, covid infection education and covid treatment performance were found to be no different at a significance level of 0.05 in Anova test, covid dental hygiene performance, covid prevention behavior performance, personal protective equipment use, clinic aerosol performance, and covid treatment communication performance showing no difference; the performance p value of the covid-cause characteristic was .013, which showed a significant difference at the significance level of 0.05. The performance of medical waste was also p=.008. There was a significant difference in 05 and the personal hygiene performance being p=As 024; there was a significant difference at the significance level of 0.05 (Table 3). In this study (Table 4) correlation analysis, the importance of covid prevention behavior, personal protective equipment, clinic aerosol importance, personal hygiene importance, covid dental hygiene treatment performance, covid prevention behavior performance, personal protective medicine performance, and personal hygiene performance were highly correlated. In previous studies, many dental staff answered that the reason for not practicing infection prevention behavior was high, and 77.7% of them said that the reason why hand washing performance was not well practiced in [32] Park et al. [33] was because of busy work. In addition, Bae and Lee [34] said that when looking at the time and workload of infection control subjects in domestic dental hospitals devoted to the work in the dental field, other tasks such as treatment accounted for relatively higher proportions of time than the unique tasks of infection control.
In this study, there were no significant results in covid cause characteristics, covid dental hygiene, covid prophylactic behavior, personal protective equipment, room aerosol management, personal hygiene, and covid therapy communication. As in 023, there was a significant difference at the significance level of 0.05. The significance level as a result of testing for significance by heavy regression analysis for the covid importance and performance based on the dependent variable and individual independent variable being taken from the number of patients per day. The independent variable that satisfactorily affects 05 is the degree of performance of covid prevention behavior (t=-2.834, p=.005), with room aerosol performance (t=3.042, p=.003) also having a significant impact (Table 5). It was pointed out that although there are various methods for infection control, there was no accurate evidence for their effectiveness. Thus, it was necessary to study various management methods to generalize infection control methods for dental workers [34]. In addition, that study suggested institutional improvements were needed to develop and apply infection control standards appropriate to the actual conditions according to the structure and treatment type of each dental institution in order to increase and activate infection control procedures in each dental institution [35]. Although these results cannot be directly compared with this study, their meaning is expressed in the context of the need for a structured system to systematically carry out infection control activities within medical institutions in order to increase awareness for the importance and performance of infection control. In order to increase the importance and performance of dental infection management, administrative and financial support should be delegated to establish and activate an infection control structure system, and institutional improvement is needed to make it mandatory. The limitation of this study is that it is a crosssectional study of some regions and cannot reflect the infection management structure system according to the characteristics of each dental institution. Thus, it is necessary to investigate the recognition to practice dental infection management in dental systems in future studies. In conclusion, through this study, it can be seen that although practitioners are somewhat equipped in terms of the infection control structures in dental clinics, the actual performance rate is low due to the lack of infection control personnel and lack of infection monitoring standards. Therefore, it is desperately needed to develop infection monitoring standards and infection control guidelines applicable to dental hospitals, and it is also necessary to strengthen infection control in nursing hospitals by securing dedicated personnel to apply the needed procedures.
Discussion
This study conducted a research survey on 172 dental hygienists working at Y Dental Clinic, S Dental Hospital, L Dental Hospital, and J Dental Hospital in Gwangju Metropolitan City from May 1 to May 30, 2022. Participants in this study were surveyed by dental hygienists who had tested negative after contacting COVID-19 confirmed patients. Survey participants agreed to understand the purpose of the study and participate in the study, and the survey was conducted in a self-fill in manner. The purpose of this study was to find specific areas of problems by analyzing the infection control level of dental hygienists through gender, age, education level, position, number of those in daily replantation nursing, Covid infection education, need and performance of dental hygienists, and to use these criteria as basic data to improve infection and medical service quality.
a) The general characteristics of 172 subjects are gender, age, education level, position, number of those in daily replantation nursing, education of patients with covid infection, necessity of covid infection education, and method of covid education.
b) Covid Cause Characteristics, Covid Dental Hygiene, Covid Preventive Behavior, Personal Protective Equipment, Infected Patient Equipment, Clinic Aerosol Management, Personal Hygiene, Covid Therapy Communication showed no significant results, and the average and standard deviation of general dental hygienists in medical waste was 4.024 (1.088) The average and standard deviation of the chief dental hygienist is 3.678 (.855) The mean and standard deviation of part-time dental hygienists is 3.529 (8.895), f=3.850, p=.There is a significant difference at 023, the significance level of 0.05.
c) The performance of the covid-cause characteristic was also p=.013, showing a significant difference at the significance level of 0.05, and the performance of medical products was also p=.008.There is a significant difference between 05 and personal hygiene performance. There is a significant difference at p=.024, and the significance level of .05.
d) Correlation analysis shows that the importance of covid prevention behavior, personal protective equipment, clinic aerosol importance, personal hygiene importance, covid dental treatment performance, covid preventive behavior performance, clinic aerosol performance, and personal hygiene performance are highly correlated.
e) As a result of testing the significance of multiple regression analysis for the Covid importance and performance of the dependent variable and individual independent variable, which are patient nursing numbers on 5.1 days, the degree of Covid prophylaxis performance was (t=-2.834, p=.005), room aerosol performance was (t=3.042, p=.003). These show a significant effect.
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- Moon HS (1992) A Study on the Health of Dentists. Journal of the Korean Oral Health Association 16(1): 53- 73.
- Hardie J (1992) Concerns regarding infection control recommendations for dental practice. J Can Dent Assoc 58: 337-386.
- Haley RW, Morgan WM, Culver DH (1985) Update from the SENIC project. Hosptial infection control: recent progress and opportunities under prospective payment. Am J Infect Control 13: 97-108.
- (2006) Ministry of Health and Welfare: Guideline on infection control in dental treatments. Ministry of Health and Welfare, Sejong, p. 1-3.
- (2013) Ministry of Health and Welfare, Korea Institute for Healthcare Accreditation: Dental hospital accreditation standard. Mini- stry of Health and Welfare, Seoul, pp.107-117.
- Cho MJ (2011) A study on re-use intention through external stimuli and infection control of dental office perceived by medical consumer. J Korean Soc Dent Hyg 11: 571-580.
- Lee JH (2013) A survey of cognition on infection control of the clients in dental hospital. J Korean Dent Hyg Sci 13: 129-260.
- Nam SM (2011) A study on infection control practices by dental hygienists. J Korean Soc Dent Hyg 11: 137-148.
- You SM (2013) Knowledge, Attitude, and Performance of Handwashing by Health University Students. Journal of the Korean Society of Industrial Technology 14(8): 3916-3924.
- (2022) Korea Centers for Disease Control and Prevention and the Korean Medical Association for the Prevention of Infection Standards.
- (2006) Ministry of Health and Welfare. Dental treatment Prevention of Infection Korea.
- Chung HJ, Lee JH (2015) Factors influencing the perception and practice of infection control by dental hygienists in some areas. Journal of the Korean Dental Hygiene Society 15(3): 363-369.
- Lee YH, Choi SM (2015) Awareness and Practice Survey of Dental Infection Management by Type of Workplace. Journal of the Korean Society of Radiology 9(6): 409-416.
- Jeon JS, Choi SM, Lee YH (2018) A Comparative Study on the Perception and Practice of Infection Control by Dental Hygienists Multi-media paper on the convergence of art and humanities society 8(12): 597-606.
- (2008) Ministry of Environment, Medical Waste Management System Guide, Republic of Korea.
- National Legal Information Center. Article 2, 5 of the Waste Management Act (2020), Republic of Koreahtt
- (1999) American Dental Association Council on Scientific Affairs. Dental unit waterlines: approaching the year 2000. ADA Council on Scientific Affairs. J Am Dent Assoc 130(11): 1653-1664.
- Lee SS, Kim DY, Song SY (2016) Perception and practice of dental hygienists on the maintenance of dental units. Journal of the Korean Dental Hygiene Society 16(4): 507.
- Ministry of Health and Welfare Revision of Guidelines for Disinfection of Equipment and Articles for Use of Medical Institutions, Republic of Korea . 2017.
- Son EK, Choi UY, Jung HY (2016) Survey on the management of uniforms by dental hygienists. Survey on uniform management by Son, Choi Woo-yang, Jeong Hwa-young, and other dental hygienists. Survey on uniform management by Son, Choi Woo-yang, Jeong Hwa-young, and other dental hygienists. Journal of the Korean Dental Hygiene Society 16(4): 517-523.
- Bae SS (2011) Development of evaluation index for infection control and prevention at dental hospital. Unpublished doc- toral dissertation, Ewha Womans University, Seoul, Korea.
- Askarian M, Honarvr B, Tabatabaee HR, Assadian O (2004) Knowledge, Practice and Attitude towards Standard Isolation Precaution in Iranian Medical Students. Journal of Hospital Infection 58: 292-296.
- (2021) Korea Centers for Disease Control and Prevention's standard prevention guidelines for infection prevention and management of COVID-19 in dental medical institutions.
- (1985) Hospital infection control: recent progress and opportunities under prospective payment. Am J Infect Control 13(3): 97-108.
- Jeong HJ, Lee JH (2016) A survey on infection control status of the dental care institution. AJMAHS 6(6): 51-58.
- Nam YS, Yoo JS, Park MS (2007) A study on actual conditions for prevention of infections by dental hygienists. J Den Hyg Sci 7(1): 1-7.
- Kohn WG, Harte JA, Malvitz DM (2004) Guidelines for infection control in dental health care settings-2003. J Am Dent Assoc 13(5): 3-47.
- Kim BY, Park JM, Park EJ (2014) A study on the impacts of infection control education on dental hygienist perceptions for hepatitis type B and their practices to prevent infection. J Korean Acad Prosthodont 52: 287-297.
- Park JH, Heo NS, Song HJ (2011) A study of current infection control by dental hygienists and related factors. J Korean Soc Dent Hyg 11: 993-1003.
- Bae SS, Lee MS (2011) Study on elements for effective infection control at dental hospitals. J Korean Soc Dent Hyg 11: 557-569.
- Yoon HY, Lee SY (2015) The microbial contamination and effective control method of dental unit water system. J Korean Dent Hyg Sci 15: 383-392.
Editorial Manager:
Email:
pediatricdentistry@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...