Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6636
Case Report(ISSN: 2637-6636) 
Treating Inflammatory Root Resorption Following Endodontic Regeneration – Case Report Volume 7 - Issue 2
Margarita Yoshpe*
Faculty of Dental Medicine Jerusalem, Hebrew University of Jerusalem, Israel
Received: February 01, 2022; Published: February 09, 2022
*Corresponding author: Margarita Yoshpe, Faculty of Dental Medicine Jerusalem, Hebrew University of Jerusalem, Israel
DOI: 10.32474/IPDOAJ.2022.07.000261
Abstract
Aim: To describe complication management following regenerative endodontics.
Introduction: Regenerative endodontic procedures (REPs) are aimed to treat apical periodontitis and promote root maturation
of immature necrotic teeth. Recently it was shown that REP may arrest inflammatory external root resorption (IERR) in replanted
avulsed teeth. The purpose of this study is to describe a complication of REP in which IERR had been developed after REP treatment.
Root Canal Treatment (RCT) using bio ceramic materials helped to arrest the IERR.
Methods: An eight-and-a-half-year-old girl was referred for treatment after avulsion of tooth #9 which has been splinted in a
hospital for 2 weeks. After thorough examination tooth #9 was diagnosed as having necrotic pulp with symptomatic apical
periodontitis. The tooth was treated by REP using plasma rich fibrin (PRF) and restored. Eight months later, IERR has begun. RCT
using trichloroacetic acid (TCA) and mineral trioxide aggregate (MTA) plug was performed. The resorption area was treated with
bio ceramic putty material.
Results: 35 months after the treatment the tooth is functioning without signs and symptoms
Conclusions: The present case demonstrate a method in which a conservative RCT with some modification may arrest IERR using
TCA. IERR may develop long time following REP treatment. A thorough long follow-up is needed after REP. An early detection of
IERR may overcome this complication.
Key learning points: Although very rare, complication after REP such as IERR may occur, an early diagnosis of such complication
may be resolved by modified conservative RCT.
Keywords: Avulsion; Bio ceramics, External inflammatory root resorption; Regenerative endodontics, Trichloroacetic acid
Introduction
Recently, regenerative endodontic procedures (REP) have
become a very popular treatment in dental trauma cases. REP is
recommended by many authors as the treatment of choice in
cases of immature teeth with necrotic pulps [1,2]. The majority of
REP cases reported in the literature have shown positive clinical
outcomes [3-5]. Success of REP is defined in AAE guidelines (6).
The degree of success of REP is largely measured by the extent to
which it is possible to attain primary, secondary, and tertiary goals.
a) Primary goal: The elimination of symptoms and the evidence
of bony healing.
b) Secondary goal: Increased root wall thickness and/or
increased root length (desirable, but perhaps not essential).
c) Tertiary goal: Positive response to vitality testing (which if
achieved, could indicate a more organized vital pulp tissue).
Additionally, tooth maturation, increased lengthening, and
thickness of the dentinal root walls as well as regaining tooth vitality
are beneficial attainable goals of REP [4-6]. However, there is no
clear consensus in the literature regarding failure definition. The
presence of signs and symptoms after RET has been identified as a
clear presentation of failure in multiple RET cases [2,7]. However,
other descriptions of reported failures may be controversial, such
as the inability to introduce blood into the canal [8-10], tooth
discoloration [11], absence of any increase in root length [12,13],
tooth fracture [14,15], and coronal leakage [16]. The complication
described in this case - IERR is a serious one, that may lead to losing the treated tooth. There is no doubt that such complication
needs an immediate intervention to make any attempt to save the
involved teeth.
Case Description
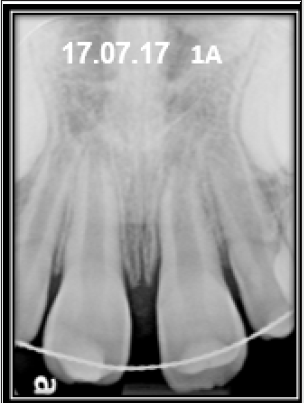
An eight-and-a-half-year-old healthy female patient was referred to our office by a general dentist for treating tooth #9 that underwent avulsion and replantation. The tooth was replanted in a hospital emergency room after it stayed 10 min in a dry condition and then 20 minutes in milk. The tooth was splinted for 2-weeks at the first appointment. Two weeks after the splint placing, clinical examination revealed normal soft tissues, negative cold test, and no sensitivity to palpation. The tooth was tender to percussion; mobility test was negative. A metallic sound could be noticed, indicative to ankylosis. Radiographic examination revealed a wide root canal space with an open apex. No periapical radiolucency was noticed (Figure 1a) The splint was removed (Figure 1b). In consecutive visits 2 and 4 weeks later no improvement to sensitivity and percussion tests were observed. A final diagnosis of necrotic pulp with symptomatic apical periodontitis was made. The parents were advised to the treatment options of apexification or REP and agreed to perform REP. An informed consent was obtained. The patient was treated under a surgical operating microscope (DOM) (Labomed, Prima, USA). At the first visit, after tooth isolation and access opening, bleeding was observed. The root canal was irrigated with NaOCl 3%, dried and dressed in calcium hydroxide for two weeks. In the subsequent visit, under local anesthetic (Lidocaine 2% 1:1000000 epinephrine; Safco, IL, Buffalo Grove, USA), the access cavity was reopened. The root canal was irrigated as above, and the calcium hydroxide was replaced for a period of 3 weeks by Trimix: a mixture of equal parts (250 mg each) of three antibiotics- Metronidazole (Sanofi-aventis, France), Cefuroxime Axetil (Zinnat,- GSK, UK), and Ciprofloxacin (Dexcel, Israel). The antibiotic tablets were crushed, then dissolved in saline to a creamy paste consistency which was introduced into the root canal by Centrix Accu Dose® 20ga Needle Tubes (Shelton, CT, USA) and endodontic B&L pluggers (Biotech, Virginia, USA) to control the insertion depth. The tooth was then temporarily restored using Interim Restorative Material (IRM, Dentsply, Sirona, Germany). Three weeks later at the third appointment, after examination and assuring that the patient was symptoms free, the final stage of the REP was performed. PRF was prepared from 40 ml of blood drawn from the patient’s cubital vein of her right forearm. A blood sample was centrifuged for 8 minutes at 1300 rpm according to the instructions [17]. Dr. Choukroun Duo Quattro PRF Centrifuge was used for the procedure. Patient was then anesthetized using Mepivacaine 3% without vasoconstrictors (Septodont, Ontario, Canada). Under rubber dam isolation, the temporary restorative material was removed, the root canal irrigated with 20 ml of 17% EDTA. After drying the root canal with paper points, the PRF was cut into small pieces and was inserted into the root canal using endodontic pluggers up to the level of the cementoenamel junction (CEJ). Resorbable Collagen Plug (Collagen Matrix, New Jersey, USA) was inserted above the PRF and covered with a bioceramic material (Biodentine, Septodont, France). The access cavity was sealed with Glass Ionomer (Fuji IX- GC, Tokyo, Japan) (Figure 1c).
Results
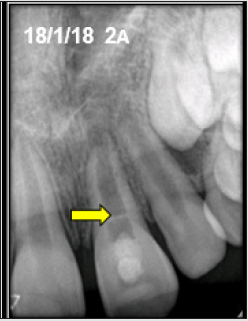
At the first follow-up appointment (3-month), the tooth was asymptomatic and tested negatively to percussion and palpation. PDL was traceable around the entire root except for around the apex. The ankylotic sound could not be detected anymore. The dentinal root canal wall at its distal aspect appeared to be a little longer and thicker and the root canal space had some radioopacities consistent with calcified tissue at the apex (Figure 2a). A dentinal bridge was noticed in the coronal third of the root. At the 8-month follow-up, the tooth continued to be asymptomatic, with a negative response to thermal and to palpation tests. There was normal sound upon percussion. However, radiographic examination revealed external resorption that destroyed dentinal bridge and coronal third of distal wall (Figure 2b). After consideration of the treatment options, it was decided to perform a conservative RCT with some modifications which included the use of TCA to cauterize the inflamed tissue and use bio ceramic material to close the pathogenic perforation that was caused by the inflammatory resorption. When the root canal was reopened, massive bleeding was observed. After rinsing the root canal with NaOCl 3%, an MTA plug (MTA; Angelus, Londrina, Brazil) was introduced just to the perforation site. The perforation site was treated by TCA 90% that was rubbed gently with micro-brush and then washed with normal saline, dried and obturated with Total Fill BC RRM (FKG Dentaire, Switzerland), which was pushed by a special spatula (G. Hartzell & Son Model # CA6CH; Spatula/Placement Instrument). The remaining root canal was obturated with gutta-percha using vertical condensation technique (B&L pluggers). BC Sealer was used (FKG Dentaire, Switzerland). The access cavity was filled with composite material (3M) (Figure 3a). Follow-up examination after 35 months revealed that IERR has been arrested. PDL is traceable around the whole root. The overfilled BC Putty in the perforation site was not resorbed completely with no inflammation around it (Figure 3b).
Figure 2B: An 8 month radiograph follow up. Notice the inflammatory root resorption on the distal wall of the root.

Figure 3B: A 35 month follow-up radiograph. Notice: The inflammatory root resorption has been arrested.

Discussion
The outcome of avulsion due to dental trauma may cause
serious complications. Often, it causes immediate loss of teeth.
When the teeth are replanted, most of the time an inflammatory
root resorption is uneventful [18-21]. Before the REP introduction
the accepted treatment for such cases was long time Ca(OH)2
dressing. Such treatment could only postpone tooth extraction but
could not avoid it. Since 2004 when Banchs and Trope introduced
the protocol for REP [22], some cases have reported the possibility
of REP to arrest inflammatory root resorption [18-21,23]. In the
case series described by Yoshpe et al. 2020 [23] some of the case
presented with ankylotic sound before the beginning of treatment.
After the REP treatment, along the follow-up period, the ankylotic
sound disappeared. The same phenomena were observed in the
present case. It had an ankylotic sound at the beginning which
disappeared at the 3 month follow up. Moreover, radiographic
examination revealed PDL surrounding the root. Up to this date the
evidence of failure rates of REP is scarce. In a systematic review
describing the failures following REP, Almutairi et al. [2] found
28 studies that reported 67 failed cases. Most of the failed cases
(91%) used blood clot as a scaffold and only 3 cases used blood concentrates in the form of platelet-rich plasma. None of the failed
cases used PRF as a scaffold. The main reason for failure was signs
and symptoms of infection.
It can be speculated that in spite of the meticulous infection
control that was taken treating this case (Trimix and Ca(OH)2), it
was imposable to eradicate the infection completely. Although
replacement resorption and ankylosis is a common finding after
tooth avulsion, Yoshpe et al. [23] demonstrated in a case series the
ability of REP to arrest ERR. However, the present case developed
EIRR observed at 8 months follow up, similar to Priya et al. [20].
who described a case of late replantation of a mature maxillary
incisor that was treated by REP using PRP as a scaffold and
developed external and Internal root resorption after 6 months.
They reopened and medicated the root canal with a long-standing
double antibiotic (minocycline and metronidazole) and succeeded
to arrest the resorption without further treatment. The treatment
strategy in this case was aimed to disinfect the root canal and
change the pH of the tissue surrounding the resorption site by
obturating it with a bio ceramic material which is known lo leach
Ca(OH)2 and thus reduce the chance of resorption continuation
[24,25]. In conclusion, it seems that most of the time REP produces
favorable results which benefit its use over the alternative MTA
apexification treatment. However, although very rare, sometimes
late postoperative complications following REP may be developed
in the form of root resorption. To overcome such complications,
it is mandatory to perform close follow-ups in the first year after
the treatment in order to diagnose any pathologic changes in its
initiation and treat them as soon as possible.
References
- Diogenes A, Ruparel NB (2017) Regenerative endodontic procedures: Clinical outcomes. Dent Clin N Am 61: 111-125.
- Almutairi W, Yassen HG, Aminoshariae A, Williams AK, Mickel A (2019) Regenerative Endodontics: A Systematic Analysis of the Failed Cases. J Endod 45(5): 567-577.
- Abu Zeid ST, Alamoudi AR Alothmani OS, Mokeem Saleh AA, Amna Y Siddiqui AY (2021) A Prospective Study of Long-Term Regenerative Endodontics Outcomes of Necrotic Immature Permanent Teeth: An 8-Year Follow-Up. Healthcare (Basel) 9(12): 1670.
- Lin J Zeng Q , Wei X, Zhao W, Cui M, Gu J, et al. (2017) Regenerative endodontics versus apexification in immature permanent teeth with apical periodontitis: a prospective randomized controlled study. J Endod 43: 1821-1827.
- Chrepa V, Joon R, Austah O, Diogenes A, Hargreaves, et al. (2020) Clinical Outcomes of Immature Teeth Treated with Regenerative Endodontic Procedures-A San Antonio Study J Endod 46: 1074-1084.
- (2016) AAE Clinical Considerations for a Regenerative Procedure.
- Meschi N, Hilkens P, Van Gorp G, Strijbos O, Mavridou A, et al. (2019) Regenerative Endodontic Procedures Posttrauma: Immunohistologic Analysis of a Retrospective Series of Failed Cases J Endod 45: 427-434.
- Lenzi R, Trope M (2012) Revitalization Procedures in Two Traumatized Incisors with Different Biological Outcomes. J Endod 38: 411-414.
- Ding RY, Cheung GS, Chen J (2009) Pulp revascularization of immature teeth with apical periodontitis: a clinical study. J Endod 35: 745-749.
- Bezgin T, Yilmaz AD, Celik BN (2015) Efficacy of platelet-rich plasma as a scaffold in regenerative endodontic treatment. J Endod 41: 36-44.
- Nagata JY, Gomes BP, Rocha Lima TF (2014) Traumatized immature teeth treated with 2 protocols of pulp revascularization. J Endod 40: 606-612.
- Nosrat A, Li KL, Vir K (2013) Is pulp regeneration necessary for root maturation? J Endod 39: 1291-1295.
- Lin LM, Shimizu E, Gibbs JL (2014) Histologic and histobacteriologic observations of failed revascularization/revitalization therapy: a case report. J Endod 40: 291-295.
- Alobaid AS, Cortes LM, Lo J (2014) Radiographic and clinical outcomes of the treatment of immature permanent teeth by revascularization or apexification: a pilot retrospective cohort study. J Endod 40: 1063-1070.
- Shimizu E, Jong G, Partridge N (2012) Histologic observation of a human immature permanent tooth with irreversible pulpitis after revascularization/regeneration procedure. J Endod 38: 1293-1297.
- Bukhari S, Kohli MR, Setzer F (2016) Outcome of revascularization procedure: a retrospective case series. J Endod 42: 1752-1759.
- Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJJ, et al. (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101: e37-44.
- Santiago CN, Pinto SS, Sassone LM, Hirata R Jr, Fidel SR (2015) Revascularization technique for the treatment of external inflammatory root resorption: a report of 3 cases. J Endod 41(9): 1560-1564.
- Chaniotis A (2016) The use of a single-step regenerative approach for the treatment of a replanted mandibular central incisor with severe resorption. Int Endod J 49(8): 802-812.
- Priya MH, Tambakad PB, Naidu J (2016) Pulp and periodontal regeneration of an avulsed permanent mature Incisor using platelet-rich plasma after delayed replantation: A 12-month clinical case Study. J Endod 42(1): 66-71.
- Saoud TM, Mistry S, Kahler B, Sigurdsson A, Lin LM (2016) Regenerative endodontic procedures for traumatized teeth after horizontal root fracture, avulsion, and perforating root resorption. J Endod 42(10): 1476-1482.
- Banchs F, Trope M (2004) Revascularization of immature permanent teeth with apical periodontitis: new treatment protocol? J Endod 30: 196-200.
- Yoshpe M, Einy S, Ruparel N, Lin S, Kaufman AY (2020) Regenerative Endodontics: A Potential Solution for External Root Resorption (Case Series). J Endod 46(2): 192-199.
- Tian J, Qi W, Zhang Y, Glogauer M, Wang Y, et al. (2015) Bioaggregate Inhibits Osteoclast Differentiation, Fusion, and Bone Resorption In Vitro. Endod 41: 1500-1506.
- Villa N, Valgas Dos Santos V, Maciel da Costa U Teixeira Mendes A, Abreu da Rosa R, Vinícius Reis Só M, et al. (2020) A New Calcium Silicate-Based Root Canal Dressing: Physical and Chemical Properties, Cytotoxicity and Dentinal Tubule Penetration. Braz Dent J 31(6): 598-604.
Editorial Manager:
Email:
pediatricdentistry@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...