Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6636
Research Article(ISSN: 2637-6636) 
Oral Status of Diabetic Children in Casablanca (Case- Control Study) Volume 2 - Issue 3
Benkirane L1*, Al Jalil Z2, Najjar K3, Lagouirah W4 and Bousfiha B5
- 1 Assistant Professor, Department of Pediatric Dentistry, School of Dentistry of Casablanca, Hassan II university, Casablanca, Morocco
- 2 Specialist, Pediatric Dentistry Service, Casablanca, Morocco
- 3,4 Private practice, Casablanca, Morocco
- 5 Professor, Department of Pediatric Dentistry, School of Dentistry of Casablanca, Hassan II university, Casablanca, Morocco
Received:January 22, 2019 Published: February 04, 2019
*Corresponding author:Benkirane L, Assistant Professor, Department of Pediatric Dentistry, School of Dentistry of Casablanca, Hassan II university, Casablanca, Morocco
DOI: 10.32474/IPDOAJ.2019.02.000140
Abstract
Objectives: This study aims to assess the oral health status of diabetic children in comparison with a control group, to appreciate the impact of diabetes mellitus and its treatment on oral and dental health and to test their knowledge regarding oral hygiene.
Material and Methods: This transversal epidemiological study with comparative purpose was conducted on 100 diabetic children aged 2 to 16 years followed in the service of the University Hospital of Pediatrics II HAROUCHI and within the association “Hayat” to support children with diabetes, and 100 healthy model children aged 3-15 years from two public schools and one private school. Through a questioning and an oral examination, the parameters of diabetes, oral and dental hygiene, and the dental status were determined.
Results: The DMF index was more pronounced in the patient group (2.933) than in the control group (1.798) with a statistically significant difference (p = 0.002). The mean Plaque index was 1.338 for the patient group versus 1.542 for the control group. In the group of sick children and tartar was present in 62% of cases.
Conclusion: In the waning of this study, it was shown that diabetes has a significant impact on teeth and oral health of children. Following these results, the oral care needs are high among the population of children with diabetes.
Keywords:Diabetes Mellitus; children; Dental Caries
Introduction
Type 1 diabetes or insulin-dependent diabetes is a common childhood chronic endocrinopathy resulting from a relative or absolute insulin deficiency, which leads to hyperglycemia and metabolism disorders of carbohydrates, proteins and fats. In the absence of a strict follow-up, it conducts to severe clinical features that may have negative impact on life quality of the child and his family. The World Health Organization (WHO) estimates that, Hyperglycemia is the third risk factor for premature mortality, after high blood pressure, obstructive pulmonary diseases and lung cancers [1]. Its incidence has been increased in the last 30 years among children and adolescents (from 0 to 15 years old) [2]. According to data from the International Diabetes Federation, more than half a million children under 15 years old are currently having type 1 diabetes [2,3]. In Morocco, as in the world, diabetes is expanding, about 100,000 children are already affected by type 1 diabetes, according to the Moroccan Association of Autoimmune and Systemic Diseases [4]. Since diabetes and tooth decay remain widespread chronic diseases, it became a major need to study the correlation between these two conditions. Frequent consumption of ferme carbohydrates is now recognized as one of the causes of tooth decay. Poorly controlled diabetes creates significant cariogenic changes in the oral environment including increased salivary glucose, decreased salivary secretion, lower buffering, and acidic pH [5]. All these changes in the oral microflora can significantly influence the prevalence of gingivitis and dental caries [6-9]. Considering the high prevalence of diabetes in Morocco, and since there is still some controversy about the impact of diabetes on oral and periodontal disease, an epidemiological survey was conducted to compare the oral health of children with type 1 diabetes and healthy children in our Moroccan context and to assess the correlation between diabetes and oral health.
Material and Methods
Study Design and Sample
A cross-sectional case-control study (diabetic and nondiabetic children) was conducted for comparative purposes by two calibrated practitioners from November 2015 to January 2016. The investigation took place in the department of Pediatrics II at the Abderrahim Harouchi Hospital, Ibn Rochd University Hospital Center and the Hayat Association for the Support of Diabetic Children in Casablanca. We enrolled 100 diabetic children in the cases group and 100 healthy children in the control group, from two public schools and one private school. They were assorted in terms of age, sex and residence area. All non-cooperating children or children experiencing a diabetes-associated pathologic condition were excluded from the diabetic group. Children suffering from a general pathology or treatment that may affect oral state were excluded from the control group. In order to calibrate the interviewers and validate the questionnaire, a pre-survey was first conducted with 15 children. These ones were excluded from the study.
Questionnaire
A patient survey form was developed with three parts, the first was related to the identification of the child, the second concerning diabetes (seniority, follow-up, severity and treatment) and the third one was basically focused on oral health status: Oral care habits and oral health status. The consent of the parents was obtained after they were informed of the nature of the work and the anonymity of the questionnaire.
Clinical Examination
The clinical examination was performed in well-lit rooms, using a mirror and Dental explorer 6 and 17.
Plaque accumulation was evaluated with Silness and Loe plaque index [10]. Caries were recorded according to DMF (The Decayedmissing- filled index) and DMF indexes [11].
Statistical Methods
The data processing was done using Epi-Info 6.0.fr. software. The Chi-2 test was used for percentages comparison, while Student’s test was applied to compare averages. A value of p < 0.05 was considered significant.
Results
Sociodemographic Status
The distribution by sex in our sample was 50% boys and 50% girls for the diabetic group and 55% girls versus 45% boys for the non-diabetic group. The sample age ranged between 2 to 16 years old with an average age of 10.01± 3.743 for the diabetic group, versus an age range from 3 to 15 years for the control group, with an average age of 9,5 years ±3, 103. 96% of sick subjects were from urban area, 2% were from per urban and 2% from rural area. For the control group, all subjects lived in urban areas. The primary/middle school level was the dominant mother’s education level within patients of the study group with a prevalence of 36%. University level was the main mother’s level of education in the control group with a rate of 53%. Regarding the socio-economic level, the average one was the most representative among diabetic children with a rate of 53%, while in the healthy group, it was mainly represented by the comfortable standards of living with a 42% prevalence.
Children with diabetes Information
The clinical symptoms revealing diabetes were mainly polyuria and thirst with respectively a prevalence of 94.6% and 92.4%. Mucosa burning sensation was reported in 11% of the patients. The average age of the diabetes onset was 6.45 years ±3.56. Children receiving 2 injections of insulin daily were about 47%, those receiving it 3 times a day were about 36% of the diabetic group. The percentage of glycosylated hemoglobin produced every 3 months ranged between 4 and 16% with an average of 8.315% ±1.904. Among diabetic group, 51% of cases had moderate diabetes, while 49% of the children examined had severe one. All the cases undertake Insulin therapy, 80% of them are following a diet and 77% had sport activity.
Eating Habits and Oral Hygiene
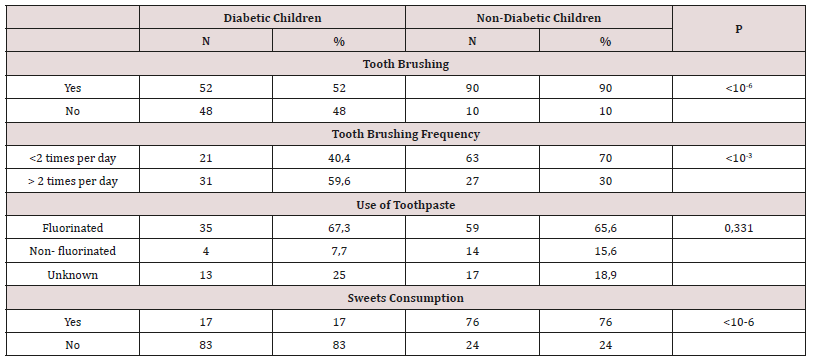
The distribution of patients according to eating habits and oral hygiene is shown in Table I.
Oral Status Information
Plaque Index
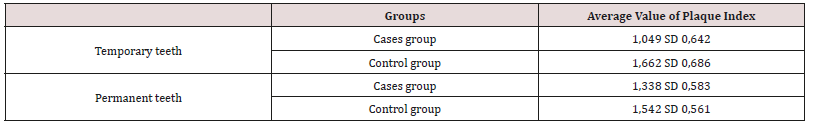
The difference observed between the cases group and the control group was statistically significant (p < 10-6), with a plaque index of temporary teeth and permanent teeth higher in nondiabetics compared to diabetic children (Table 2).
Dental Calculus
Dental calculus was detected in 62% of the sick children versus 24% in the control group (p < 10-6).
State of Dentition
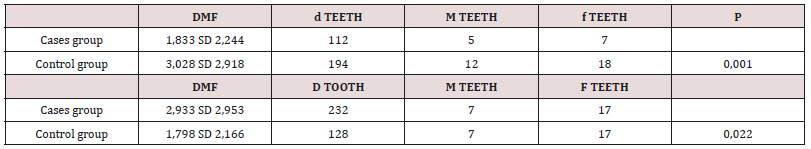
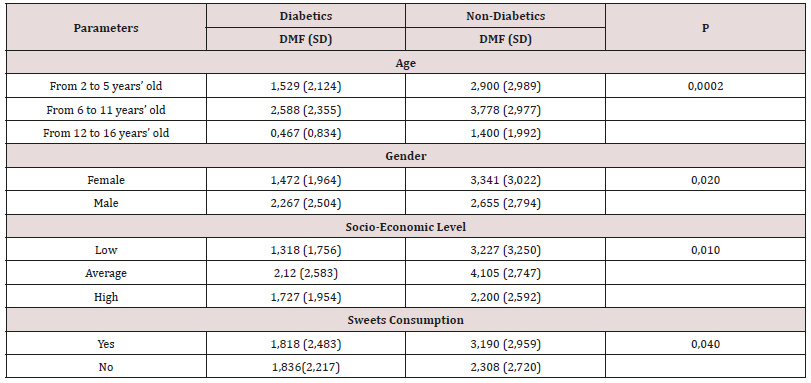
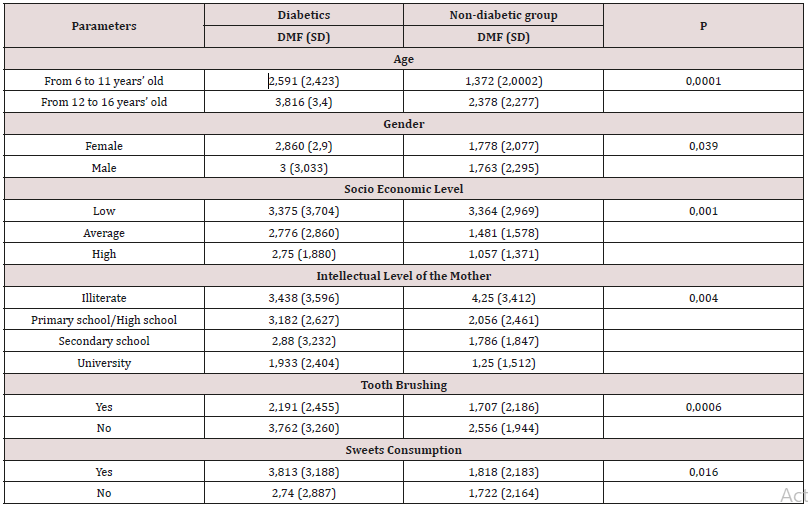
The DMF index was higher in the control group (3.028) compared to the cases group (1.833) with a statistically significant difference (p = 0.001). In contrast, the DMF index was more pronounced in the cases group (2.933) than in the control group (1.798) with a statistically significant difference (p = 0.002). This index increases with age and reaches a higher value among low socioeconomic children. There was a large predominance of decayed teeth compared to missing and filled ones regardless of dentition type and group (Table 3). The distribution of DMF and DMF indexes according to the studied parameters are listed in the following (Tables 4,5).
Discussion
The purpose of this study was to compare the oral status of 100 diabetic children with that of 100 control children by age, sex, place of residence and school setting (Tables 4,5). The questionnaire used for this purpose was extracted from WHO [12] in its oral section and from literature in the section about diabetes information. The majority of diabetic children and all healthy children were from urban areas, which is consistent with the results of a study conducted at the Kaunas School of Dentistry in Lithuania on diabetic children aged between 10 and 15 years old, showed that the vast majority of children came from urban areas [13]. The highest level of maternal education was the primary / middle school level for the cases group while it was predominantly the university level among the control group. In the city of Kaunas (Lithuania), the university level of the mother was dominant for the group of cases (54%) versus primary / college for the control group (44%). The least educated parents are the least receptive to the oral health education of their children. Regarding diabetes, the average age of its onset in our study was 6.45 years. This earlier onset diabetes has been confirmed by several reports including the Swedish register where, across five birth cohorts, the age of diagnosis has declined in the recent decades [14]. A Finnish work reports the same findings [15]. The experience of children’s hospital in Rabat states that the incidence of type 1 diabetes has tripled between 1990 and 2005 among children under 5 years old [16]. This early onset diabetes shift is still unexplained, although changes in the environment and its interaction with the genome have been attributed: viral infection rates, increased maternal age, diet, exposure to toxins. This tendency to lower the age of diabetes diagnosis has serious consequences, for example the interference with intercurrent febrile diseases, frequent at this age, the immaturity of the child to participate in its treatment, not to mention the increased risk of long-term degenerative complications [17].
Table 5: Distribution of DMF index by age, gender, socio-economic level, mother’s intellectual level and sweets consumption.
The average of glycated hemoglobin was 8.315% with two insulin injection per day (the most adopted). Similar findings were reported at the University Hospital of Santa Catrina in Sao Paulo [18]. The better the control of diabetes was, the lower the number of injections and the rate of complications is. The children reported following a balanced diet which is critical in the patient medical management in PII and Hayat association are 80%. Only 17% of diabetic children consumed sweets outside mealtimes, unlike the children of the control group, 76% of them did (the difference being statistically significant). The results of this study are consistent with those of the case-control study of Bassir L. et al. performed in Iran, where diabetic children consumed less cariogenic snacks than control children; snacks like cheese sandwich instead of cookies (P < 0.05). These habits could serve as dietary strategies in diabetic children [19]. Regarding oral hygiene habits, almost all of the control children are brushing their teeth against only 52% of children with diabetes. Brushing is mostly done independently in children whom average age is around 9,5 and 10 years. This statistically significant difference would be the result of parents’ concern about the illness and neglect of their child’s oral hygiene measures. The frequency of brushing was, however, higher in the children with diabetes (59.6%) compared to control children (30%). This higher brushing frequency associated with a lower consumption of sweet snacks may explain the lower value of plaque index in our diabetic children (for temporary and permanent teeth), the difference was statistically significant. (p< 10-6), These results are different from those of the Lydia and Lopez study, which showed that diabetic children had more plaque than control children and explained their results by xerostomia more present in sick children [20].
In addition, dental calculus was found in 62% of the cases compared to only 24% in the control group; these results are in agreement with those of the studies carried out in Lithuania, Puerto Rico and Sao Paulo [18,20,21]. The mineralization of dental plaque was caused by the dry mouth. Concerning the state of dentition and carious indexes, it was noticed in diabetic patients, especially in the age group 2 to 5 years old, that the DMF was lower than in the control group. It seems that parents of diabetic children were more vigilant about the diet recommended by the pediatrician, moreover, at this age, there is less environmental influence. As for the DMF index, regardless of gender, it was more important in diabetic patients, its value increased with age and was higher among children in both groups who did not brush their teeth. This finding is consistent with the scientific data. The higher DMF in the cases group may be partly explained by poor and irregular oral hygiene in diabetic children and teenagers, by the seniority of diabetes, its early onset (around 6.45 years of age), its complications such as dry mouth, and also probably by the underestimation of sweets consumption reported by children with diabetes. The DMF index found in this study was significantly higher than that reported by the Lopez del Valle study in Puerto Rico among 50 diabetics aged 6 to 12 years old, the DMF was about 1.43 for the cases group and 0.56 for the control group, with a statistically significant difference. The DMF index was higher in the 12 to 16 age group, age of revolt and opposition to oral hygiene and care. The high DMF in our diabetic adolescents remains lower than the one found in the Sarajevo study in diabetic patients aged 12 to 18 years old, it was 6.19 ± 2.54 and was strongly related to poor glycemic control [22]. Previous studies on this issue have revealed inconsistent results. In a systematic review of oral health in adolescents with Type 1 diabetes, five studies had a significantly higher DMF in children with type 1 diabetes compared to control group when three studies had significantly lower values and seven studies reported no difference between the two groups. The highest DMF index is found in children with low socioeconomic, whether they have diabetes or not, while the wealthy class has the lowest DMF index. This may be related to the ease of access to information and dental care in this socioeconomic category. Finally, the DMF index and the education level of the mother were inversely proportional. Indeed, the lower the level of education, the higher the DMF index was, this result seems to be related to the lack of information and motivation of inadequately educated mothers faced to the need to maintain good oral hygiene of their children.
Conclusion
Based on this case-control study’s results, we can highlight the negative effect of diabetes on oral health. The affected children have a higher DMF index compared to healthy children, dental calculus is also increased; However, besides the pathology, other contributing factors are, inadequacy of dental brushing, low level of education of the mother and parent’s preoccupation with the disease much more than oral health state. The odonto pediatrician is an actor of health in the diabetic disease but most of the time neglected in the medical care of diabetic children. It is of this fact, essential to remedy this lack of information and to establish community programs and actions of oral hygiene education, and this, at the level of parents and diabetes specialist, to improve the oral health and quality of life of our young diabetics.
References
- Colin Mathers, Gretchen Stevens, Maya Mascarenhas (2015) Global health risks mortality and burden of disease attributable to selected major risks. World Health Organization. (NLM classification: WA 105) © World Health Organization 2009 International Diabetes Federation Atlas. 7th Edn.
- Patterson C, Dahlquist G, Gyürüs E, Green A, Soltész G (2009) The EURODIAB Study Group. Incidence trends for childhood type 1 diabetes in Europe during 1989-2003 and predicted new cases 2005-20: A multicenter prospective registration study. Lancet 373(9680): 2027- 2033.
- Association marocaine des maladies auto-immunes et systémiques 100000 enfants diabétiques au Maroc LNT/MAP Nouvelle Tribune 2013.
- Stefano Lai, Maria Grazia Cagetti, Fabio Cocco, Cossellu D, Meloni G, et al. (2017) Evaluation of the difference in caries experience in diabetic and non-diabetic children, case control study. PLOS ONE 12(11): e0188451.
- Malicka B, Kaczmarek U, Skośkiewicz Malinowska K (2014) Prevalence of xerostomia and the salivary flow rate in diabetic patients. Adv Clin Exp Med 23(2): 225-233.
- R Rafatjou, Z Razavi, S Tayebi, M Khalili, M Farhadian (2016) Dental Health Status and Hygiene in Children and Adolescents with Type 1 Diabetes Mellitus. J Res Health Sci 16(3): 122-126.
- Leite RS, Marlow NM, Fernandes JK (2013) Oral health and type 2 diabetes. The American journal of the medical sciences 345(4): 271-273.
- Siudikiene J, Machiulskiene V, Nyvad B, Tenovuo J, Nedzelskiene I (2008) Dental caries increments and related factors in children with type 1 diabetes mellitus. Caries Res 42(5): 354-362.
- Löe H (1967) The Gingival Index, the Plaque Index and the Retention Index Systems. J Periodontol 38(6): 610-616.
- Klein H, Palmer CE (1940) Studies dental caries: a procedure for recording and statistical proceeding of dental examination findings. J Dent Res 19: 243-252.
- CJ Holmgren (1997) Oral Health Surveys: Basic Methods, 4th Ed., Geneva World Health Organization (NLM Classification: WU 30) © World Health Organization.
- Siudikiene J, Maciulskiene V, Nedzelskiene I (2005) Dietary and oral hygiene habits in children with type I diabetes mellitus related to dental caries. Stomatologija 7(2): 58-62.
- Pundziute Lycka A, Dahlquist G, Nystrom L, Arnqvist H, Bjork E, et al. (2002) The incidence of Type I diabetes has not increased but shifted to a younger age at diagnosis in the 0-34 years group in Sweden 1983- 1998. Diabetologia 45(6): 783-791.
- Harjutsalo V, Sjoberg L, Tuomilehto J (2008) Time trends in the incidence of type 1 diabetes in Finnish children: A cohort study. Lancet 371(9626):1777-1782.
- Imane Z, Amhager SN, Bennani NA, Balafrej A (2010) Epidemiology of Diabetes in Children Under 5: Experience of Pediatric Diabetology. Service Medicine of Metabolic Diseases 36 (1): A46.
- Lévy Marchal C (2010) The increase in incidence of type 1 diabetes: the reality of childhood diabetes Metabolic Disease Medicine 4(3): 326-331
- Carolina C Costa, Gimol B Resende, Joeci M Souza, Silvia S Tavares, Izabel CSS Almeida, et al. (2004) Filho Study of the oral manifestations in diabetic children and their correlation variables. Arq Bras Endocrinol Metab 48(3).
- L Bassir, R. Amani MK Masjedi, F Ahangarpor (2014) Relationship between Dietary Patterns and Dental Health in Type I Diabetic Children Compared with Healthy Controls. Iran Red Cres Med J 16(1): e9684.
- Lopez del Valle LM1, Ocasio Lopez C (2011) Comparing the oral health status of diabetic and non-diabetic children from Puerto Rico: A casecontrol pilot study. PR Health Sci J 30 (3): 123-127.
- Darwazeh AMG (1990) Diabetes mellitus, dental caries and periodontal disease: evidence for a relationship. Dental Health 29: 3-7.
- Rusmira Fazlić (2016) Differences in dental caries experience between diabetic adolescents and healthy controls. Journal of Health Sciences 6(1): 46-51.
- Ismail AF, McGrath CP, Yiu CK (2015) Oral health of children with type 1 diabetes mellitus: a systematic review Diabetes. Res Clin Pract 108(3): 369-381.
Editorial Manager:
Email:
pediatricdentistry@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...