Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6636
Review Article(ISSN: 2637-6636) 
Viral Enanthems and Oral Mucosal Lesions in Viral Infections in Children and Adolescents Volume 6 - Issue 2
Satarupa Ghosal Bhattacharyya1 and Sayan Bhattacharyya2*
- 1BDS, Dental Surgeon, Kolkata, India
- 2Assistant Professor, Department of Microbiology, AIIH&PH, India
Received:May 07, 2021 Published: May 17, 2021
*Corresponding author: Sayan Bhattacharyya, Assistant Professor, Department of Microbiology, AIIH&PH, India
DOI: 10.32474/IPDOAJ.2021.06.000231
Abstract
Oral lesions , also sometimes called enanthems, can be seen in many viral infections. They are typical of some viral infections in most cases but can also be non-specific. Proper clinical suspicion and Laboratory tests can clinch the diagnosis of such infections.
Keywords:Enanthems; herpes; infectious mononucleosis; koplik’s spots
Introduction
Enanthems are oral and mucosal rashes or spots that appear in many viral infections, particularly in children. They can be diagnostic of these diseases. A good clinical history and study of the appearance and description of these rashes, along with diagnostic tests, can establish diagnosis of these infections with high specificity and accuracy. Both dentists and clinicians have to suspect these lesions properly for proper diagnosis. However, the diagnosis is often missed unled proper inquisitive history taking and oral examination are carried out in such patients. Hence the scope of this review article is to summarize the available knowledge of these enanthems.
Materials and Methods
Thorough literature search was done scientifically to find out and enumerate the various viral enanthems.
a) Koplik’s spots: Koplik’s spots are characteristically seen in inside of buccal mucosa opposite first and second upper molars [1]. They are seen in Measles. Koplik’s spots appear as white grain of sand surrounded by red ring. Koplik spots appear in 60% to 70% of people suffering from measles [2]. Though commonly seen in buccal mucosa, Occasionally, they may also appear in other areas such as the soft palate, conjunctival fold, and vaginal or intestinal mucosa and usually persist for 2 or 3 days [2]. They were named after Dr Henry Koplik of New York, who described them in 1896 [1,2] (Figure 1).
b) Forchheimer’s spots: These rashes are characteristically found in some of the Rubella patients. Forchheimer spots are found in about 20% of patients with rubella with enanthem as small, red spots on the soft palate, occasionally before onset of a rash [3]. These spots are not specific for Rubella and can be seen in cases of measles, scarlet fever, and other systemic infections also [3]. It is also fleeting in nature. It named after Frederick Forchheimer [4]. Enanthems in infectious mononucleosis: Red spots over hard and soft palate are seen in Infectious mononucleosis. Occasionally oral hairy leukoplakia can also be seen.
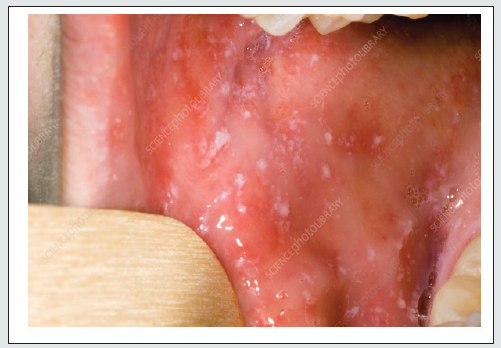
c) Herpetic enanthems: Herpetic gingivostomatitis is the commonest acute clinical manifestation of primary HSV (Herpes Simplex Virus) infection, usually caused due to HSV-1. It occurs between the ages of 6 months and 5 years [5]. It usually presents with flu-like manifestations (fever, chills, and cervical and submandibular lymphadenopathy), intraoral mucosal vesicles (about 2-3 mm in size), involving the gingiva, lips, hard and soft palate, tongue, buccal mucosa, and perioral regions. The vesicles may coalesce, especially on the mucosa of the cheeks and under the tongue, forming ulcers surrounded by erythema [5]. The lips and gingiva may get swollen, and the lesions are painful and may resemble those of aphthous stomatitis ; they may also prevent feeding of the child.
Findings in Epstein-Barr virus infections: EBV is a very common herpesvirus which is spread from man to man by contact with saliva. In many cases, there may be a maculopapular enanthems and petechiae, located between the hard and soft palate, often coalescing together [5]. Oral hairy leukoplakia (OHL) is a disorder of the mucosa associated with EBV infection and occurring mostly in patients infected with HIV, as well as in HIV-negative patients with organ transplants or immunocompromising diseases [5]. OHL appears as a white patch on the lateral surfaces of the tongue, unilaterally or bilaterally, with a corrugated or hairy appearance which cannot be scraped off. The lesions may sometimes involve the buccal mucosa, palate, or pharynx. The pathogenesis of OHL is unclear; the virus, however, may be recovered from the upper layers of the epithelium [5]. Recent studies have also implicated EBV in the pathogenesis of advanced types of periodontal disease [6]. Nagayama spots: Nagayama spots, an enanthem associated with HHV-6 primary infection, are reddish macules and papules seen on the soft palate and uvula. These can be seen in twothirds of patients with exanthema subitum, which is the typical exanthema associated in children with HHV-6 [5]. It can be seen also in Roseola infantum. Classic roseola infantum is a clinically based diagnosis. It starts with high fever that may be over 40° C (104 °F). The fever usually lasts three to five days. During the fever, children may appear to be active and well. However, children may also have malaise, conjunctivitis, orbital edema, inflammation of the tympanic membranes, lymphadenopathy, irritability, anorexia, a bulging fontanelle, diarrhea, cough, and other upper respiratory tract symptoms [7]. Nagayama spots, occur in these patients as erythematous papules found on the soft palate and uvula that are seen in two-thirds of cases [7]. HHV-8 and lesions in mouth: Human Herpesvirus 8 is associated with Kaposis’s Sarcoma and multicentric Castleman’s disease. The clinical features of oral involvement by HHV-8 are maculopapular rashes (75%) or nodular lesions (14%), and proliferative lesions such as tumors (11%) primarily seen on the hard palate followed by involvement of the oropharynx. The tongue, gingiva, and oral mucosa are less commonly involved. All of these lesions may bleed after eating [5,8].
d) Parvovirus B19 infections: PB19 V is the causative agent of erythema infectious (fifth disease) characterized by a “slapped cheek appearance” and an erythematous maculopapular exanthem involving the trunk and extremities. Oral and mucosal lesions can also be found here. Oral lesions include petechiae, vesicles and pustules, and small erosions developing on the lips, buccal mucosa, and soft palate [5,9]. PB19 V oral lesions may mimic Koplik’s spots [5].
e) Hand- foot and mouth disease and Herpangina:
The causative agent of herpangina is most commonly CV (Coxsackieviruses) group A and sometimes CV group B, echoviruses, adenoviruses, and parechovirus 1. The involved types can change depending on the outbreak and the geographic area. Mainly, herpangina affects children younger than 10 years of age in the summer or early autumn [5]. It starts with fever and malaise, followed by lymphadenopathy, sialorrhea and a typical enanthem characterized by some painful grayish white papulovesicular lesions which rapidly evolve into shallow ulcerations with a red rim. Lesions are found on the soft palate, uvula, tonsils, and pharynx [5,10].
Enteroviruses may also produce a maculopapular eruption or HFMD (Hand Foot and Mouth disease), frequently associated with systemic symptoms [5]. Coxsackievirus, mainly A16 type, causes HFMD . It is a highly contagious infection that begins with an incubation period of 3 to 7 days and is typified by nonspecific constitutional symptoms, like low-grade fever and malaise. Shortly after this, the patient complains of sore throat with papulovesicular lesions in mouth that rapidly erode, developing shallow ulcerations. Generally, the enanthem starts before the exanthem. Atypical HFMD also has been reported worldwide, caused by CV-A6 and CV-A10 [5]. It is characterized by a relative absence of oral lesions and vesico-bullous lesions that have a wider distribution on the extremities and trunk than typical HFMD. Perioral erythematous papules can be seen only in atypical HFMD due to CV-A6. Another oropharyngeal involvement without skin lesions may be caused by group A CV. It is an acute lymphonodular pharyngitis, consisting of raised, tiny nodules in the soft palate and tonsils that resolve without ulceration [8]. Echovirus infections: Echovirus 9 can cause intraoral lesions. Punched-out ulcers on the soft palate or tonsillar pillars and greyish-white dots are similar to Koplik’s spots and may be seen as typical enanthem in this case [5]. Similar ulcers, accompanied by a pink maculopapular dermatitis, especially on the face and trunk, are also seen in the so-called Boston exanthema [5].
f) Adenovirus infections: In infections due to human Adenoviruses, there can be upper respiratory symptoms with fever, myalgia, cough, otitis and pharyngitis, and exudative tonsillitis. There may be cervical adenopathy pharyngitis, reminiscent of the condition associated with group A streptococcal pharyngitis. Adenovirus serotypes 3, 4, and 7 may also cause a distinct syndrome consisting of conjunctivitis, pharyngitis, fever, preauricular lymphadenopathy (pharyngoconjunctival fever), and gastroenteritis [5]. In patients coinfected with EBV/CMV or other respiratory agents and Adenovirus, the maculopapular skin eruption may be associated with a nonspecific palatal petechiae [11].
g) HIV infection: More than 90% HIV infected patients can show some intraoral lesions during their course of illness [5]. Six typical lesions are frequently related to HIV infection, which are Oral candidiasis, Oral hairy leucoplakia, Kaposi’s sarcoma, necrotizing ulcerative gingivitis, linear gingival erythema, and non- Hodgkin lymphoma [12].
h) Dengue infections: Dengue is caused by DENV (Dengue virus), of which 5 serotypes are known: DENV1, DENV2, DENV3, DENV4 and DENV5. It is the most common arbovirus illness in humans [5]. About 50% of Dengue patients have a pinpoint-size vesicular enanthem with petechiae on the soft palate. The tongue is often coated with protruding red hypertrophied papillae, called the “strawberry tongue” [5].
i) Zika virus infections: Zika virus (ZIKV) is transmitted by Aedes mosquitoes and is now spread worldwide [5] . During ZIKV infection, oral lesions are mostly hemorrhagic. Petechiae and ecchymosis on the palate, gingival bleeding, and aphthous and ulcerative lesions have also been depicted in literature [13]. j) Yellow fever: In Yellow fever, which is caused by Yellow Fever virus and vector is Aedes mosquito, there may be an acute phase followed by a toxic phase [5]. In these phases, there may be oral mucosal bleeding, as well as hematemesis and bleeding of the nose and eyes. The tongue characteristically shows bright-red margins and a white furred centre [5,14] (Figure 2).
k) COVID-19 infections and enanthems: In COVID-19, there can be Painful oropharyngeal lesions which are seen mainly in the form of ulcers, blisters and gingivitis [5]. There can also be palatal petechiae, erythema, and pustules [5]. Histologic analysis, conducted in three of these patients, showed inflammatory infiltrates and focal necrotic hemorrhages in the lamina propria and, in one case, small vessel obliteration with thrombi. In children, interestingly, oral mucous membrane changes also appear to be an important finding in MIS-C or Multisystem Inflammatory syndrome in Children [15]. It can be confused with Kawasaki disease, which can present in children with Strawberry tongue [15].
Discussion
Thus, many infections by viruses can present as enanthems and oropharyngeal lesions. Clinicians and dentists hence have to be very careful about these.
Conclusion:
Many viral infections cause intraoral lesions and rashes, and they have to be inquired for and found out on examination. If needed serology or other tests can be done for these viruses.
References
- https://Rxlist.com.
- Jain P, Rathee M (2021) Koplik Spots. Stat Pearls, Treasure Island (FL): StatPearls Publishing.
- Fukuda M, Harada T, Shimizu T, Hiroshige T (2020) Forchheimer Spots in Rubella. Intern Med 59(13): 1673.
- https://dbpedia.org
- Drago F, Ciccarese G, Merlo G (2021) Oral and cutaneous manifestations of viral and bacterial infections: Not only COVID-19 disease. Clin Dermatol.
- Slots J, Saygun I, Sabeti M (2006) Epstein-Barr virus in oral diseases. J Periodontal Res 41: 235–244.
- Mullins TB, Krishnamurthy K (2020) Roseola Infantum. STAT Pearls.
- Drago F, Ciccarese G, Gasparini G (2017) Contemporary infectious exanthems: an update. Future Microbiol 12: 171–193.
- Sklavounou-Andrikopoulou A, Iakovou M, Paikos S (2004) Oral manifestations of popular-purpuric gloves and socks syndrome due to B18 V infection: the first case presented in Greece and review of the literature. Oral Dis 10: 118–122.
- Clarkson E, Mashkoor F, Abdulateef S (2017) Oral viral infections diagnosis and management. Dent Clin North Am 61: 351–363.
- Wang X, Yang K, Wei C (2010) Coinfection with EBV/CMV and other respiratory agents in children with suspected infectious mononucleosis. Virol J 7: 247–256.
- Coogan MM, Greenspan J, Challacombe SJ (2005) Oral lesions in infection with human immunodeficiency virus. Bull World Health Organ 83: 700–706.
- Sharp TM, Muñoz-Jordán J, Perez-Padilla J (2016) Zika virus infection associated with severe thrombocytopenia. Clin Infect Dis 63: 1198–1201.
- Carneiro SC, Cestari T, Allen SH (2007) Viral exanthems in the tropics. Clin Dermatol 25: 212–220.
- Ghosal Bhattacharyya S, Bhattacharyya S (2021) Oral Manifestations of Covid-19 In Children and Adults. Interventions Ped Dentistry Open Access J 5(5): 479-481.
Editorial Manager:
Email:
pediatricdentistry@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...