Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6636
Research Article(ISSN: 2637-6636) 
Prevalence of Pediatric Cranio-Facial injury in West Libya and India- A Retrospective Study Volume 6 - Issue 3
Mohamed Elarbi*
Consultant Oral and Maxillofacial Surgeon, AOA Neurosurgery University, Libya
Received:July 19, 2021 Published: July 30, 2021
*Corresponding author: Mohamed Elarbi, Consultant Oral and Maxillofacial Surgeon, AOA Neurosurgery University, Libya
DOI: 10.32474/IPDOAJ.2021.06.000239
Abstract
Aim and Objective: To determine the prevalence of paediatric craniofacial fractures in Libya and India
Material and Methods: Traumatized patients reported to the emergency or casualty department of hospitals in respected demographic areas of country. In between 2017 and 2019 were selected for this study. The hospital records of patients were retrospectively analysed for age, gender, etiology of trauma, distribution of bone fracture in facial structure and among maxilla and mandible with the treatment procedures patients underwent in different age groups.
Result: 317 and 371 traumatic patients were analysed for paediatric craniofacial trauma in Libya and India hospitals respectively. The commonly affected age group were found to be 13-16years, with RTA being the most common etiology leading to mandible fracture with dentoalveolar and Lefors II fracture in majority of cases. The frequent treatment option found to be either conservative management or ORIF according to age groups.
Conclusion: The facial injury pattern is influenced by growth and age of patient. A retrospective study on the prevalence is important to know about the common cause of trauma as well as most prone bony structure to be fractured in associate age group. Such studies and data boost the campaigning on prevention and increasing awareness of facial fractures as well.
Introduction
In the past few decade, the facial injuries in children witnessed an exponential growth due to variable reasons. Here we present the incidence of facial injury in different demographic areas of world like Libya & India. Facial trauma in children brings up a challenge for treatment as well as aesthetic rehabilitation. It has a devastating effect on patient and to their families as well. Children are commonly affected by facial injuries due to higher cranial mass to body ratio which is 8:1 [1-3]. The less mineralized bone, flexible bone suture lines, lack of pneumatization of paranasal sinuses, presence of unerupted teeth leads to green stick fracture in children who encounter the trauma. Moreover, the prominence of buccal fat pad which disperse the momentum of force to wider regions, hence in children it demands higher force to fracture the bones when compared to adults. In patients with age less than 5 years facial structure is positioned returned than cranium shows less incidence of mid face fractures, as the age increases the downward and forward growth of face make maxilla a more prone structure to be fractured i.e., mid-facial injury [4,5]. The cause of facial fractures with regards to difference in demographic area may be due to the difference in culture and risk factors of specific age groups. The management of craniofacial injury requires a multi professional approach with prolong hospitalization and remarkable health care system [6]. Hence the undertaken of such epidemiological studies provide information and allows the development and implementation of polices to prevent traumatic injuries and to deliver an appropriate, prompt and commendable care to patients [7,8]. Here, in this study we have determined the prevalence of paediatric craniofacial injuries under different parameters as well as the treatment procedure done to the patients in different age groups.
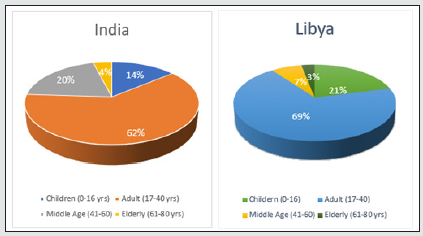
Materials and Method: the paediatric patients reported to the out-patient department of oral and maxillofacial surgery department in hospitals during the period of year 2017-2019 were included in this study. The design of study was approved by the institutional ethical committee and the details of all parameters were recorded and analysed under 3 different age groups of 0-5yrs, 6-12yrs, 13-16yrs (Graph-1).
Observation
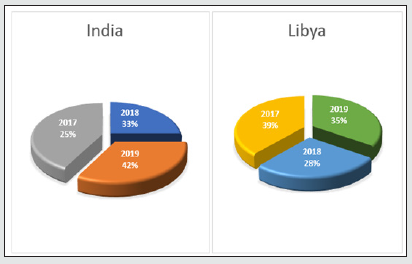
The purpose of this study was to record and make a report of the natural history of facial injuries in which total case reported were 317 in West Libya and 371 in Jaipur (India) from year 2017-2019 of paediatric craniofacial trauma at the emergency department of respected hospitals (Graph 2).
Results
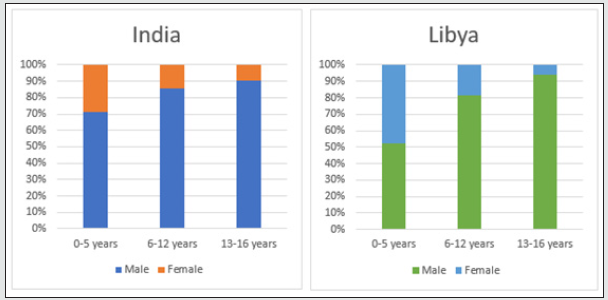
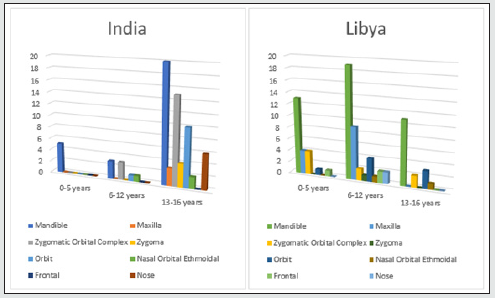
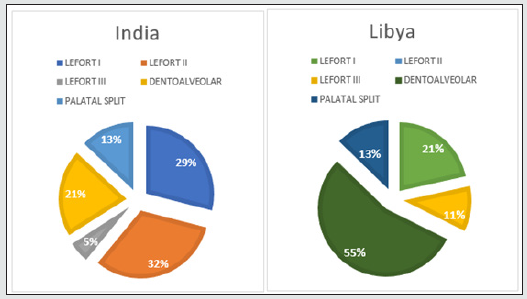
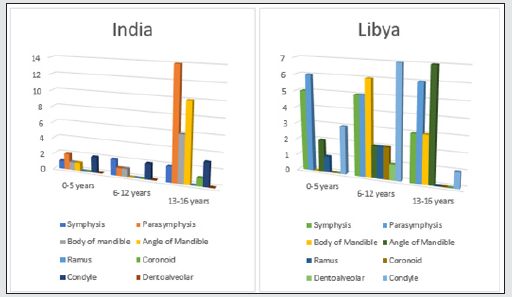
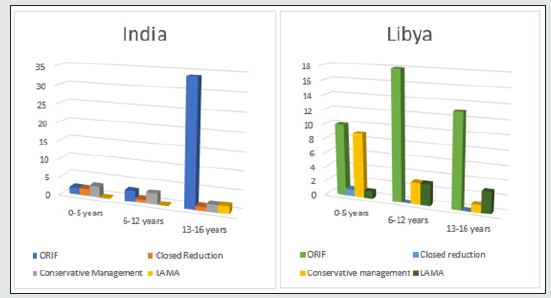
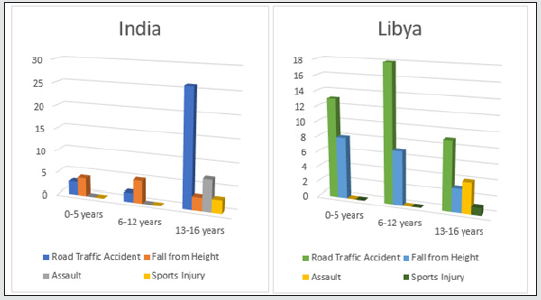
In our retrospective study of 317 (Libya) and 371 (India) cases of Craniofacial fractures, 21% (Libya) and 14% (India) of cases were of child trauma (Graph-1). There was a significant male predominance observed in all age group (Graph 3). The most common cause of the injury is RTA (nonviolent traumatic injury) in 62% (Libya) & 58% (India) in all age groups (Graph 4) followed by injury due to fall from height i.e 28%(Libya) 23% (India) till age group 0-12 years whereas, injury due to Assault is commonest after RTA in age group 13-16years which is 6% & 7% in Libya and India respectively. Sports injury is of 2% (Libya) & 3% (India) in age group 13-16years. Most of the cases involve more than one bone fracture including mandible, maxilla, zygomatic orbital complex, zygoma, orbit, nasal orbital ethmoidal, frontal and nasal (Graph 5) and the most commonly fractured bone is mandible among all which is about 54% and 46% in Libya and India respectively. Out of these, maximum cases were between age group 6-12years followed by 0-5years in Libya whereas its maximum in between by 13-16years followed by 6-12years in India. There is a male predilection in both the country data with 75% and 25% in male and females respectively and in India its 91% and 9% in male and females respectively (Graph 3). In maxillary bone fracture most, common fracture is of dentoalveolar (55%) and Lefort I (21%) in Libya however in India Lefort II is most common one (32%) followed by Lefort I (29%) and dentoalveolar (21%) (Graph 6). The mandible bone fracture is the commonest among all other bones fracture we found in our study and out of the entire mandible bone the most common fractured one is parasymphysis (27%) and symphysis (19%) in Libya. However, in India its Parasymphysis (29%) and Condyle (20%) of all the other bones. In Libya the predilection of fracture bone changes according to age, which is been parasymphysis (9%) and symphysis (7%) in 0-5years of age, Condyle fracture (7%) in 6-12years of age and angle fracture in 13-16years if age group (Graph 7). The common treatment procedures patients underwent were of Open reduction & internal fixation (ORIF) 63% followed by Conservative management (20%) in all the age groups in Libya. Whereas, in India most common treatment option is of conservative management (43%) in 0-5years of age group, conservative management and ORIF in 6-12years of age group (43% of both) and ORIF (87%) in between 13-16years of age group (Graph 8).
Graph 4: Etiological distribution of Maxillofacial Trauma in Paediatric patients according to age group.
Discussion
After the adults the young children are found to be at high risk for traumatic injuries. Children are also dependent of their caretakers and lacks coping skills [9]. They are under rapid developing and growth stage, if encounter a facial trauma brings surgeons in a perplexing situation to decide treatment procedure and modality taking in consideration of their age and growth phase [10,11]. Apart from the treatment factor child trauma demands a psychological management as well [9]. We underwent this study and recorded the prevalence of child trauma to improve the preventive measures and awareness regarding patient’s care from all aspects. The recorded data might help in a way to counsellors who all work with these population and age groups endeavour to reduce risk factors and improve protective factors eventually in the long run may reduce children’s exposure to traumatic accidents. Likewise, we hope legislators might influence some public policies related to child safety and care who have been exposed to traumatic injury as well as enhancement to childhood mental health by enhancing parents’ participation in psychoeducation focused events for reducing childhood trauma exposure and improving their ability to cope up with its post treatment phase medically as well as psychologically. The early childhood trauma has an impact on behavioural and learning skills of child The school counsellors serve as a mediators between wellness and academics will explore a way of awareness and implement the ruling regarding safety of child trauma in early childhood [12,13]. That’s how the longterm collection and analysis of epidemiologic data of paediatric facial injury by this retrospective study will help in improving the awareness and implementation of safety measure regarding child safety and health care [14,15].
Conclusion
By the present study we have conclude that the effect and the management of trauma depend on the age of child. Road traffic accident being the most common cause of trauma and mandible bone frequently fractured bone with dentoalveolar fracture during facial injuries. A clear male predilection has also been observed.
References
- Singaram MGSV, Udhayakumar RK (2016) Prevalence, pattern, etiology, and management of maxillofacial trauma in a developing country: a retrospective study. Journal of the Korean Association of Oral and Maxillofacial Surgeons 42(4): 174.
- Sharma P, Arora P, Valiathan A (2014) Age Changes of Jaws and Soft Tissue Profile. The Scientific World Journal p. 1–7.
- Brasileiro BF, Passeri LA (2006) Epidemiological analysis of maxillofacial fractures in Brazil: A 5-year prospective study. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 102(1): 28–34.
- Haug RH, Foss J (2000) Maxillofacial injuries in the pediatric patient. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 90(2): 126–134.
- Hatef DA, Cole PD, Hollier LH (2009) Contemporary management of pediatric facial trauma. Current Opinion in Otolaryngology & Head and Neck Surgery 17(4): 308–314.
- Wong L, Dufresne CR, Richtsmeier JT, Manson PN (1991) The Effect of Rigid Fixation on Growth of the Neurocranium. Plastic and Reconstructive Surgery 88(3): 395–403.
- Vanderas AP, Papagiannoulis L (1999) Incidence of dentofacial injuries in children: a 2-year longitudinal study. Dental Traumatology 15(5): 235–238.
- Gassner R, Tuli T, Hächl O, Rudisch A, Ulmer H (2003) Cranio-maxillofacial trauma: a 10-year review of 9543 cases with 21067 injuries. Journal of Cranio-Maxillofacial Surgery 31(1): 51–61.
- McLaughlin KA, Lambert HK (2017) Child trauma exposure and psychopathology: mechanisms of risk and resilience. Current Opinion in Psychology 14: 29–34.
- Kurpad SN, Goldstein JA, Cohen AR (2000) Bioresorbable Fixation for Congenital Pediatric Craniofacial Surgery: A 2-Year Follow-Up. Pediatric Neurosurgery 33(6): 306–310.
- Saunders BE, Adams ZW (2014) Epidemiology of Traumatic Experiences in Childhood. Child and Adolescent Psychiatric Clinics of North America 23(2): 167–184.
- Dufresne C, Manson P (2011) Pediatric Craniofacial Trauma: Challenging Pediatric Cases-Craniofacial Trauma. Craniomaxillofacial Trauma and Reconstruction 4(02): 73–84.
- Akama MK, Chindia ML, Macigo FG, Guthua SW (2008) Pattern of maxillofacial and associated injuries in road traffic accidents. East African Medical Journal 84(6): 287-295.
- Ashrafullah Pandey RK, Mishra A (2018) The incidence of facial injuries in children in Indian population: A retrospective study. Journal of Oral Biology and Craniofacial Research 8(2): 82–85.
- Zaggut AW, Rahman MM, Youssef G, Holmes S, Ellamushi H, et al. (2020) Craniomaxillofacial War Injuries in Misrata, Libya. Journal of Dentistry Open Access 2(2): 3-3.
Editorial Manager:
Email:
pediatricdentistry@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...