Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6636
Case Report(ISSN: 2637-6636) 
Surgical Management of Intruded Permanent Incisors: A Case Report with 10-year Follow Up Volume 8 - Issue 3
Antoine Berberi1*, Georges Aad2, Hassan Dib1, Albert Waked1 and Nabih Nader1
- 1Department of Oral and Maxillofacial Surgery, Faculty of Dental Medicine, Lebanese University, Lebanon
- 2Department of Oral Medicine and Maxillofacial Radiology, Faculty of Dental Medicine, Lebanese University, Lebanon
Received: February 02, 2022; Published: February 10, 2023
*Corresponding author: Berberi Antoine, Department of Oral and Maxillofacial Surgery, Dental Faculty, Lebanese University, Lebanon
DOI: 10.32474/IPDOAJ.2023.08.000286
Abstract
Traumatic intrusion is an accident that leads to luxation of the tooth that will be displaced along the vertical axis toward the alveolar bone. This injury is regarded as serious because of the damage that it causes to the peri-dental and dental tissues. The traumatic movement is associated with severe damage to the periodontal ligament, pulpal tissue, root, and alveolar bone. The purpose of this paper is to describe the surgical repositioning approaches used in cases of intrusion injury in association with orthodontic repositioning. This report describes the surgical-orthodontic treatment of intruded permanent maxillary incisors following trauma in an 11-year-old boy. The clinical and radiographic examination ten years after treatment revealed no sign of pulp necrosis, root resorption or ankylosis.
Keywords: Trauma; Surgical repositioning; Orthodontic extrusion; Incisor; Maxilla
Introduction
Traumatic dental accidents occur more frequently in childhood, both in primary and permanent dentition, with an incidence rate of 25-30% in children and young people [1]. In mixed dentition, trauma to the orofacial sphere directly affects the maxillary and sometimes lower incisors which can lead to their intrusion and 0.3- 1.9% of the traumatic injuries seen in permanent teeth and males are more affected than females (M:F = 3:2) [2]. Depending on the degree of intrusion, severe complications can result pulp necrosis, root resorption, ankylosis and loss of marginal bone support [3]. The optimal treatment of these re-impacted permanent incisors remains a controversial subject, however the literature suggests a simple observation hoping for spontaneous re-eruption, surgical repositioning, orthodontic extrusion, or a combination of the last two [3-6].
Case Report
The 10-year-old patient was referred to our clinic 24 hours after a consultation in the hospital emergency room following a fall on a staircase. The questioning of the parents reveals that the child is in good general health. The intraoral examination revealed a fracture of the buccal alveolar bone of the maxillary left incisor (21) with a coronary fracture of the mesial angle of maxillary right incisor (11) and degree 2+ mobility (Figure 1). The panoramic x-ray confirms the apical displacement of both left and right incisors (11 and 21) whose apices are closed, and no root fracture was noted (Figure 2). The thermal pulp vitality tests on these incisors are positive and the latter show no pain on percussion. The recommended treatment is immediate fixation of the teeth followed by orthodontic extrusion. For this, buttons are glued to the vestibular faces of 11, 21, and 22 using a self-curing composite, thus allowing their coronal traction. After six weeks, we notice the evolution of 11 and 22 up to the occlusal plane and a minimal displacement is observed at the level of 21 located at the level of the nasal floor Indeed, an increase in the intensity of the force at the level of the 21 can bring the tooth back to the arch but with absence or lack of attached gingiva. We then observe a difference in gingival height between 11 and the adjacent teeth (Figures 3a & 3b).
Figure 3: After six weeks, we notice the evolution of 11 and 22 up to the occlusal plane and a minimal displacement is observed at the level of 21 located.

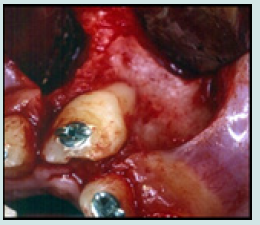
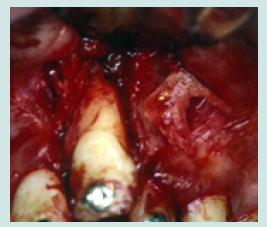
Thus, a surgical extrusion was decided and discussed with the parents. Under local analgesia (xylocaine with adrenaline 2%), a flap is drawn. The incision extends from the collar of 21 and 22 with two relief incisions. A muco-periosteal flap is reflected, and buccal bone was drilled and separated, using a conical carbide bur 0.6 on surgical hand piece, to be able to displace it with the tooth coronally. The alveolar bone is lifted. The tooth is pulled towards the alveolar ridge by a sliding motion. The alveolar bone is repositioned coronally around the neck of the tooth in its new position. The tooth is stabilized in place by an orthodontic wire and a metal grid, and everything is bonded with composite. The flap is sutured in place with 3 0 silk threads and an intra- oral radiograph was taken for the follow-up period (Figures 4a-4e). Medication is prescribed for the patient based on amoxicillin 500 mg 4 times a day and an analgesic based on paracetamol as needed and mouthwashes based on gluconate 0.12% chlorhexidine.
Figure 6: The horizontal and vertical osteotomy to note the intact nasal spine and the displacement alveolar bone.
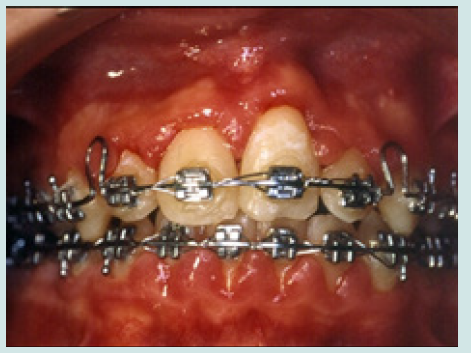
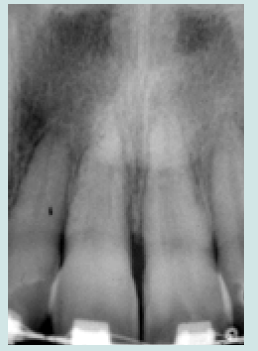
The sutures are removed ten days later, and the patient is followed up monthly. Subsequently, the patient is taken care of by his orthodontist. Conventional attachments are glued in the ideal place at the level of all the teeth and flexible nickel-titanium memory arch wires will allow the final positioning of the intruding teeth on the arch (Figures 5a & 5b). Two years later the orthodontic appliance was removed, a twisted wire bonded to the maxillary central incisors using a light-curing composite was placed to prevent their intrusion and an intra-oral radiograph was taken and showed no bone or root resorbtion (Figures 6a-6c). Ten-years later the re-impacted incisors reveal no signs of pulp necrosis, root resorption or ankylosis. Only periodontal plastic surgery was done to achieve a better gingival tissue alignment (Figures 7a & 7b).
Discussion
In our case, our therapeutic decision was to start orthodontic extrusion immediately and not to wait for a spontaneous reeruption. Moreover, [2] reports that immature teeth can erupt spontaneously, while teeth with a closed apex must be repositioned orthodontically. Similarly, waiting for a spontaneous re-eruption may increase the risk of ankylosis and pulp resorption may progress silently, and it is unable to intervene endodontically [7,8]. Similarly, Turkley et al. found that dislocation of intruded teeth before the application of orthodontic force prevents ankylosis in dogs [9]. However, orthodontic extrusion requires a long treatment with a long retention period and critical patient cooperation [10,11]. Surgical repositioning may be an alternative to orthodontic extrusion [12], but surgically repositioned teeth present more problems with root resorption, ankylosis and loss of marginal bone support [11-14]. The latter can be indicated only when the teeth are moved into the vestibule through the floor of the nasal cavity [13].
The diagnosis is critical immediately after a trauma, especially since the techniques used to assess the dental pulp and the periodontal health of the re-impacted teeth are limited [12] (radio, electrical test, percussion, color).In general, the prognosis of intruded teeth following trauma is poor because those with a closed apex have a 100% incidence of pulp necrosis while those with an immature apex have an incidence of 63%. Similarly, the incidence of ankylosis is approximately 24% [13,14]. Indeed, the factors predisposing to pulp necrosis are: the depth of the intrusion, the stage of root development (mature apex), and the coronary fracture [14].In our case, the prognosis is considered good because the patient does not present to date (3 years later) any sign of pulpal necrosis, ankylosis and root resorption despite the existence of risk factors (severity of the trauma, closed apex, coronary fracture). Indeed, minimal surgical manipulation made it possible to obtain good periodontal health at the level of 21 and a repositioning of the apical alveolar bone towards the lost vestibular table.
Conclusion
Our young patients very often present lesions of all kinds following a shock to the teeth which are not always well apprehended by the attending practitioner. A multidisciplinary approach is often essential. The motivation of the patient and the parents and interdisciplinary cooperation contributed to the success.
Acknowledgement
The authors do not have any financial interest, either directly or indirectly, in the products or information listed in this paper.
Funding
None
Competing Interests
None.
References
- CullyJ L, Zeeb K, Sahay RD, Gosnel lE, Morris H, Thikkurissy S (2019) Prevalence of Primary Teeth Injuries Presenting to a Pediatric Emergency Department. Pediatr Dent 41(2): 136-139.
- Andreasen JO, Bakland LK, Matras RC, Andreasen FM (2006) Traumatic intrusion of permanent teeth. Part 1. An epidemiological study of 216 intruded permanent teeth. Dent Traumatol 22(2): 83-89.
- Pithon MM (2021) Conservative treatment in adult patients with reimplanted anterior teeth after traumatic avulsion with extensive bone loss: an 8-year follow-up. Dental Press J Orthod 26(1): e21bbo1.
- Rovira-Wilde A, Longridge N, Mc Kernon S (2021) Management of severe traumatic intrusion in the permanent dentition. BMJ Case Rep 14(3): e235676.
- Pinto LCC, Antunes LS, Valente MIB, Lenzi M, Antunes LAA, Gomes CC (2017) Intrusive luxation of an immature permanent incisor: a 10-year follow-up. Gen Dent 65(3): e21-e24.
- Rai P, Pandey RK, Khanna R (2016) A multidisciplinary approach to the management of traumatic intrusion in immature permanent teeth. BMJ Case Rep 2016: bcr2014208571.
- Hurley E, Stewart C, Gallagher C, Kinirons M (2018) Decisions on repositioning of intruded permanent incisors; a review and case presentation. Eur J Paediatr Dent 19(2): 101-104.
- Kim HJ, Kim YI, Min KS (2017) A combined approach with passive and active repositioning of a traumatically intruded immature permanent incisor. Eur J Paediatr Dent 18(1): 27-31.
- Turley PK, Crawford LB, Carrington KW (1987) Traumatically intruded teeth. Angle Orthod 57(3): 234-44.
- Mota Júnior SL, Azevedo DGR, Campos MJDS, Tanaka OM et al. (2021) Orthodontic treatment after intrusive dislocation and fracture of the maxillary central incisors. Am J Orthod Dentofacial Orthop 160(5): 757-763.
- Sönmez H, Tunç ES, Dalci ON, Saroglu I (2008) Orthodontic extrusion of a traumatically intruded permanent incisor: a case report with a 5-year follow-up. Dent Traumatol 24(6): 691-694.
- Belevcikli M, Altan H, Altan A (2020) Surgical Extrusion of Anterior Teeth with Intrusion Traumatic Injury: A Report on two Cases. Eur Endod J 5(3): 295-299.
- Saito CT, Luvizuto ER, dos Santos CL, Trevisan CL, Anzarini SR, et al. (2011) Treatment of traumatic dental intrusion by surgical repositioning. Compend Contin Educ Dent 32(6): 101-103.
- Silva JS, Herkrath A, Pontes DG, Queiroz AC, Medina PO et al. (2022) Multidisciplinary Management of Intrusive Luxation: Four-year Clinical Follow-up. Oper Dent 47(6): 603-611.
Editorial Manager:
Email:
pediatricdentistry@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...