Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6636
Review Article(ISSN: 2637-6636) 
SurvivalRateofResin andCeramicMini-InvasiveRestorations: A Systematic Review Volume 8 - Issue 3
Imen Kalghoum*, Oumayma Mejri, Emna boudabous, Yosra Farhat, Belhssen Harzallaha and Dalenda Hadyaoui
- Department of Fixed Prosthodontics, Research Laboratory of Occlusodontics and Ceramic, University of Monastir, Tunisia
Received: March 09, 2022; Published: March 30, 2022
*Corresponding author: Imen Kalghoum, Department of Fixed Prosthodontics, Research Laboratory of Occlusodontics and Ceramic, University of Monastir, Tunisia
DOI: 10.32474/IPDOAJ.2022.08.000289
Abstract
Purpose: to assess the 3-year survival rates and the incidences of biological and technical complications of resin and ceramic mini-invasive restorations.
Materiel and Methods: Online research of literature on PubMed and Cochrane was conducted independently by 3 reviewers to identify the clinical studies performed from 2010 up to 2022 and completed by manual research. Survival and complication rates were analyzed using robust Poisson’s regression to obtain summary estimates of 3-years prepositions. Keywords, inclusion, and exclusion criteria were well defined.
Results: the research revealed 737 titles and led to final analysis of 23 full text articles. Only 5 studies met the inclusion criteria. The meta-regression indicated that the type of ceramic material did not affect the survival rate. Estimated survival rates for glass—ceramics and feldspathic porcelain were between 75% failures were related to fractures (4%°at 3 years (n=5998 restorations). Estimated complications (3%), secondary caries (1%), failures were related to fractures (4%),followed by endodontic complications., ceramic inlays, onlays, overlays and veneers showed high survival rates at 5years and 10 years =,and fractures were the most frequent cause of failure.
Conclusion: Both ceramic and resin showed a high survival rate in mini-invasive restorations. Hybrid materials showed promising results, however, a longer clinical observation period is necessary to draw further conclusions.
Keywords: Ceramic; resin; veneers; inlay; onlay; overlay; survival rate; complication rate
Background
In the last decade, The use of tooth ceramic restorative materials has increased significantly especially With the development and improvement of reliable adhesive technologies and the augmentation of aesthetic demands [1], Therefore, minimally invasive restorations have become a field of great interest in modern restorative dentistry. This treatment preserves the tooth structure while allowing reconstruction of the destructed one to maintain correct and proper tooth functioning and also provides a satisfactory cosmetic appearance [2]. Partial indirect restorations are classified as veneers, inlays, onlays, and endocrown; those restorations can be made by numerous available resin or ceramic materials. Ceramics and resin-based composites currently are two major categories of the esthetic materials used in the production of CAD/CAM restorations. In one hand, glass–ceramics are strong due to their higher elastic modulus, and generally exhibit good mechanical and esthetic properties, however they are brittle and susceptible to chipping during the milling process. In the other hand, older composite resin milling blocks may suffer from increased material wear, loss of surface polish, and color instability but [3] Over the past decade, resin-based composites have been significantly improved due to advances in composite technology and have been expanded to CAD/CAM systems for the fabrication of indirect restorations such as inlays, onlays and veneers [4]. Differences in the mechanical properties of resin-based and ceramic materials raise the question as to which material can survive longer, and ensure the aesthetic durability at the same time [5]
This systematic review aimed to evaluate the survival rate of resin and ceramic inlays, onlays, veneers and to identify the types of complications associated with the main clinical outcomes reported in Randomized Controlled Trials, prospective studies, and in vivo studies.
Materiel and Methods
Focused questions
Our systematic review aims to answer the following questions:
a) What are the survival and complication rates of resin and ceramic inlay, onlay, overlay, veneers.
b) Are the survival rates of resin and ceramic similar after a mean observation period of at least 3 years.
c) what kind of complications we will face with resin and ceramic restorations.
Constitution of the work team and work organization
A hospital-university professor of dentistry (DH), an assistant in fixed dental prostheses department (IK) and a thesis candidate: resident in fixed dental-prostheses department (YF). The critical reading of the articles the extraction and data analysis independently, required a commitment from the members of the work team and a well coordination according to predefined schedule.
Literature research
We searched the following databases for articles: MEDLINE, THE COCHRANE CENTRAL REGISTER OF Controlled trials, and Ebsco. Initially PICOS questions defined the search strategy as follows: population, Intervention, comparison, outcomes, study type.
a) Population: Comprised patients who received resin or ceramic mini-invasive restorations.
b) Intervention: Included inlays, onlays, overlays and veneers made of resin or ceramic.
c) Comparison: Resin-ceramic mini-invasive restoration.
d) Outcomes: clinical survival rate and technical, biological, and esthetic complication rates.
e) Study: prospective studies, randomized controlled clinical trials, clinical studies.
The following MESH terms search terms and their combination were used in the MEDLINE search.
P and I: resin AND ceramic,C: inlay OR onlay OR overlay OR veneers;O: longevity) OR success) OR failure) OR survival rate [MeSH Terms]) OR clinical performance,The combination in the builder was set as “P&I AND C AND O”. The following MeSH terms, search terms, and their combinations were used in the MEDLINE search: (inlay*) OR onlay*) OR overlay*) OR veneers)) AND ((((( ceramic*) OR resin) )) AND (clinical evaluation) OR clinical trial[MeSH Terms]) AND longevity) OR success) OR failure) OR survival rate[MeSH Terms]) OR clinical performance) AND follow up study[MeSH Terms]) OR clinical study) OR comparative study)). In addition the following terms were used in the Cochrane central register of controlled trials search: ((ceramic or resin) and (inlay or onlay or overlay or veneers)
Study selection and eligibility criteria
All titles and abstracts of the selected studies were first assessed for the following inclusion criteria:
Studies with follow-up period of 3 years, Prospective studies, RANDOMIZED controlled trial, Cohorts
Studies between 2010 and 2020, Clinical studies elated to only resin and all ceramic inlays, onlays, overlays and veneers ,English studies ,Studies with clinical follow up of at least 10 patients.
Exclusion criteria
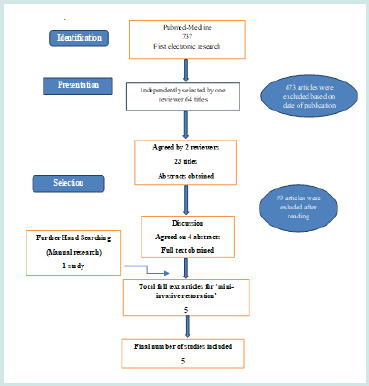
Articles with the following features without language restrictions were considered ineligible. In vitro or animal studies, Studies with a mean follow-up time less than 3 years Clinical or case report. Retrospectives studies, Studies conducted in isolated groups (bruxism, erosion, hypoplasia, others). Studies without a survival analysis on incomplete data for the analysis Studies with a dropout rate higher than 45 %; The final selection based on inclusion and exclusion criteria was made for the full text articles. For this purpose, sections on the strategy of selection were screened (Figure 1). This step was again carried out by two readers (Ik&YF) and double checked.
Critical reading of the selected articles and data extraction (Reading grid)
All the articles were fully read expect the ones excluded because of the exclusion criteria and the availability of the text. The relevant data contained in the articles selected in this study were extracted according to a predefined reading grid. The grid was developed by the working group (see appendix) and included the following information’s Study design, Patients characteristics ,Type of miniinvasive restorations, Results and effects observed, Mean follow-up time, Type of bonding materials ,Type of used materials ,Technical and biological complications, Survival rate, Failure rate.
Critical reading of selected articles
Titles and abstracts of the research were independently screened by two reviewers (IK and YF) for possible inclusions in the review. The literature on mini-invasive restorations was independently assessed by three of the reviewers (DH and IK and YF). Any disagreement regarding inclusion was resolved by discussion.
Data extraction
Data on the following parameters were extracted. Author(s), Title, Journal, Year of publication, Study design (cohort, metaanalysis, randomized controlled clinical trials, prospective case series, prospective study, and prospective clinical study). Population (Planned number of patients, sex, Age),Actual number of patients at the end of the study.
Drop-out rate, Mean age, Operators (practitioners), Material framework, Type of used material. Band name of cosmetic material. Type of mini-invasive restoration, Type of bonding material. Location of preparation, Reported mean follow –up time, Published survival rate, Reported biological complications: (caries, periodontal diseases, root-fracture),Reported technical complications: (framework fracture, minor chipping, major chipping), Esthetic complications, Specificity of the study. Based on the included studies, the survival rate of each mini-invasive restoration was calculated. In addition, the number of events for all technical and biological complications was extracted and the corresponding number total exposure of the reconstruction was calculated. Data was extracted independently by two reviewers (Ik & YF) using data extraction form. Disagreement regarding data extraction was resolved by consensus of three reviewers (DH & IK & YF).
Statistical analysis
The definition of survival is that the tooth supported miniinvasive restoration remains in situ with or without modification during the observation period. Restoration success is the demonstrated ability of a restoration to perform as expected without modification. Failures included every type of complication that led to the removal or the replacement of the restoration or the loss of the tooth. Complication may lead or not to failure. Failure and complication rates were calculated by dividing the number of events (failure or complication) in the numerator by the total tooth supported mini-invasive restoration exposure time in the denominator. The numerator could usually be extracted directly from the publication the total exposure time was calculated by talking the sum of:
a) Exposure time of tooth-supported mini-invasive restoration that could be followed for the whole observation time.
b) Exposure time up to failure of the tooth-supported miniinvasive restoration that were lost due to failure during the observation time.
c) Exposure time up to the end of observation time for toothsupported mini-invasive restoration that did not complete the observation period due to reasons such as death, change of address, refusal to participate, non-response, chronic illnesses, missed appointments and work commitments
For each study, event rates for the tooth-supported mini-invasive restoration were calculated by dividing the total number of events by the total tooth-supported mini-invasive restoration exposure time in years. The total exposure was determined by multiplying the total number of tooth-supported mini-invasive restoration by the mean follow –up time, no more precise information. For further analysis, the total number of events was considered to be Poisson , disturbed for a given sum of tooth-supported miniinvasive restoration exposure years and Poisson regression with a logarithmic link-function with a total exposure time per study as an offset were used. Robust standard errors were calculated to obtain 95% Confidence intervals of the summary estimates for the event rates. To assess heterogeneity of the study specific event rates, the Spearman goodness-of-fit statistics and associated p-value were calculated. If the goodness-of-fit p-value was below 0.05 three year survival; proportions had been calculated via the relationship between event rate and survival function S, S (T) = exp (-T*event rate), by assuming constant event rates. The 95% CONFIDENCE intervals for the survival proportions were calculated by using the 95% CONFIDENCE LIMITS of the event rates. Multivariable Poisson regression was used to formally compare construction subtypes and to assess other study characteristics. All analyses were performed using stata version 13.1.
Results
The strategy of the selected articles epitomizes the approach taken during this study. The research on MEDLINE using the Boolean-equation has identified 737 articles. The research on Cochrane and EBSCO has identified the same articles founded with PubMed search so duplicate was eliminated. During the preselecting step, 637 articles were excluded based on titles. After reading, other 41 articles were excluded based on other excluded criteria that we mentioned earlier in the study. Among the 23 selected articles, only 4. corresponded to studies on tooth-supported mini-invasive restoration. One study was included from hand searching [1]. Figure 1 describes the process of identifying the 5 full text articles selected from an initial yield of 737 that were found published from the 2010 up to 2020. Among the 5 selected articles, 2 prospective clinical studies; two randomized split-mouth clinical trials, one clinical trials and one longitudinal clinical evaluation.
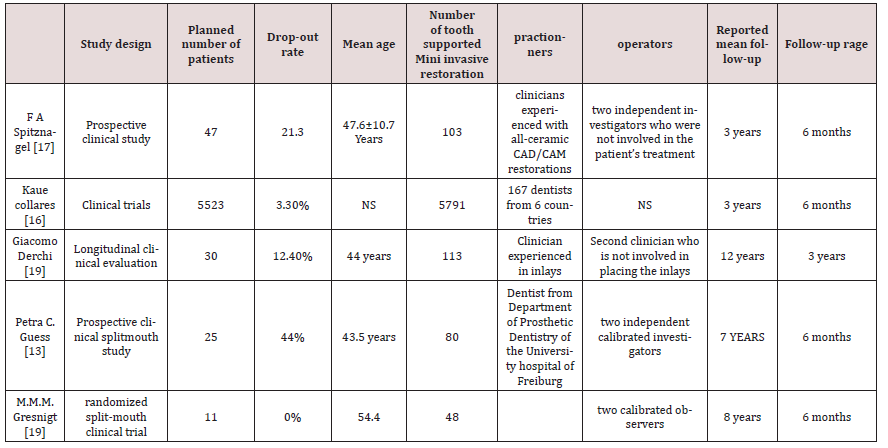
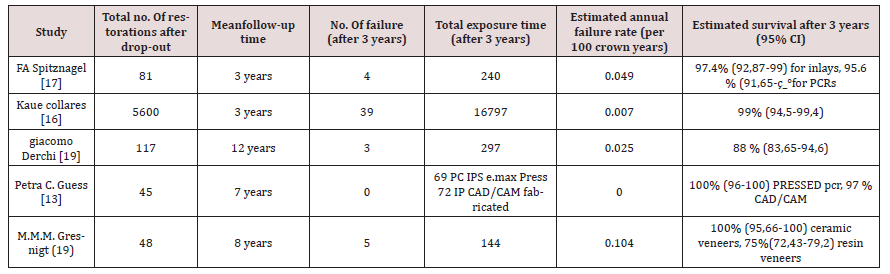
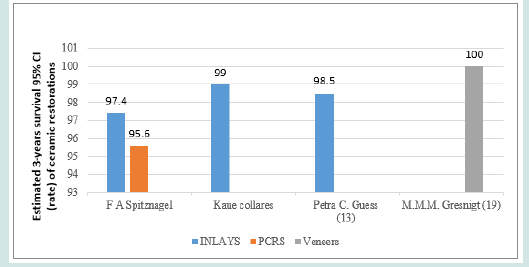
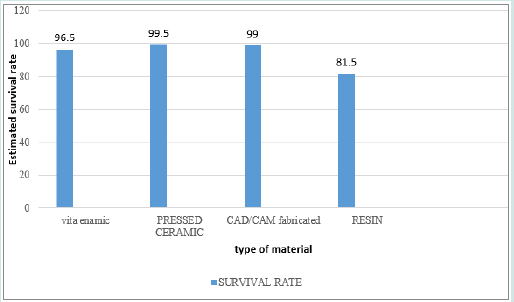
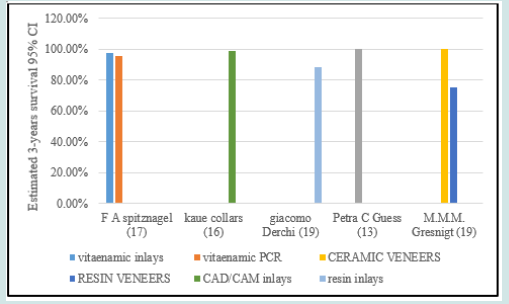
The articles included in this study are listed in Table 1 by author, study design and patient characteristics. (Table 1). The 5 clinical studies included two 3 years follow-up , one 7 years follow-up, one 8 years follow-up and one 12 years follow-up (Table 2). For ceramic group 5894 inlays were clinically followed on 3 years, 80 inlays on 7 years and 24 veneers on 8 years with a mean follow-up time of 3 years +/- 6 months for a total number of 5998 ceramic mini-invasive restorations (Table 3 & Figure 2). For resin group 113 inlays clinically followed on 12 years and 24 veneers on 8 years with mean follow-up time of 11 years +/- 6 months for a total number of 137 restorations. Out of these studies one use polymer infiltrated ceramic , one study compared leucite glass ceramic and lithium disilicate glass ceramic, one study compared two types of resin Cingum and kuzlar, one compared ceramic IPS empress and resin Estenia and the last one compared CAD-CAM system and pressed ceramic (Table 1 & Figure 3 ). The different types of ceramic used during the various studies was as follows: feldspathic porcelain (FP), leucite glass ceramic (LD), lithium disilicate glass ceramic (LEU) and pressed ceramic (IPS Empress) (Figures 3 & 4). The studies included patients between the age of 42 and 60. The proportions of patients who could not be followed for complete studies periods or at least 3 years were calculated for all studies as a drop-out rate and ranged from 0% and 44% (Table 2). In all included studies, preparation guidelines according to the manufacturer’s recommendation were considered. Different measurement methods were used to examine the mini-invasive restoration at the recall appointments; in order to identify the technical and biological complications.
Restoration survival
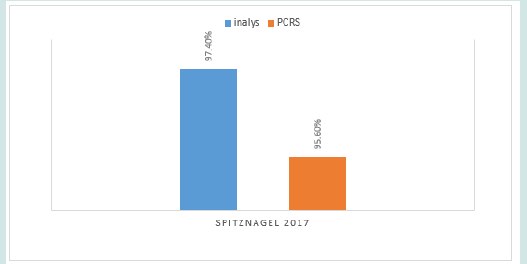
Overall, in the 4 studies reporting ceramic group with a mean follow-up of 3 years+/- 6 months. An estimated failure rate of 0.028 was reported, translated into an estimated 3-year survival of ceramic restoration of 98% (Figure 2). In comparison, all resin restorations had an annual failure rate ranging between 0.025 and 0.104, translating into overall estimated 7 years survival rates ranging between 75% and 88%. This was based on 2 studies. The survival rates of ceramic restorations differed for the various types of ceramics. One study used vitaenamic and rended an estimated 3 year survival rate of 97.4 % for inlays and 95.6% FOR PCRS.
Technical and Biological Complications
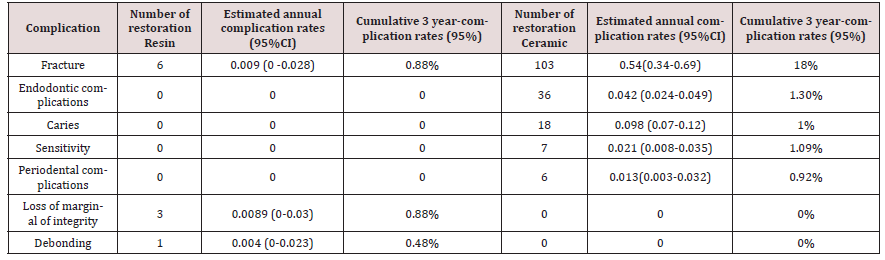
Table 3 displays a summary of biological and technical complications, the solution and the failures for ceramic and resin restorations. Table 1 display an overview of the incidences, the estimated annual complication rates and the cumulative 3-years complication rates of technical and biological complications for ceramic and resin as well as the statistical differences between the restoration types.
Technical complications
Loss of marginal integrity, marginal discrepancy, minor chipping, fracture , the marginal adaptation and the anatomical form according to the USPHS criteria (Table 3) and described as bravo (B). The solutions adopted for the different technical complications were (Table 1). A clinical check-up for the non-marginal adaptation was adopted as a solution for 4 cases reported as inlays made from resin during a mean follow-up time of 3 years in one study [27]. Minimal fracture was reported in one study [30] and the polishing of ceramic was the solution to adopt. The restoration fracture was reported as a failure and the restoration replacement was needed. Charlie and delta criterion according to the USPHS criteria were reported as failure and the loss of crown was a fact. 108 restorations were lost by fracture: 4 of them made by vita enamic [26] (Figures 5), 98 made from feldspathic porcelain [28] and 6 others made from resin [27]. The restoration replacement due to marginal discrepancy was reported in one study [27] the solution was the replacement of the restoration, and the material is resin.
veneer is debonded and the accurate solution was rebonding [30]. Fracture was the most frequent technical complication with a cumulative 3-years event rate of 18% (95% CI:12.43-19.05). Fracture also occurred for resin group with a cumulative 3-year complication rate of 0.88%; (95% CI: 0-2.69%). Debonding (cumulative 3-years event rate of 0.48% (95% CI: 0-3.69%) and loss of marginal integrity (cumulative 3-years event rate of 0.88% (95% CI:0-2.69%)) occurred in the resin group only. For the USPHS (Table 2) the criterions Bravo, Charlie and Delta were considered as technical complications that leaded to clinical control, intervention, and loss of the restoration respectively.
Biological complications
Loss of tooth vitality, endodontic and periodontal infection, recurrent caries lesions, were reported as biological complications for mini-invasive restoration. The solutions adopted for different biological complications were: (Table 3). Root treatment for teeth with ceramic inlays/onlays [28] and resin inlays [27]. A periodontal treatment was adopted for the several periodontal infections and diseases on 3 ceramic inlays [28]. Eleven cases were reported for recurrent caries treatment on tooth supporting ceramic inlays [28]. The tooth fracture and the extraction due to infection were not observed. According to Table 2 secondary caries and endodontic complication were common biological complication and the most frequent for ceramic inlays (3-yearcomplication rate 1.3% CI: 0.1-1). Finally, sensitivity is found for the resin group and showed a cumulative 3-years complications rate of 0.72 CI: 0.65- 0.98). According to the study, secondary caries, endodontic and periodontal diseases, and loss of tooth vitality for prosthodontics reasons were the most common biological complications for resin and ceramic mini-invasive restorations.
Discussion
This systematic review assessed the survival rate of miniinvasive restoration by comparing resin and ceramic with minimal follow-up time of 3years and focused on the results of prospective clinical studies and case series that would compare head-tohead resin and ceramic in mini-invasive restorations along with a randomized controlled trial. Database search revealed the presence of controlled randomized trials which are studies at the top of pyramid of levels of scientific evidence. Retrospective and in vitro studies, narrative review, case and clinical reports and studies with a mean follow-up period less than 3 years were excluded to summarize the available information about survival and complication rates of mini-invasive restorations after a period of at least 3 years. Retrospective studies are eliminated because of the limited control the investigator has over data collection furthermore the existing data may be incomplete, inaccurate, or inconsistently measured between subjects. Even with follow-up time of at least 3 years. Some clinicians may argue that such a period is still too short to obtain reliable information on survival and complication rates. It should be mentioned at this point that survival is defined as the number (or percentage) of restorations that remain in situ, with or without modification.
The interest of our systematic review is to compare two types of material (ceramic vs resin) used in mini-invasive restorations in order to find out the one with better survival rate and less complications as well as patient satisfaction. The research was carried out methodically according to CONSORT standards. This search identified a total of 5 articles; the number of articles is considered sufficient and allowing for a systematic review. The risks of bias of the selected studies were analyzed according to the Cochrane collaboration. The methodology was then accepted, and the studies were then included in the systematic review. One of the most important and longest parts of a systematic review is to extract the data from these studies. The data extraction grid developed is at the appendix. This systematic review assessed the survival rate of mini-invasive restorations made by ceramic and resin with minimal follow-up period of three years. The mini-restorative treatments examined in the studies included in this systematic review were performed in both males and females and in a very wide range of ages, covering the whole spectrum of adultery. As it is known, both sex and age are probably the most confounding variables in medical/dental studies, as they are associated with exposures of interest, such as diet, muscular strength and oral hygiene [32]. Studies that included patients with bruxism problem are exculed from this review due to the fact that bruxism is associated with a higher complication rates. In fact a systematic review on bruxism and prosthetic treatment by Johansson et al has shown that bruxism is associated with an increased rate of mechanical and technical complications [33].
In the 5 included studies the biggest number of restorations was evaluated by Kaus collaress et al. who have reported on 5791 restorations, while the longest evaluation period was accomplished by giacomo Derchi et al. [27] who reported for a period of up to 12 years. This systematic review showed a high survival rate for both resin and ceramic group for a period of at least 3 years followup time that exceeded 80% in the 5 included studies which is in correlation with S.Morimoto and et al. systematic review [5]. The high survival rate of mini-invasive restorations in our systematic revue is in agreement with the literature, Sampaio FBWR et al. found estimated survival rates for CAD/CAM of 97% after five years [34].However the review of Rodrigues et al. included studies on CAD/CAM materials for single crown, multiple- unit or partial ceramic crown with a 24 to 84-month follow-up based on the longevity and failures rates, suggesting that the longevity of CAD/ CAM partial restorations is lower compared to the conventionally fabricated restorations [35]. These results were assessed based on the restoration type, given higher success rates for the overall clinical performance in full crown reconstructions compared to partial crowns. Similar data were found for survival rates of full crowns, estimated 5-year survival rate for leucite or lithium disilicate reinforced glass ceramic (96.6%) and sintered alumina and zirconia (96%) were similar [36]. On the basis of this review as well as other previous systematic reviews on this subject, there is a lack of clinical evidence for survival on the best fabrication technique (CAD/CAM, pressable and stratified).
Another study that examined the survival of ceramic inlay/onlay restorations is kaus Collares et AL practice research network .The main finding of this study is that ceramic inlay/onlay restorations have a good survival rate which are comparable to our findings and with other prospective studies on ceramic restoration. However, we could identify three risk factors that can lead to restorations failure which were position of restoration cervical outline , use of a glass ionomer liner and type of adhesive .It has been shown that the risk factors for survival were deep cervical cavity outline related to the more reliable bond to enamel compared to dentin also presence of a glass ionomer lining cement [37]. In this systematic review, pressed ceramic and CAD/CAM all ceramic partial coverage restorations the pooled estimated survival rate was 100% for pressed ceramic and 97% for CAD/CAM for 3 years of follow-up yet this was not a significant difference (p=0.091). One explanation for the similar performance of pressed-ceramics and CAD/CAM porcelain could be the adhesive cementation that likely compensated for the mechanical differences between the 2 ceramic materials [30].
In Marco M.M Gresnigt study which compared indirect composite resin and ceramic veneers the number of absolute failure was limited to one debonding and 2 cohesive fractures that occurred only in the composite laminate veneers leading to an annual survival rate of 100% for the ceramic group and 87% for resin group which did not show significant differences (p > 0.05; Kaplan Meier log Rank (Mantel-cosd. CI = 95% ) which is in correlation with our results (p=0.087) .To the authors this is the first randomized controlled clinical study where both material were compared in the same patient so based on the non-significant differences in the clinical survival of two materials the nul hypothesis could be accepted ,however, some of the findings could provide insight into the long term performance of the two materials tested .In fact , surface quality changes were more frequently observed in the composite veneer material which may require more maintenance over time and also may lead to the replacement of the restoration.
These findings are in correlation with our present review, in fact, the meta-analysis indicated low complication rates. Apparently, strong, and durable adhesion of resin cements to both ceramic and resin increased the survival rate. The tooth-ceramic bond ensures re-establishment of tooth strength. After an observation period of 3 years, the lowest annual failure rates were seen for pressed ceramic PCRs (0 per 100 SCs years). Multivariable random-effect Poisson’s regression showed that resin veneers has significantly higher annual failure rates of about 0.104 per 100 SCs years. Furthermore the analyzing study reporting on ceramic inlays with a mean follow-up time of 3 years had expressed an annual failure rate about 0.028 per 100 SCs years, translating into 3-year survival rate of 98%. According the Derchi et AL twelve years longitudinal clinical evaluation of bonded indirect composite resin inlays, they are reliable options for long term function in posterior region, According to the authors up to 3 years the surface texture, marginal integrity and restoration integrity were acceptable and did not show significant difference.
Hybrid materials
In one study ,included in this review spitznagel and al studied the survival rate of Polymer-infiltrated ceramic CAD/ CAM inlays and partial coverage restorations over 5 years which showed promising results with survival rates of 97.4 and 95.6%, respectively [26]. As there are no controlled clinical trials of VITA Enamic in the literature available yet, comparisons to other clinical studies are only possible to a limited extent. Variations in material selection, as well as clinical treatment procedure and study design have to be taken into account [38].
Limitation
Differences in settings (universities vs private dental clinics), treatment protocols, experience, age and clinical skills of operators, periodontal factors, tooth history and extent of tooth destruction prior to restoration make the drawing of definitive conclusions very difficult. However, it is encouraging that according to most authors, mini-invasive restorations present high survival rates for the first 3 years, exceeding 80%. Unfortunately, the authors of all papers did not provide information about the location of the restorations which failed. This is a very important issue, as the literature suggests that both biological and technical complications may be associated with the location of the restorations. According to the findings of this systematic review, a great heterogeneity of the methodological data between studies with lack of properly comparisons (control and study groups), no homogeneous restoration material type groups and a short follow-up examination was observed. More homogeneous studies with the more comparable materials, manufacturing techniques and CAD/CAM software system with a control group in a split-mouth randomized controlled study design should be conducted.
Conclusion
within the limitations of this systematic review ceramic and resin mini-invasive restorations showed favorable survival rate after at least 3 years. This meta-analysis indicates that the survival rate remains high regardless of the ceramic material, study design, and study setting. Our results indicate that fractures remain the most frequent type of failure and the type of tooth does not seem to affect survival rates. Clinicians should note that gaps in clinical evidence exist for the justification of resin composites compared with ceramics when restoring teeth with mini-invasive restorations. Particle-filled composite resin CAD/CAM materials might be promising for single-tooth restorations because of their advantageous material characteristics however a longer clinical observation period is necessary to draw further conclusions.
References
- Guess PC, Schultheis S, Wolkewitz M, Zhang Y, Strub JR (2013) Influence of preparation design and ceramic thicknesses on fracture resistance and failure modes of premolar partial coverage restorations. J Prosthet Dent 110(4): 264-273.
- Wayakanon K (2017) Partially Coverage Restoration: An Esthetically Conservative Treatment for a Complex Cavity Restoration. Open J Stomatol 7(4): 234-241.
- Awada A, Nathanson D (2015) Mechanical properties of resin-ceramic CAD/CAM restorative materials. J Prosthet Dent 114(4): 587-593.
- Ling L, Ma Y, Malyala R (2021) A novel CAD/CAM resin composite block with high mechanical properties. Dent Mater 37(7): 1150-1155.
- Morimoto S, Rebello de Sampaio FB, Braga MM, Sesma N, Özcan M (2016) Survival rate of resin and ceramic inlays, onlays, and overlays: a systematic review and meta-analysis. J Dent Res 95(9): 985-994.
- Mangani F, Marini S, Barabanti N, Preti A, Cerutti A (2015) The success of indirect restorations in posterior teeth: a systematic review of the literature. Minerva Stomatol 64(5): 231-240.
- Beier US, Kapferer I, Burtscher D, Dumfahrt H (2012) Clinical performance of porcelain laminate veneers for up to 20 years. Int J Prosthodont 25(1): 79-85.
- Fron Chabouis H, Smail Faugeron V, Attal JP (2013) Clinical efficacy of composite versus ceramic inlays and onlays: a systematic review. Dent Mater 29(12): 1209-1218.
- Petridis HP, Zekeridou A, Malliari M, Tortopidis D, Koidis P (2012) Survival of ceramic veneers made of different materials after a minimum follow-up period of five years: a systematic review and meta-analysis. Eur J Esthet Dent 7(2): 138-152.
- Klink A, Huettig F (2013) Complication and survival of Mark II restorations: 4-year clinical follow-up.
- Aboushelib MN, Elsafi MH (2016) Survival of resin infiltrated ceramics under influence of fatigue. Dent Mater 2016 32(4): 529-534.
- Yildiz C, Vanlıoğlu BA, Evren B, Uludamar A, Kulak-Ozkan Y (2013) Fracture resistance of manually and CAD/CAM manufactured ceramic onlays. J Prosthodont 22(7): 537-542.
- Yu WQ, Yu M, Yao LL, Wang CH, Wang M, Fan C (2018) Comparison of clinical efficacy of CAD/CAM all -ceramic inlay and polymerid porcelain inlay in restoration of posterior Class II cavity. Shanghai Kou Qiang Yi Xue 27(1): 61-64.
- Homsy FR, Özcan M, Khoury M, Majzoub ZAK (2018) Comparison of fit accuracy of pressed lithium disilicate inlays fabricated from wax or resin patterns with conventional and CAD-CAM technologies. J Prosthet Dent 120(4): 530-536.
- Pott P, Rzasa A, Stiesch M, Eisenburger M (2016) Marginal fit of indirect composite inlays using a new system for manual fabrication. Eur J Paediatr Dent 17(3): 223-226.
- Hooshmand T, Rostami G, Behroozibakhsh M, Fatemi M, Keshvad A, van Noort R (2012) Interfacial fracture toughness of different resin cements bonded to a lithium disilicate glass ceramic. J Dent 40(2): 139-145.
- Piwowarczyk A, Schick K, Lauer HC (2012) Metal-ceramic crowns cemented with two luting agents: short-term results of a prospective clinical study. Clin Oral Investig 16(3): 917-922.
- Belli R, Geinzer E, Muschweck A, Petschelt A, Lohbauer U (2014) Mechanical fatigue degradation of ceramics versus resin composites for dental restorations. Dent Mater 30(4): 424-432.
- Grivas E, Roudsari RV, Satterthwaite JD (2014) Composite inlays: a systematic review. Eur J Prosthodont Restor Dent 22(3): 117-124.
- Melilli D, Cumbo EM, Baldissara P, Wandscher VF, Valandro LF, Gallina G, et al. (2018) Evaluation of marginal leakage after mechanical fatigue cycling of composite inlays luted with different cements. Gen Dent 66(4): 51-55.
- Cal E, Celik EU, Turkun M (2012) Microleakage of IPS empress 2 inlay restorations luted with self-adhesive resin cements. Oper Dent 37(4): 417-424.
- Fron Chabouis H, Prot C, Fonteneau C (2013) Efficacy of composite versus ceramic inlays and onlays: study protocol for the CECOIA randomized controlled trial. Trials 14: 278.
- Rajagopal P, Chitre V, Aras MA (2012) A comparison of the accuracy of patterns processed from an inlay casting wax, an auto-polymerized resin and a light-cured resin pattern material. Indian J Dent Res 23(2): 152-156.
- Cubas GB, Camacho GB, Pereira-Cenci T, Nonaka T, Barbin EL (2010) Influence of cavity design and restorative material on the fracture resistance of maxillary premolars. Gen Dent 58(2): 84-88.
- Edelhoff D, Güth JF, Erdelt K, Brix O, Liebermann A (2019) Clinical performance of occlusal onlays made of lithium disilicate ceramic in patients with severe tooth wear up to 11 years. Dent Mater 35(9): 1319-1330.
- Spitznagel FA, Scholz KJ, Strub JR, Vach K, Gierthmuehlen PC (2018) Polymer-infiltrated ceramic CAD/CAM inlays and partial coverage restorations: 3-year results of a prospective clinical study over 5 years. Clin Oral Investig 22(5): 1973-1983.
- Derchi G, Marchio V, Borgia V, Özcan M, Giuca MR,et at. (2019) Twelve-year longitudinal clinical evaluation of bonded indirect composite resin inlays. Quintessence Int 50(6): 448-454.
- Collares K, Corrêa MB, Laske M (2016) A practice-based research network on the survival of ceramic inlay/onlay restorations. Dent Mater 32(5): 687-694.
- Gresnigt MMM, Cune MS, Jansen K, van der Made SAM, Özcan M (2019) Randomized clinical trial on indirect resin composite and ceramic laminate veneers: Up to 10-year findings. J Dent 86: 102-109.
- Guess PC, Selz CF, Steinhart YN, Stampf S, Strub JR (2013) Prospective clinical split-mouth study of pressed and CAD/CAM all-ceramic partial-coverage restorations: 7-year results. Int J Prosthodont 26(1): 21-25.
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, et al. (2011) Cochrane handbook for systematic reviews of interventions. Chichester: John Wiley & Sons.
- Richards D, Clarkson J, Matthews D, Niederman R (2008) Evidence-based dentistry: managing information for better practice. Quintessence publishing, London, UK.
- Johansson A, Omar R, Carlsson GE (2011) Bruxism and prosthetic treatment: a critical review. J Prosthodont Res 55(3): 127‐
- Sampaio FBWR, Özcan M, Gimenez TC, Moreira MSNA, Tedesco TK, et al. (2019) Effects of manufacturing methods on the survival rate of ceramic and indirect composite restorations: A systematic review and meta-analysis. J Esthet Restor Dent 31(6): 561-571.
- Rodrigues SB, Franken P, Celeste RK, Leitune VCB, & Collares FM (2019) CAD/CAM or conventional ceramic materials restorations longevity: a systematic review and meta-analysis. Journal of Prosthodontic Research.
- Sailer I, Makarov NA, Thoma DS, Zwahlen M, Pjetursson BE (2015) All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs). Dent Mater 31(6): 603-623.
- Fron Chabouis H, Smail Faugeron V, Attal JP (2013) Clinical efficacy of composite versus ceramic inlays and onlays: a systematic review. Dent Mater 29(12): 1209-1218.
- Cobankara FK, Unlu N, Cetin AR, Ozkan HB (2008) The effect of different restoration techniques on the fracture resistance of endodontically-treated molars. Oper Dent 33(5): 526-533.
Int J Prosthodont 26(3): 272-276.
Editorial Manager:
Email:
pediatricdentistry@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...