
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6636
Research Article(ISSN: 2637-6636) 
Pinch of Prevention in Pounds of Troubles: Utilization of Preventive Oral Health Care Services by High-Risk Children and Other Target Groups Amidst Covid- 19 Milieu Volume 7 - Issue 2
Irosha Perera1*, Chandra Herath2, Manosha Perera3 and Chandana Gajanayake4
1Preventive Oral Health Unit, National Dental Hospital (Teaching) Sri Lanka, Sri Lanka
2Division of Pedodontics, Department of Community Dental Health, Faculty of Dental Sciences, University of Peradeniya, Sri Lanka
3Alumnus School of Dentistry and Oral Health, Griffith University, Australia
4Deputy Director, Office of Deputy Director, National Hospital Sri Lanka
Received: January 10, 2022; Published: January 18, 2022
*Corresponding author: Irosha Perera, Preventive Oral Health Unit, National Dental Hospital (Teaching) Sri Lanka, Ward Place, Colombo 7, Sri Lanka
DOI: 10.32474/IPDOAJ.2022.07.000256
Abstract
Introduction: COVID-19 global pandemic caused suspension of routine and preventive dental treatment whilst prioritizing
emergency care. Preventive oral health care services contribute to oral health improvements among high-risk children and pregnant
women. We, therefore, aim to investigate the impact of COVID-19 on utilization of preventive oral health care services targeted for
high-risk groups provided by a premier tertiary care public dental hospital in Sri Lanka.
Methods: A retrospective cross-sectional study on performance statistics of the Preventive Oral Health Unit of National Dental
Hospital (Teaching) Sri Lanka was conducted for the periods from 1st January to 30th November 2020, pertaining to pre-COVID- 19
period (baseline), 1st Wave of COVID-19, transition period and on-going second wave. Comparisons were done on mean numbers of
selected preventive treatment episodes performed and risk groups attended using independent sample t-test, one-way ANOVA and
Kruskal-Walli’s test. Relative contributions of emergency visits for total visits were assessed for the given period. Data were entered
and analysed by using SPSS-21 statistical package.
Results: Significant declines was evident in preventive dental care episodes provided for high-risk toddlers and pregnant
mothers during the first and on-going second waves of COVID-19 compared to pre-COVID- 19 and transition periods(p<0.05). In
contrast, substantial increases detected in relative contribution of emergency visits for total number of visits among children for
symptomatic dento-alveloar infections during two waves of COVID-19 compared to pre-COVID- 19 and transition periods.
Conclusions: COVID-19 has negatively impacted on preventive oral health care service utilization by high-risk groups, whilst
raising the proportion of emergency visits due to aggravated dental diseases. Providing preventive care becomes essential to reduce
the burden of aggravated late sequel of dental caries among high risk children. Novel models of preventive oral health care services
for high-risk low socio-economic groups could be a way-forward in COVID-19 milieu.
Keywords: Preventive Oral Health Care; high risk groups; low socio-economic groups; COVID-19; emergency visits; Sri Lanka
Introduction
Corona virus disease (COVID-19) global pandemic caused by
SARS-Cov-2 virus presaged an indelible public health catastrophe
impacting individuals, families, countries, economies, and health
systems across the globe [1]. The global epicenters of highest spread
and burden of COVID-19 comprised the USA, Italy and Brazil at the
beginning presently concentrated to Indian sub-continent and neighboring countries in South Asia. The pandemic revolutionized
the landscape of health services from primary to tertiary care,
firstly to become scrambled to ensure safety of service providers
while being connected to service recipients [2], but lately to develop
innovation and resilience underpinned by timely transformations
[3,4]. Oral health services were strained by the high-risk status
of COVID-19 transmission attributed to face-to-face contact and
constant exposure to blood and saliva of patients compounded
by aerosol generation procedures inherent to dental treatment
procedures [5,6]. Consequently, COVID-19 induced dental practice
modifications became the new normal underpinned by meticulous
adherence to infection control informed by explicit evidence-based
technical guidance [7-10]. Accordingly, routine and non-urgent
dental treatment procedures were deferred, and treatment care
services were streamlined for emergency services strengthened
by patient triaging and risk stratification [11]. However, access to
basic oral health care services is considered to be a human right
[12] as it allows people to perform daily vital activities as eating,
speaking, smiling, sleeping and socially interacting without pain,
suffering and discomfort.
Despite availability of cost-effective preventive strategies,
untreated dental caries in permanent teeth recorded the most
prevalent condition according to global burden of oral diseases
affecting 2.4 billion people, and untreated caries in deciduous
teeth was the 10th -most prevalent condition, affecting 621
million children across the globe [13]. Indeed, dental caries among
children below 6-years of age known as early ‘childhood dental
caries’ has become the most common chronic childhood disease
[14]. Moreover, untreated dental caries accounts for the largest
unmet health need among preschool children compounded by late
squeal of pain, swelling and infection thus increasing the incidence
of emergency dental visits [15]. Pregnant women are at high risk of
dental caries and periodontal diseases compounded by oral health
effects of pregnancy associated life-style-changes and hormonal
changes [16]. Therefore, pregnant women, toddlers and preschool
children are among high risk groups for poor oral health. Targeting
preventive oral health care services for those high risk groups
become fundamental in reducing their oral disease burden [17].
Nevertheless, COVID-19 induced oral health service modifications
have resulted in serious impediments and limitations in providing
preventive oral health care services [18]. The first case of COVID-19
community transmission in Sri Lanka was reported on 11 March
2020. One of the unique features of Sri Lanka’s response to the
first wave of COVID-19 pandemic was its stringent enforcement of
community lockdown: closure of schools, public and private offices;
introducing work from home strategies; social/physical distancing;
closure of supermarkets, retail shops; and imposing a countrywide
quarantine curfew [19]. This resulted in curtailing indigenous
community transmission of the infection and limiting the death toll
to 13 as for 24 September 2020, attributed to COVID-19 [20].
However, a sinister second wave of COVID-19 emerged since
3rd October 2020 originated from the workforce of supply chain of
the country has expanded to 28,580 cases and 142 deaths as per 8th
December 2020. Despite possessing an efficiently pro-poor, unique
public health care delivery model extended up to the grass root level
that played a pioneering role in successful control of first wave of
COVID-19 [21], the country was grappling with many challenges in
flattening the persistently high epidemic curve of the second wave
[22]. In contrast to stringently imposed island wide lock down in
the first wave, the second wave has witnessed locally imposed lock
downs with travel restrictions yet continuation of near normalcy in
the country with health safety measures. Oral health care services
are closely integrated into the public health care delivery model in
the country and routine oral health care has been suspended during
the first wave [23,24] and ongoing second wave of the COVID-19
infection in the country. However, the National Dental Hospital
(Teaching) Sri Lanka, the premier multi-specialty public dental
hospital continued to provide emergency and essential services
[23]. Preventive Oral Health Unit of this hospital exclusively caters
to socially disadvantaged, culturally diverse high risk groups in
the Colombo Municipal Council region [25-28] which became
the epicenter in COVID-19 community clusters and infection
transmission in Sri Lanka. Therefore, navigating preventive
oral health care services to target groups deemed increasingly
challenging in that present context. Against this backdrop, we aim
to investigate the impact of COVID-19 on utilization preventive
oral health care services of Sri Lanka’s National Dental Hospital
with potential implications on the need for such services targeted
for high risk groups and communities during global pandemic by
mitigating many constraints and challenges.
Methods
A retrospective cross-sectional study was conducted to assess the performance statistics on preventive oral health care services delivered to high risk urban priority groups for the periods pertaining to pre-COVID 19, 1st Wave of COVID -19, transition period and ongoing second wave of COVID-19 in Sri Lanka.
Study setting
Preventive Oral Health Unit (POHU) of National Dental Hospital (Teaching) Sri Lanka was the study setting. This unit provides preventive oral health care services for high risk targets groups of toddlers, preschool children, primary school children, pregnant women and diabetic patients underpinned by a geographically targeted need and demand based model of Colombo Municipal Council (CMC) region. As revealed by previous findings, they belonged to low socioeconomic status and multi-racial backgrounds [25].
Data sources
Performance statistics data of the preventive dental clinic conducted by POHU for the year 2020 from 1st January to 30th November was accessed from the data base. Data on total number of visits and total number of episodes of given categories of preventive oral health treatment offered per given month were collected. Collected data on selected treatment procedures comprised of total number of oral hygiene instructions and dietary counselling for parental care givers of children, pregnant women and diabetic patients, Glass Ionomer Cement (GIC) fillings, fluoride varnish applications, fluoride gel applications, scaling and emergency management of dento-alveolar infections (prescribing antibiotics and analgesics). Moreover, total numbers of each category of target groups: toddlers (children ≤ 3-years), Pregnant women and patients with diabetes accessed preventive oral health care services in each month were obtained.
Statistical analysis
Comparisons were made on mean selected indicators of
treatment categories and dental patients over 4-time periods
namely:
a) Pre-COVID 19 period (January & February 2020),
b) 1st Wave of COVID-19 (March to May 2020),
c) Transition period (June to September 2020) and
d) On-going 2nd Wave of COVID-19.
Selected dental treatment episodes were preventive care
comprised of oral hygiene advice with dietary counselling, fluoride
varnish and gel applications, fissure sealant applications, GIC
fillings and scaling. Percentage contributions of emergency visits
to total visits were compared from January to November 2020.
Distributions of variables were assessed for normality by using
Kolomogorov-Smirnov and Shapiro-Wilk tests. Independent
sample t-test, one-way ANOVA and Kruskal-Wallis tests were used
to compare means at the statistical significance of p <0.05. Data
were entered and analysed by using SPSS-21 statistical package.
Results
During the pre-COVID 19 period (baseline), a total of 2807
visits which included both first visits and recall visits were made
by high risk groups of toddlers, preschool children, primary school
children, pregnant women and patients with diabetes to the POHU.
Whilst there were 912 total visits during first wave of COVID-19
which overlapped a stringently imposed island wide lock down
from mid-March to May 2020. There was a total of 3846 visits
for the ‘transition’ period extended from June to September that
recorded exit from stringent lockdown with“0” community cases of
COVID-19 in Sri Lanka that continued over a period of 4-months,
however, ended up by emergence of a second wave of COVID-19
since October 2020 which is on-going. This resulted in a spectacular
decline in total visits limiting to 60 until end of November.
Table 1 illustrates the comparison of mean numbers of selected
preventive dental treatment episodes: oral hygiene advice and
dietary counseling, fluoride varnish application, fluoride gel
application, fissure sealant applications provided by POHU from
January to November 2020 that overlapped 4-trajectories of
COVID-19 in Sri Lanka from pre-COVID- 19 to on-going second
wave. As demonstrated in Table 1, clearly discernible reductions
were evident in preventive dental treatment episodes comprised
of fluoride applications, fissure sealant applications and GIC
fillings during two COVID -19 waves compared with pre-COVID
19 (baseline) and transition periods. Those differences were
statistically significant (p <0.05). However, there were no significant
differences in mean episodes of oral hygiene advice and dietary
counseling as well as scaling treatment despite overall reductions
in treatment episodes during two waves of COVID-19. Moreover,
significant reductions in total number of visits in two COVID-19
waves were evident compared with transition and baseline periods
(p<0.05).
Table 1: Comparison of mean episodes of preventive dental treatment and emergency treatment.
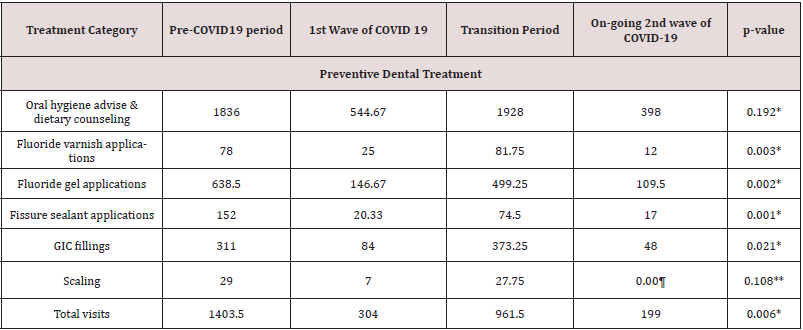
*One-way ANOVA test **Kruskal-Walli’s test ¶ no scaling done
Table 2: Comparison of mean numbers of high risk groups treated at POHU.
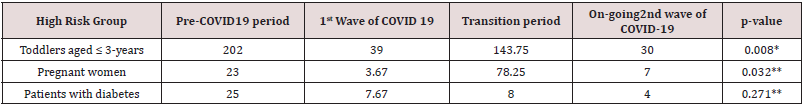
*One-way ANOVA **Kruskal-Wallis Test
Figure 1: Relative contribution of emergency visits to total visits (January to November 2020).
* 99% of emergency visits were made by children.

Figure 1 depicts the % contribution of emergency visits to total visits made to POHU from January to November 2020. It shows a significant peak in October 2020, accounted for 76% of total visits superimposed on second wave of COVID-19. Similar peak was evident in April 2020, accounted for 70% of total visits, which overlapped the first wave of COVID-19. During the transition period there were notable reductions in % proportion of emergency visits. As illustrated in Table 2, remarkable reductions in attendance of toddlers during waves of COVID-19 compared with pre-COVID-19 (baseline) and transition period was observed that were statistically significant (p<0.05). Similarly, there were significant reductions in pregnant women who received preventive oral health care during COVID-19 waves compared to baseline and transition period that marked an increased attendance over baseline. A notable reduction of patients with diabetes accessing preventive oral health care was evident in the first wave of COVID-19 compared to baseline level which had continued through to transition period and on-going second wave. However, those differences were not statistically significant over four time periods (p>0.05).
Discussion
COVID-19 pandemic continues to affect health status of people
by heavily impacting on health systems and health workers
across the globe. Hence, countries need critical consideration on
alternative models of health care provision for prioritized health
needs of people [23]. As deferment of routine dental treatment with
exclusive emergency/urgent dental care was the norm of COVID-19
induced dental practice modifications [29], studies have reported
increase in emergency dental visits to tertiary care hospitals in
many countries [30]. Furthermore, delaying dental visits especially
for checkups, planned treatment as well for bothering issues among
adults attributed to COVID-19 has been reported [31]. Moreover,
an array of studies highlighted the impact of COVID-19 pandemic
on oral health care services ranging from oral & maxillofacial
practices, dento-alveolar/oral & maxillofacial injuries [32,33], oral
oncological services [34] and Paediatric dental services [35,36].
Despite, the common notion on notable restrictions, it is not known
how COVID-19 specifically impacted on preventive oral health
care services. Therefore, present study addressed this information
gap pertaining to preventive oral health care services of a tertiary
care public dental hospital in Sri Lanka, a lower-middle-income
developing country. As emerged from the findings, there were
significant reductions in preventive dental treatment episodes
delivered to high risk toddlers and pregnant women. Moreover,
there were substantial reductions in attendance of children and
patients with diabetes for routine preventive oral health care.
Deferment of routine and non-urgent dental treatment such as
fluoride and fissure sealant applications and GIC fillings seemingly
impacted on increased incidence of emergency visits among
children, accounted for almost three fourths of total visits in two COVID-19 waves. Despite offering oral hygiene and dietary advice
for high risk children and their parental caregivers at emergency
visits with symptomatic dento-alveolar infections, it is not clear
how well they complied with those advice. The Colombo Municipal
Council region, the terrain of current geographically targeted
preventive oral health care model for high risk groups became
the epi-centre of second wave of on-going COVID-19 in Sri Lanka.
Therefore, lock-down scenario of locals of this region compounded
by oral health service restrictions resulted in discernible reductions
in attendance of toddlers, pregnant women and diabetic patients
during COVID-19 waves.
The unprecedented challenges encountered by Paediatric
dentists at present providing services for children have been
well documented. The uncertainty of COVID-19 infectious status
of children who are predominantly asymptomatic has created
a dilemma [37]. Moreover, gaining cooperation of toddlers
and children having dental anxiety becomes difficult as they
could cough and cry generating more aerosols thereby possibly
increasing the risk of COVID-19 transmission [38]. However, noninvasive,
preventive dental treatment procedures such as fluoride
applications garnered better cooperation from high risk children
combined with non-pharmacological behavioural management
techniques [28]. Given the high burden of advanced dental caries
among high risk children, that give rise to frequent painful dentoalveolar
infections, compounded by absence of aerosol generating
pulp therapy and near absence of extraction of non-restorable
pulp-exposed deciduous teeth under general anaesthesia, minimal
intervention dentistry (MID) provides a viable option [38].
Clinical preventive dental treatment is underpinned by MID which
involves no, or selective carious tissue removal accomplished by
hand instruments [39] complimented by brushing and dietary
advice, fluoride and fissure sealant applications. Therefore,
current recommendations highlight the importance of practicing
minimally invasive dental caries management techniques for high
risk children as COVID-19 continues to impact paediatric dentistry
practice [38,40].
High contribution of emergency visits of children having
symptomatic pulp exposed teeth to total number of visits
was clearly evident in our findings pertaining to two waves of
COVID-19. Furthermore, prescribing antibiotics and analgesic for
children presented for the emergency of dento-alveolar infections
were complimented by brushing and dietary advice and fluoride
applications. Those complied with the international guidelines
on paediatric dentistry that emphasized triaging and exclusive
treatment for emergency cases by minimizing aerosol generation
procedures underpinned by case-base selection of biological, noninvasive
or minimally invasive treatment methods [40]. However,
increased incidence of symptomatic dento-alveolar infections of
high risk children warrants further investigations. Breakdown
of preventive oral health care with regular follow-up visits could
have substantially impacted on their oral health status. This
could have been mediated by cariogenic dietary patterns and
less optimal brushing habits. A recent study conducted in Brazil
reported those changes in dietary habits of children as perceived
by parents and their fears in accessing dental care for the children
except for urgent visits [41]. Therefore, such factors could have
contributed for patterns of utilization of preventive oral health
services observed in this study during COVID-19 waves. Moreover,
our findings demonstrated significant reductions in attendance for
preventive oral health care by pregnant women during COVID-19
waves whilst showcasing a relatively high attendance during
transition period that lasted between two subsequent COVID-19
waves. As the pregnant women were predominantly referred from
geographically targeted ante-natal clinic based oral health programs
conducted in Colombo Municipal Council region [26], termination
of those during COVID-19 waves could have plausibly contributed
to significant reductions in their attendance. Further, termination
of aerosol generating ultrasonic scaling treatment during COVID-
19 waves as shown in our results, could have contributed to
reductions in the attendance of pregnant women and vice-versa
as this treatment was mostly provided to them. This speculation
could have been valid for patients with diabetes as well, since most
of them received scaling treatment to improve their oral hygiene
and periodontal disease status. However, provision of routine
scaling is fraught with criticism pertaining to lack of evidence-base
and cost of resources [42]. Furthermore, diabetes has garnered
recognition for poor outcomes in COVID-19 especially among older
adults [43,44] who opted to refrain utilizing routine health care
services. That could have contributed to persistent low attendance
of patients with diabetes (predominantly comprised of older adults
and elderly) since the first wave of COVID-19 as evident from our
findings. Nevertheless, it is not known how inability in accessing
preventive oral health care services both by pregnant women and
patients with diabetes impacted on their oral health status. This
becomes important to investigate in the light of evidence on the
possible connection of poor oral hygiene with severity of SARSCoV-
2 infection especially among older adults and elderly having
non-communicable diseases such as diabetes [45].
The COVID-19 pandemic the unprecedented global public
health conundrum, demonstrated high-virulence transmission
compounded by heterogeneity in patterns of vulnerability [46].
Therefore, it became important to understand the country-wise
dynamics of COVID-19 vulnerability. Undoubtedly, the COVID-19
pandemic has challenged health professions and systems, having
evoked success and failures in flattening the epidemic curves while
ensuring continuous access to health care by needy people across
the globe. Moreover, it posed a significant challenge for dentistry
as there is an elevated risk of cross infection among patients and
dental practitioners [6]. In this backdrop, the roles of preventive
oral health care professionals in preventing the transmission of
COVID-19 while engaging in pro-active and reformed dentistry
[47,48] catering to children and other vulnerable groups have
become a cause for concern. As populations disproportionately
affected by COVID-19 carried a higher risk for oral diseases whilst
becoming susceptible for oral health disparities [49] compounded
by deepening child oral health inequities [50], ensuring access to
preventive oral health care services has become an ethical and moral imperative. In light of evidence of current recommendations
on employing dynamic suppression interventions for pragmatic
control COVID-19 transmission [50], encouraging high risk groups
to access preventive oral health care during relaxation periods
become important.
Conclusions
Our findings provided some deep insights into how COVID-19 milieu heavily impacted on a preventive oral health care service delivery model of a tertiary care public dental hospital. It was well-known that accessing preventive oral health care services reached an almost standstill across the globe concomitant to COVID-19. However, little was known about accessing preventive oral health care services by high risk low-socioeconomic groups in a developing country context. As evident from the findings, the impact of COVID-19 milieu was not only pervasive but multifaceted pertaining to utilization of preventive oral health services and preventive dental treatment episodes. Increased incidence of emergency visits in waves of COVID-19 that superimposed on severe constraints in delivery of comprehensive preventive oral health care package indirectly indicated its effectiveness in preventing and controlling emergency dental visits of high risk children having multiple dental caries. This notion was further supported by flattening of proportion of emergency visits to total visits almost to the baseline level during transition period in which the delivery of the comprehensive preventive oral package was resumed. Providing preventive oral health care while addressing the symptomatic dento-alveolar infections became useful in reducing the burden of aggravated late sequel of dental caries among high risk children. Moreover, innovative models of preventive oral health care services for high risk low socio-economic groups dominated by children could be a way-forward in COVID-19 milieu and in similar pandemics in future..
Funding
This research received no external funding.
Acknowledgments
Authors wish to acknowledge the contribution of health staff of Preventive Oral Health Unit of National Dental Hospital (Teaching) Sri Lanka.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Arshad Ali S, Baloch M, Ahmed N, Arshad Ali A, Iqbal A (2020) The outbreak of Coronavirus Disease 2019 (COVID-19)-An emerging global health threat. J Infect Public Health 13(4): 644-646.
- Krist AH, DeVoe JE, Cheng A, Ehrlich T, Jones SM (2020) Redesigning Primary Care to Address the COVID-19 Pandemic in the Midst of the Pandemic. Ann Fam Med 18(4): 349-354.
- Wong ELY, Yeoh EK, Dong D (2020) Covid-19: Transforming healthcare will require collaboration and innovative policies. BMJ 369: 2229.
- Legido Quigley H, Asgari N, Teo YY, Leung GM, Oshitani H, et al. (2020) Are high-performing health systems resilient against the COVID-19 epidemic? Lancet 395(10227): 848-850.
- Richards W (2020) Being a dentist in the pandemic. Evid Based Dent 21(2): 58-59.
- Bescos R, Casas-Agustench P, Belfield L, Brookes Z, Gabaldón T (2020) Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine. J Dent Res 99(9): 1113.
- (2020) World Health Organization. Considerations for the provision of essential oral health services in the context of COVID-19. Interim guidance.
- (2020) Centers for Disease Control and Prevention. Interim Infection Prevention and Control Guidance for Dental Settings During the COVID-19 Response.
- (2020) American Dental Association. What Constitutes a Dental Emergency?.
- European Centre for Disease Control and Prevention Stockholm 2020.Personal protective equipment (PPE) need in health care setting for the patents with suspected or confirmed novel corona virus (2019nCov), ECDC Technical Report.
- Gurzawska Comis K, Becker K, Brunello G, Gurzawska A, Schwarz F (2020) Recommendations for Dental Care during COVID-19 Pandemic. J Clin Med 9(6): 1833.
- Catalanotto FA (2006) A welcome to the workshop on professional promises: Hopes and gaps in access to oral health care. J Dent Educ 70(11): 1120-1124.
- Kassebaum NJ, Bernabé E, Dahiya M, Bhandari B, Murray CJ, et al. (2015) Global burden of untreated caries: a systematic review and metaregression. J Dent Res 94(5): 650-658.
- Folayan M, Olatubosun S (2018) Early Childhood Caries - A diagnostic enigma. Eur J Paediatr Dent 19(2): 88.
- Corrêa Faria P, Daher A, Freire MDCM, de Abreu MHNG, Bönecker M, et al. (2018) Impact of untreated dental caries severity on the quality of life of preschool children and their families: a cross-sectional study. Qual Life Res 27(12): 3191-3198.
- Karunachandra NN, Perera IR, Fernando G (2012) Oral health status during pregnancy: rural-urban comparisons of oral disease burden among antenatal women in Sri Lanka. Rural Remote Health 12: 1902.
- Wang NJ, Aspelund GØ (2010) Preventive care and recall intervals. Targeting of services in child dental care in Norway. Community Dent Health 27(1): 5-11.
- Brian Z, Weintraub JA (2020) Oral Health and COVID-19: Increasing the Need for Prevention and Access. Prev Chronic Dis 17: E82.
- Ratnasekera N, Perera I, Kandapolaarachchige P, Surendra G, Dantanarayana A (2020) Supportive care for oral cancer survivors in COVID-19 lockdown. Psychooncology 29(9): 1409-1411.
- Wickramaarachchi WPTM, Perera SSN, Jayasinghe S (2020) COVID-19 Epidemic in Sri Lanka: A Mathematical and Computational Modelling Approach to Control. Comput Math Methods Med 2020: 4045064.
- Adikari PS, Pathirathna K, Kumarawansa W, Koggalage PD (2020) Role of MOH as a grassroots public health manager in preparedness and response for COVID-19 pandemic in Sri Lanka. AIMS Public Health 7(3): 606-619.
- Attanayake AMCH, Perera SSN, Jayasinghe S (2020) Phenomenological Modelling of COVID-19 Epidemics in Sri Lanka, Italy, the United States, and Hebei Province of China. Comput Math Methods Med 2020: 6397063.
- Surendra G, Perera I, Ranasinghe A, Kumarapeli V, Tham R, et al. (2021) Pattern and Causes of Oral and Maxillofacial Injuries Presented to a Tertiary Care Public Dental Hospital in Strictly Imposed COVID-19 Lockdown Scenario. Oral 1: 3-14.
- Jayasuriya NSS, Perera IR, Ratnapreya S (2020) Re: Maxillofacial Surgery and COVID-19, the Pandemic!. J. Maxillofac. Oral Surg 19: 475–476.
- Perera I, Herath C, Perera M, Dolamulla S, Jayasundara Bandara JM (2017) Service Delivery of a Preventive Oral Health Care Model to High Caries Risk Urban Children in Sri Lanka: A Retrospective, Descriptive Study. Journal of Advances in Medicine and Medical Research 20(3): 1-10.
- Irosha Rukmali Perera, Manosha Lakmali Perera, Thilini Kulathunge (2019) Providing Oral Health Awareness and Screening to Low Income, Urban Pregnant Women: A Developing Country Perspective. Journal of Gynecology and Women’s Health 17(2): 555958.
- Perera IR, Wickramaratne PWN, Liyanage NLP, Karunachandra KNN, Bollagala AD, et al. (2013) Preventive dental clinic solutions to tackle early childhood dental caries. International Conference on Public Health Innovations. National Institute of Health Sciences Sri Lanka.
- Karunachandra KNN, Bollagala AD, Perera IR, Liyanage NLP, Kottahachchi MJ, et al. (2013) Behavioural management strategies and oral health related behaviours of preschool children receiving preventive dental care. International Conference on Public Health Innovations. National Institute of Health Sciences Sri Lanka.
- Dave M, Seoudi N, Coulthard P (2020) Urgent dental care for patients during the COVID-19 pandemic. Lancet 395(10232): 1257.
- Yang Y, Zhang W, Xie L, Li Z (2020) Characteristic changes of traumatic dental injuries in a teaching hospital of Wuhan under transmission control measures during the COVID-19 epidemic. Dent. Traumatol 36: 584–589.
- Kranz AM, Gahlon G, Dick AW, Stein BD (2020) Characteristics of US Adults Delaying Dental Care Due to the COVID-19 Pandemic. JDR Clin Trans Res 27: 2380084420962778.
- Maffia F, Fontanari M, Vellone V, Cascone P, Mercuri LG (2020) Impact of COVID-19 on maxillofacial surgery practice: a worldwide survey. Int J Oral Maxillofac Surg 49(6): 827-835.
- Jayasuriya NSS, Perera IR, Ratnapreya S (2020) Re: Maxillofacial Surgery and COVID-19, the Pandemic! J Maxillofac Oral Surg 19(3): 475-476.
- Wu V, Noel CW, Forner D, Zhang ZJ, Higgins KM, et al. (2020) Considerations for head and neck oncology practices during the coronavirus disease 2019 (COVID-19) pandemic: Wuhan and Toronto experience. Head Neck 42(6): 1202-1208.
- Jayaraman J, Dhar V, Moorani Z, Donly K, Tinanoff N, et al. (2020) Impact of COVID-19 on Pediatric Dental Practice in the United States. Pediatr Dent 42(3): 180-183.
- Casamassimo PS, Townsend JA, Litch CS (2020) Pediatric Dentistry During and After COVID-19. Pediatr Dent 42(2): 87-90.
- She J, Liu L, Liu W (2020) COVID-19 epidemic: Disease characteristics in children. J Med Virol 92(7): 747-754.
- Bani Hani A, Gardener C, Raggio DP, Santamaría RM, Albadri S (2020) Could COVID-19 change the way we manage caries in primary teeth? Current implications on Paediatric Dentistry. Int J Paediatr Dent 30(5): 523-525.
- Innes NP, Frencken JE, Bjørndal L (2016) Managing carious lesions: consensus recommendations on terminology. Adv Dent Res 28(2): 49‐57.
- Al-Halabi M, Salami A, Alnuaimi E, Kowash M, Hussein I (2020) Assessment of paediatric dental guidelines and caries management alternatives in the post COVID-19 period. A critical review and clinical recommendations. Eur Arch Paediatr Dent 21(5): 543-556.
- Campagnaro R, Collet GO, Andrade MP, Salles JPDSL, Calvo Fracasso ML, et al. (2020) COVID-19 pandemic and pediatric dentistry: Fear, eating habits and parent's oral health perceptions. Child Youth Serv Rev 118: 105469.
- Singh AK, Gupta R, Ghosh A, Misra A (2020) Diabetes in COVID-19: Prevalence, pathophysiology, prognosis and practical considerations. Diabetes Metab Syndr 14(4): 303-310.
- Shahid Z, Kalayanamitra R, McClafferty B, Kepko D, Ramgobin D, et al. (2020) COVID-19 and Older Adults: What We Know. J Am Geriatr Soc 68(5): 926-929.
- Watt RG (2020) COVID-19 is an opportunity for reform in dentistry. Lancet 396(10249): 462.
- Sampson V, Kamona N, Sampson A (2020) Could there be a link between oral hygiene and the severity of SARS-CoV-2 infections? Br Dent J 228(12): 971-975.
- Sominsky L, Walker DW, Spencer SJ (2020) One size does not fit all - Patterns of vulnerability and resilience in the COVID-19 pandemic and why heterogeneity of disease matters. Brain Behav Immun 87: 1-3.
- Halepas S, Ferneini EM (2020) A Pinch of Prevention is Worth a Pound of Cure: Proactive Dentistry in the Wake of COVID-19. J Oral Maxillofac Surg 78(6): 860-861.
- Kalash DA (2020) How COVID-19 deepens child oral health inequities. J Am Dent Assoc 151(9): 643-645.
- Chowdhury R, Heng K, Shawon MSR, Goh G, Okonofua D, et al. (2020) Global Dynamic Interventions Strategies for COVID-19 Collaborative Group. Dynamic interventions to control COVID-19 pandemic: a multivariate prediction modelling study comparing 16 worldwide countries. Eur J Epidemiol 35(5): 389-399.
- Jacobs A, Perera I, Kruger E, Tennant M (2011) A discussion of factors influencing the oral health of Australian Aboriginal and Torres Strait Islander population. International Journal of Oral Health 7: 1-6.
Editorial Manager:
Email:
pediatricdentistry@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




