Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6636
Research Article(ISSN: 2637-6636) 
Visual Support Requirement of Patients with Autism Spectrum Disorders during Periodic Dental Check-Ups Volume 7 - Issue 5
Chungtzu Hsueh1, Ogasawara Tadashi2,3*, Suzuki Kahori2,4 and Okada Yoshiyuk5
Received: May 25, 2022; Published: June 09, 2022
*Corresponding author: Ogasawara Tadashi, Department of Pediatric Dentistry, Yokosuna Dental Clinic, Shizuoka, Japan
DOI: 10.32474/IPDOAJ.2022.07.000272
Summary
Aims: Visual support of the TEACCH program has been reported to be effective in communicating new tasks in dentistry in ASD (ASD), but the need for routine activity remains unclear. Patients with ASD were investigated for their need for visual support in routine activity of regular dental check-ups.
Methods: Altogether, 36 patients with ASD were investigated in terms of sex, age, visual support in daily life, developmental age, severe behavioral disorder, and dental experience by interviewing caregivers or parents. The need for visual support was confirmed in three steps: “ lying down on the dental chair”, ”opening their mouth”, and ” using a rotary brush.” A decision tree analysis was performed to explore factors requiring visual support in regular dental check-ups.
Results: Of the patients, 80.6% did not always require visual support in routine dental settings. The factor associated with the requirement for visual support was “difficult-to-handle panic.” Those who received visual support during regular dental check-ups required visual support for “opening their mouth”.
Conclusion: Almost patients with ASD do not need visual assistance for routine dental check-ups activities. Evaluating the need for visual support with associated factors and providing visual support as needed are crucial.
Keywords: Autism spectrum disorder; communication; oral examination; visual support; TEACCH program
Introduction
Dental treatments of patients with ASD are more difficult than those of patients with intellectual disability [1,2] because of the latter’s impairments in social interaction, mutual relationships, and social communication [3]. Patients with ASD may show refusal behavior such as not sitting on the dental chair or not assuming the supine position during oral examinations and dental treatments. This is because they have uncertainties, fears, and confusion regarding unexpected things, which are derived from a lack of understanding of verbal forms of communication. Therefore, people with ASD have been recommended to use the TEACCH(Treatment and Education of Autistic and Related Communication Handicapped Children) program [4,5] because they have excellent understanding and visual memory despite their difficulty in understanding spoken words [6]. The TEACCH program was reported to be effective in dental practice [7] and relaying toothbrushing instruction [8] due to the visual structure that shows what to do in advance with pictures and photographs.
It is well known that visual support is important in patients with ASD to help them understand and experience something for the first time to allay their uncertainties. However, the need for visual support for routine activities in the dental office, such as oral examinations and professional mechanical tooth cleaning during periodic dental check-ups is unclear. Although they have undergone oral examinations many times during regular dental check-ups, some require visual support to accept regular dental examinations, while others do not. Schopler E [4] has advocated the importance of preparing the environment to compensate for their weaknesses, and that understanding from the actual observation of the child is the basic idea of the TEACCH program. All patients with ASD may not need visual support. Providing visual support to all patients with ASD prolongs oral examination time. However, there is no information on the proportion and factors of patients with ASD who require visual support, even for routine dental activities. Moreover, communication difficulties in patients with autistic spectrum disorders vary widely depending on individual characteristics and developmental stage. Thus, we investigated the percentage of patients with ASD who require visual support and patients’ characteristics associated with the need for visual support when assuming the supine position, opening their mouth by themselves, and accepting professional mechanical tooth cleaning in regular dental check-ups.
Methods
Participants
Altogether, 36 patients (27 men and 9 women) diagnosed with ASD who underwent regular oral examinations in our institution were included in this study between April and August of 2014. Written informed consent was obtained from all the patients and their parents. None of the participants were applied with physical restraint in our department. The mean age of the participants was 19.4 ± 10.4 years (mean ± S.D.) [4–45 years (range)]. This study was approved by the institution’s ethics committee (approval number: 200).
Interview with caregivers or parents
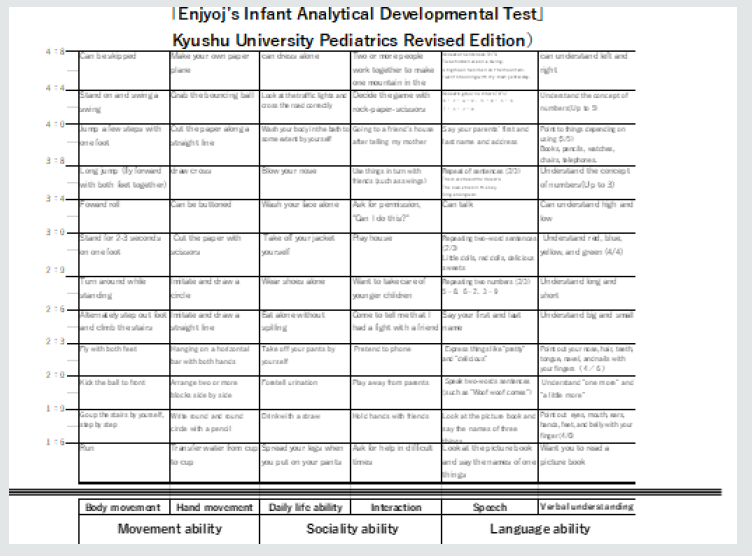
The parents or caregivers were interviewed regarding the presence or absence of visual support in the patients’ daily life, previous dental experiences, the age of the patients during their first experience of physical restraint during dental treatment, amount of time of restraint, and previous history of panic during dental treatment. Periodic dental check-ups, number of periodic dental check-ups, number of dental treatments under intravenous sedation, number of dental treatments under local anesthesia, performing visual support (VS) in a periodic oral examination, and DMF were investigated from dental records. The Enjoji infant analytical development test (Figure 1) was performed to evaluate the developmental age of locomotion, hand movement, basic habits, interpersonal relationships, speech, and language comprehension [9]. Severe behavioral disorders according to the Ministry of Health, Labor, and Welfare (Table 1) were evaluated by interviewing the parents and caregivers.
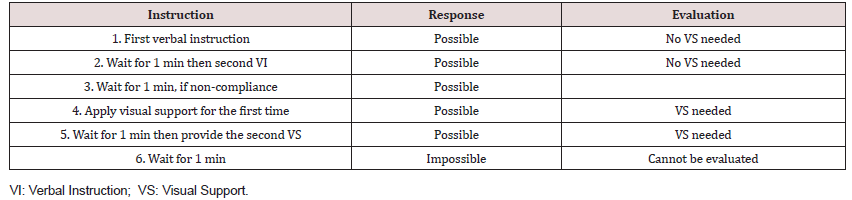
Procedure and judgment
The need for visual support was identified in three steps after calling the patient in the waiting room. The three steps were as follows: “Please lie down on the dental chair”; “Please open your mouth”; and “I will brush your teeth using a rotary brush.” Instructions and judgment were given at each step according to the procedure in Table 2. Illustrations of visual support are shown in Figure 2.Analysis
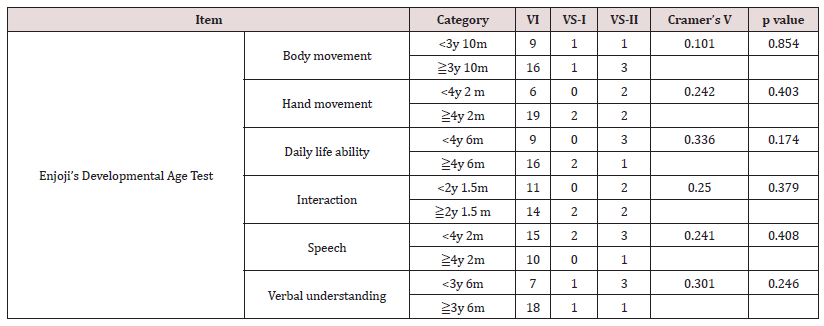
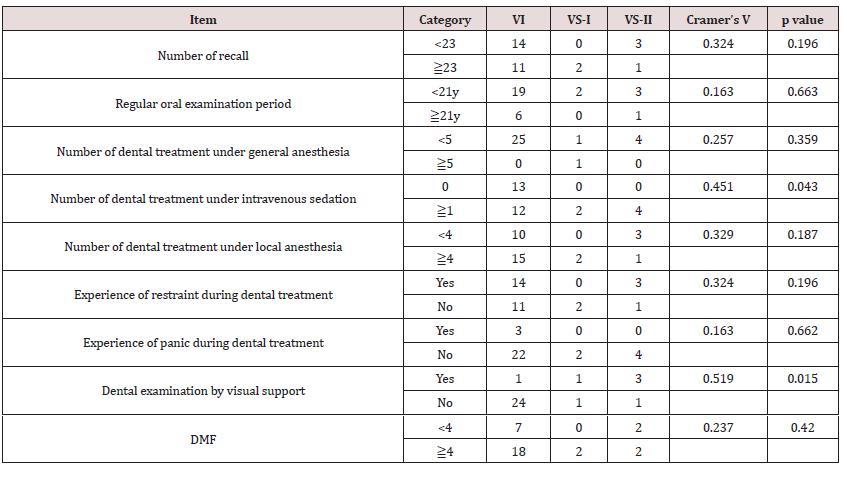
Those who could perform three tasks only by verbal instruction were classified into the verbal instruction (VI) group, those who performed even one visual support of three tasks were classified as the VS group, and those who could not perform all tasks by oral instruction and VS were classified as the non-compliance group. The ratio of the patients who belonged to each group was calculated. Furthermore, among the VS group, those who received VS only while lying on the dental chair were designated as the first only VS group (VS-I group), and those who received VS when opening their mouth or brushing their teeth with a polishing brush were designated as the VS from the middle task group (VS-II group). The relationship between the three groups (VI group, VS-I and VS-II groups), patient background, and dental treatment experience was analyzed using the G test and Cramer’s V. Cramer’s V was compared with each dividing point of number in the items of the ordinal scale (age of history, age of development, number of recalls, duration of regular examination, number of general anesthesia, number of local anesthesia, DMF). The significance level was set at 5%. A decision tree analysis was performed with the VI group, VS-I, and VS-II as objective variables and the items with significant differences as explanatory variables to search for factors that require VS. The G test and Cramer’s V were performed using Stat Mate III (Atms, Tokyo), and the decision tree analysis was performed using IBM SPSS Decision Trees (IBM, Tokyo).Results
Developmental age of participants
The median developmental age of the participants was 4 years and 2 months for the developmental fields of locomotion and hand movement, 4 years and 6 months for the developmental field of basic habits (upper limit of developmental age that can be tested), 2 years and 1.5 months for the developmental field of interpersonal relationships, 2 years and 4.5 months for the developmental field of speech, and 3 years and 10 months for the developmental field of language understanding (Figure 3).
Figure 3: Patient distribution according to Enjoji’s developmental age. The median age for interaction and speech is around 2 years, which is far below that for the other items.

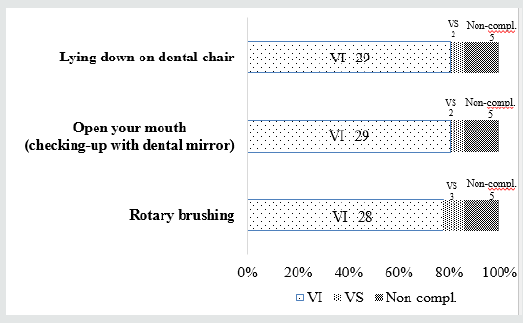
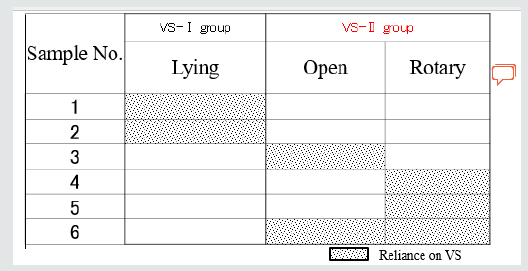
Proportion of Response to Each Instruction
Here, 29 patients (80.6%) were able to execute “lying down on dental chair” and “open their mouth” by verbal instructions, 2 patients (5.6%) were able to execute them by visual support but not by verbal instruction, 28 people (77.8%) were able to accept “brushing their teeth with the rotary brush” by verbal instructions, 2 (5.6%) were able to do it with visual support, and 5 people (13.9%) were unable to do it despite providing both verbal instruction and visual support (Figure 4). Those who could not perform each task from the provided verbal instructions and visual support were the same. Except for five people who could not perform any tasks, 25 people (80.6%) were able to perform all tasks by verbal instruction, and six people (19.4%) required visual support (Figure 5). Regarding the requirement of visual support, two people were provided visual support only for “lie down on the dental chair,” and did not need visual support in the latter two tasks. Two people were provided visual support for “opening your mouth”, and three people were provided visual support for “brushing your teeth with the rotary brush”. Therefore, the participants were classified into two groups: two people in the VS-I group and four people in the VS-II group (Figure 6).
Figure 5: Grouping the patients reliant on visual support (VS). There were 25 persons in the Oral Guidance (VI) group and 6 persons in the VS group except for the 5 persons of non-compliance groups.
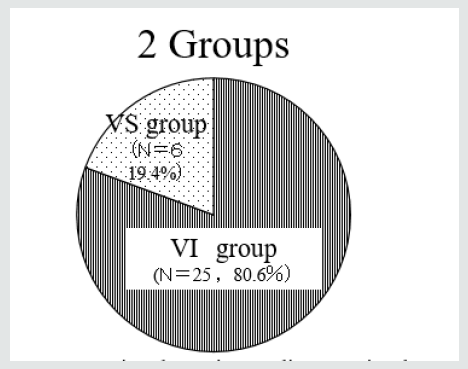
Figure 6: Details of the visual support (VS) group. According to the 3 consecutive steps, we divided the VS group into patients who received VS before lying on the dental chair at the first step (2 patients: VS-I group) and those who received VS when opening their mouth or brushing their teeth with a polishing brush (4 patients: VS-II group).
Single correlation between patient background and visual support
No association was found between developmental age and implementation of visual support in all groups. Items that were found to be related to the implementation of visual support were “the previous history of panics that are difficult to deal with,” “number of experiences with intravenous sedation,” and “performing VS in a periodic oral examination” (Tables 3-6).
Table 5: Single correlation between patient background and visual support: patient’s behavioral disorder.

Decision tree analysis
A decision tree analysis was performed using the three items of “the previous history of panic that is difficult to deal with,” “number of experiences of intravenous sedation,” and “implementation of visual support during oral examination” as explanatory variables. Of these results, “the previous history of panic that is difficult to deal with” had the strongest effect on visual support, and the patients with this item required visual support at the beginning. The second most influential factor was “performing VS at regular checkups”. Those who required visual support at the time of the oral examination tended to perform tasks with visual support from the second task “open your mouth” The number of intravenous sedations was not extracted as a related factor (Figure 6).
Figure 7: Factors affecting reliance on visual support (VS) based on the decision-tree analysis. The decision tree analysis indicates that intense panic and VS during previous dental check-up are factors affecting reliance on VS.

Discussion
Participants
Cooperativity in dental examinations in individuals with ASD is reportedly associated with the ability to dress oneself, [10] ability to communicate verbally, [10] sitting for haircuts, [11] and reading [11]. People with ASD have no movement disorders, so being able to put on and take off clothes and sit down for a haircut indicates their intellectual ability and developmental stage. Takai [12] has reported that oral examinations for children with developmental disabilities over two years and six months of age are accepted. The participants with ASD in this survey had a median age of development of basic habits of 4 years and 6 months or more and were able to put on and take off their clothes. Those who cried and showed refusal behavior during the oral examination were excluded from the analysis of the need for visual support, so those who had the ability to accept the oral examination and tooth surface polishing were the participants.
The necessity of visual support
The characteristics of ASD include poor verbal communication, lack of imagination, and lack of prediction ability, and they have difficulty accepting instructions [3,5]. Especially for the first visiting dental treatment of people with ASD, visual support is effective as a structure of information based on the TEACCH program, due to communication problems and lack of imagination [4,5]. Visual support based on the TEACCH program has been reported to be effective in dental treatment [7,13-17]. Thus, visual support should be provided when a person with ASD first visits a dental office. However, the factors for those who need visual support and the need for routine activities as oral examinations in the same dental office is unclear. According to this study’s results, 80% of the participants did not require visual support. Only 6.5% required visual support to lie down on the dental chair and to open their mouth during periodic dental examinations, and to open their mouth in periodic dental examinations. A total of 9.7% required visual support to brush their teeth with a rotary brush. A total of 19.4% required visual support in one or more of the three steps, and 80.6% were able to perform the three steps by verbal instruction. Most people could understand and perform the three steps by verbal instructions if it was a routine task. It was suggested that all people with ASD do not need the pattern of visual support in the routine of lying down on the dental chair during oral examination and brushing their teeth.
The most relevant factor for requiring visual support was “difficult-to-handle panic.” Those with “difficult-to-handle panic” tended to require visual support only at the beginning. Panic is caused by not understanding what will come next, disliking being touched due to hyperesthesia, interrupting their favorite activities, being unable to control excited feelings, and being unwell. People with ASD tend to panic because they cannot control unbearable stress by themselves. Those who have the “difficult-to-handle panic” cannot accept verbal instructions and cannot lie down on the dental chair because they do not understand what will come next and feel anxious in front of the dental chair. Here, the patients were able to open their mouths, undergo oral examinations, and brush their teeth with verbal instructions. However, when giving a verbal instruction to “open the mouth,” the dentist held the mirror and gave the verbal instruction. The verbal instruction “brush your teeth with the rotary brush” was also given while offering a brush. The procedure may have been understood and accepted by looking at the dental equipment, and it is unknown whether it was accepted only by verbal instructions. Hence, it was considered that those who gave visual assistance only for the first instruction might not be able to understand verbal instructions without a mirror or rotary brush. I reconfirmed that showing dental tools to show what to do next will lead to structuring.
The second most relevant item to the need for visual support was “implementation of visual assistance in previous dental examinations.” Those who had “implemented visual support in the previous dental examination” could take the supine position on the dental chair by verbal instructions and needed visual support from the middle task. The situations that required visual support were only when one person opened his mouth, one person only polished the tooth surface, and one person both opened his mouth and polished the tooth surface. The considered factors that required visual assistance were anxiety, uncertainty, and ritualistic behavior. They did not require visual assistance in all the steps, so they required visual support in each situation. They may have felt uncertain by receiving only verbal instructions, although they could understand and allowed opening their mouth, oral examination, and tooth surface polishing with the visual support of the illustrations. Identifying the need for visual support in each task is important for individuals with ASD. Considering their capabilities, it is useful to provide visual support when they experience difficulty because they cannot follow the instructions. That is exactly how the TEACCH program tries to compensate for their weaknesses [4]. Visual support for those who do not require it may hinder their independence. The basic philosophy of the TEACCH program is individualization [4,5]. This study confirmed the importance of having dental staff evaluate each individual and provide visual support as needed.
Bullet Points
Pediatric dentists often perform periodic dental check-ups for people with ASD. This paper may reduce the burden on individual ASD individuals. The results of this paper may shorten routine visits for people with ASD.
Conflict of Interest
There are no conflicts of interest to report.
References
- Hosaka Kazuo OT, Tsukada Kumiko, Ohta Shingo, Takai Tsuneyuki, Nomura Keiko, et al. (1998) Predestinate of adaptability of developmentally retarded to dental treatment, Developmental age 3 years 10 months as critical point. JJSDH 19: 163-169.
- Sumida Sachi, Ogasawara Tadashi WN, Kawase Mizuho, Hosaka Kazuo, Matsuo Koichiroi, et al. (2009) Adjustment in dentistry for autistic persons from the Viewpoint of development and special characteristics. JJSDOH 30: 550-555.
- APA (2013) The Diagnostic and Statistical Manual of Mental Disorders: DSM 5. Washington, DC, USA p. 49-57.
- Schopler E (1966) Visual versus tactual receptor preference in normal and schizophrenic children. Journal of Abnormal Psychology 71: 108-114.
- Sasaki M (2007) Nihon Rinsho 65: 512-515.
- Dakin S, Frith U (2005) Vagaries of visual perception in autism. Neuron 48: 497-507.
- Orellana LM, Martínez-Sanchis S, Silvestre FJ (2014) Training adults and children with an autism spectrum disorder to be compliant with a clinical dental assessment using a TEACCH-based approach. J Autism Dev Disord 44: 776-785.
- Ogasawara Tadashi, KolzumI Mari YK, Sumida Sachi, Mitsui Takanobu, Andou Nobuyuki, et al. (2007) The readiness and effect of visual support in tooth brushing instruction for people with Autistic Disorders. JJSDOH 28: 28-33.
- Enjoji Munenori GN, Kurokawa Toru, Nawa Akiko, Nanbu Yumiko, Shinohara Shinobu, et al. (2012) The Enjoji infant analytical development test Kyushu University Pediatrics Revised New Edition, Keio University Press, Tokyo, Japan p. 4-9.
- Nelson T, Chim A, Sheller BL (2017) Predicting successful dental examinations for children with autism spectrum disorder in the context of a dental desensitization program. J Am Dent Assoc 148: 485-492.
- Marshall J, Sheller B, Williams BJ (2007) Cooperation predictors for dental patients with autism. Pediatr Dent 29: 369-376.
- Takai Tsuneyuki OT, Kawase Yuka, Kojima Hiroomi, Ohtsuki Yukihisa, Ohtuki Mariko, et al. (2002) Readiness of disabled children for oral examination. JJSDH 23: 27-32.
- Virues-Ortega J, Julio FM and Pastor-Barriuso R (2013) The TEACCH program for children and adults with autism: a meta-analysis of intervention studies. Clin Psychol Rev 33: 940-953.
- Elmore JL, Bruhn AM, Bobzien JL (2016) Interventions for the Reduction of Dental Anxiety and Corresponding Behavioral Deficits in Children with Autism Spectrum Disorder. J Dent Hyg 90: 111-120.
- Balian A, Cirio S, Salerno C (2021) Is Visual Pedagogy Effective in Improving Cooperation Towards Oral Hygiene and Dental Care in Children with Autism Spectrum Disorder? A Systematic Review and Meta-Analysis. Int J Environ Res Public Health p. 18.
- Cagetti MG, Mastroberardino S, Campus S (2015) Dental care protocol based on visual supports for children with autism spectrum disorders. Med Oral Patol Oral Cir Bucal 20: e598-604.
- Pilebro C, Bäckman B (2005) Teaching oral hygiene to children with autism. Int J Paediatr Dent 15: 1-9.
Editorial Manager:
Email:
pediatricdentistry@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...