Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6636
Research Article(ISSN: 2637-6636) 
Oral Streptococci and Other Oral Commensals in Children Volume 7 - Issue 2
Sayan Bhattacharyya*
Associate Professor, Department of Microbiology, AIIH&PH, India
Received: January 13, 2022; Published: January 26, 2022
*Corresponding author: Sayan Bhattacharyya, Associate Professor, Department of Microbiology, AIIH&PH, Kolkata, India
DOI: 10.32474/IPDOAJ.2022.07.000258
Abstract
Oral Streptococci are important commensal flora of children and also play a role in development of many diseases of the mouth cavity and extra-oral diseases. They belong to many genera and species. It is important to know about commensal oral bacteria and their interplay with other bacteria. In this article the author has tried to give brief information about these bacteria and their functions and ill effects while being present in the mouth.
Keywords: Oral microbiota; Streptococci; caries
Introduction
Leeuwenhoek’s microscopic observations in his own dental plaque, more than 3 centuries ago, had indicated an unexpected diversity of microorganisms ( “animalcules”) in the human oral cavity [1]. Oral streptococci are common commensals in children. Their presence in excess amounts causes plaque and caries. Numbers can increase after eating sweet food items. Bacteria in the genus Streptococcus are the first inhabitants of the oral cavity and can be acquired right after birth. They thus play a very important role in the assembly of the oral microbiome [2]. Hence it is important to study the oral Streptococci and their characteristics, particularly in children.
Materials and Methods
Thorough scientific literature search using scientific terms was
used to search for literature.
Types of oral streptococci in children: Streptococcus mitis,
Streptococcus salivarius, S. sanguis and others are common. They
belong commonly to the capsular Lancefield groups F, M and N.
Now the oral streptococci are classified into 8 distinct groups: mitis,
sanguinis, anginosus, salivarius, downei, mutans, pyogenic, and
bovis. Pyogenic and bovis groups are not commonly seen in mouth
[2]. The mitis group is the largest bacterial group found in the oral
cavity, presently having 20 species.
Other oral commensal bacteria in children: Leptospira and
Borellia can also be seen in oral cavity in children. Even anaerobes
like Fusobacterium spp. are common in oral cavity of children and
tend to colonize early [1]. In healthy children and adults, there is
a balance between the numbers of cariogenic bacteria and noncariogenic
commensals. The latter keeps the cariogenic population
in mouth in check by the formation of alkali, Hydrogen peroxide or
other inhibitory molecules [2]. Bacteria like Rothia spp., Treponema
spp. and Veillonella spp. are later colonizers of the mouth [1].
Development of the oral microbiome in children: It
has been postulated that oral bacteria of the mother get entry
into the blood and then via placenta can enter the oral cavity
of the developing fetus. However, this theory is debated and
needs further testing [1]. Also, a combination of different mother
microbiome sources like gut, vaginal, skin flora and other factors.
Additionally, breast milk and early foods may also shape the early
oral microbiome in children [1]. The metabolic products formed by
Streptococcus spp. using dietary oligosaccharides in breast milk or
formula as substrates by fermentation, pave the way for other oral
commensal bacteria to survive [1].
Role of the oral commensals in children: Commensal
bacteria in the oral cavity play some pathogenetic roles in disease
and ill health.
Caries: Oral Streptococci , also called Viridans Streptococci, are
directly implicated in Dental caries. It is well known that the oral
streptococci ferments carbohydrates to form demineralizing acids
that leads to plaque and caries [3]. Mutans Group of Streptococci
has 2 main cariogenic species: S. mutans and S. sobrinus [4] Good
oral hygiene and regular flossing has been shown to prevent caries of teeth in teenagers(3). An association of S. mutans with
other acidogenic bacterial species, like Scardovia wiggsiae and
bifidobacteria, has been documented in severe early childhood
caries [2].
Pathogenesis of caries: Under the conditions of too much
of carbohydrates and less oxygen, streptococci tend to carry
out homolactic fermentation, thus reducing pyruvate into lactic
acid and making NAD from NADH. The formation of lactic acid
leads to speedy acidification of the environment, which allows
streptococcal species to outclass acid-sensitive microorganisms
[2]. Bacterial adhesins adhere well to the substrates in the acquired
salivary pellicle , like albumin, proline-rich proteins, glycoproteins,
mucins, and sialic acid. This then promotes release of bacterial
polysaccharide and DNA. Salivary amylase also plays a pivotal
role in bacterial colonization of oral surfaces of man and other
mammals. This is because amylase-binding bacteria (like S. mitis, S.
gordonii, S. salivarius and S. cristatus) have been found to colonize
only the hosts having salivary amylase activity [5].
Role of Lactobacilli in caries: In around 3 month old children,
Lactobacilli are also common in oral microbiome. This genus is also
cariogenic, and their presence is highly predictive of caries at about
3 years of age [1].
Rheumatic fever and oral Streptococci: Rheumatic fever
can develop after pharyngitis caused by Group A Streptococci. Oral
streptococci share antigens with tissues in heart, glomerulus of
kidney and joints. Hence antibodies cross react, and this can explain
Rheumatic fever. Mainly Group A Streptococci are imp0ortant here.
Anti-myosin antibodies in blood have been found to react with the
M protein epitope of Group A Streptococci [6]. S. pyogenes (group A
β-hemolytic streptococcus) can be seen in the oropharynx of more
than 20% of children and a smaller portion of adults. Carriage rates
increase a lot during epidemics and in crowded conditions [7].
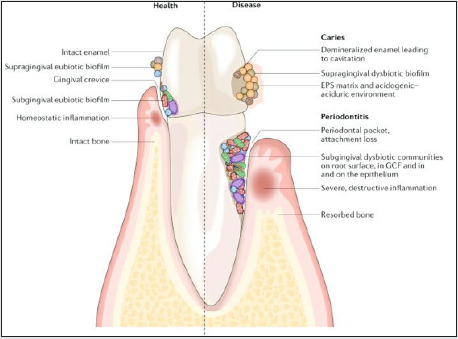
Periodontitis: Other than dental caries , periodontitis is also
directly related to the presence and metabolic activities of the
dental plaque bacteria [2].
Other diseases: Oral Streptococci, the first microorganisms to
colonize oral mucosal surface and the dominant bacteria in the
human oral cavity, have recently gained attention as the pathogens
of various systemic diseases, like infective endocarditis, purulent
infections, brain hemorrhage, intestinal inflammation, autoimmune
diseases, and also bacteremia [8].
Use as probiotics: Commercially available products containing
Streptococcus salivarius strains K12, M18 or 24smb have been
used for optimum oral and dental healthcare [9]. S. salivarius is a
component of the healthy microbiota of the oral and nasopharyngeal
cavity. S. salivarius K12 was first extracted from the oral cavity of
a healthy school-going child in New Zealand, and many strains
have been developed since to protect and maintain oral health
also. Salivaricins liberated from S. salivarius interact with the cell
walls of Gram-positive bacteria, producing a bactericidal effect. It is
capable to reduce load of otopathogens causing Acute otitis media
in nasopharynx of children [9].
Other interesting facts
Oral bacteria also help enhance mucosal immunity. Both cellular and numeral immunity may be enhanced by the oral microbiota. The oral bacteria and its importance are highlighted in Figure 1 below.
Detection
The oral Streptococci can be detected by appearance of colonies that are alpha hemolytic on sheep blood agar and form black heaped colonies commonly on Mitis- Salivarius agar. Mitis- salivarius agar has casein enzyme hydrolysate, Dextrose, sucrose and Trypan blue with other constituents. This medium (having 1% potassium tellurite) is a highly selective medium, that enables to isolate streptococci from highly contaminated specimens like exudates from body cavities and faeces, since it inhibits a wide variety of bacteria [10]. E. coli is inhibited in this medium, Enterococci produce blue-black colonies while S. salivarius produces blue or gum-drop colonies.
Discussion
Oral Streptococci are very common in mouth of children and should be investigated whenever serious lesions are seen. They have diverse pathogenetic factors. Their quantity or population is linked with plaque, caries, and periodontitis in children. Other bacteria are also important in the mouth. The oral microbiome is complex and is very interesting to study.
Conclusion
Oral Streptococci play diverse roles in the body and hence should be studies and researched meticulously.
References
- Gomez A, Nelson KE (2017) The Oral Microbiome of Children: Development, Disease and Implications Beyond Oral Health Microb Ecol 73(2): 492-503.
- Abranches J, Zeng L, Kajfasz JK (2018) Biology of Oral Streptococci. Microbiol Spectr 6(5).
- Seow WK, Cheng E, Wan V (2003) Effects of Oral Health Education and Tooth-brushing on Mutans Streptococci Infection in Young Children. Pediatric Dentistry 25(3): 223-228.
- Okada M, Soda Y, Hayash F, Doi T, Suzuki J, et al. (2002) PCR detection of Streptococcus mutans and S sobrinus in dental plaque samples from Japanese children. J Med Microbiol 68: 443-447.
- Scannapieco FA, Solomon L, Wadenya RO (1994) Emergence in human dental plaque and host distribution of amylase-binding streptococci. J Dent Res 73: 1627-1635.
- Cunningham MW (1996) Streptococci and Rheumatic Fever. Friedman H, Rose NR, Bendinelli M (Eds.), Microorganisms and Autoimmune Diseases. Infectious Agents Pathog. Springer, Boston, MA, USA 24(4): 408-416.
- V Courtney Broaddus MD (2022) Murray & Nadel's Textbook of Respiratory Medicine Streptococcus - an overview | Science Direct Topics.
- Yumoto H, Hirota K, Hirao K, Ninomiya M, Murakami K, et al. (2019) The Pathogenic Factors from Oral Streptococci for Systemic Diseases. Int J Mol Sci 20(18): 4571.
- Sarlin S, Tejesvi MV, Turunen J (2021) Impact of Streptococcus salivarius K12 on Nasopharyngeal and Saliva Microbiome: A Randomized Controlled Trial. Pediatr Infect Dis J 40(5): 394-402.
- Mitis Salivarius agar base. M259.pdf.
Editorial Manager:
Email:
pediatricdentistry@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...