
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6636
Case Report(ISSN: 2637-6636) 
Oral Squamous Papilloma on the Tongue of a 12-Year Old Female: Report of a Case with Human Papilloma Virus Literature Review Volume 2 - Issue 4
Cameron YS Lee DMD, MD, PHD, MPH1,2* and Kirk Y Hirata MD, MS3,4
- 1 Private Practice in Oral, Maxillofacial and Reconstructive Surgery, Hawaii, USA
- 2 Clinical Professor, Department of Periodontology and Oral Implantology, Kornberg School of Dentistry. Temple University, Philadelphia, PA 19140, USA
- 3 Staff Pathologist, The Queen’s Medical Center, Honolulu, HI 96813, USA
- 4 Associate Clinical Professor of Pathology, John A Burns School of Medicine, University of Hawaii, Honolulu, Hawaii 96813, USA
Received:March 11, 2019; Published: March 19, 2019
*Corresponding author:Cameron YS Lee, Private Practice in Oral, Maxillofacial and Reconstructive Surgery, Hawaii, USA Clinical Professor, Department of Periodontology and Oral Implantology, Kornberg School of Dentistry, Temple University, Philadelphia, USA
DOI: 10.32474/IPDOAJ.2019.02.000145
Abstract
Human papillomavirus (HPV) infection that causes squamous papilloma is common in the oral cavity of adults but not in children. Although benign, the slow progressive growth is a concern to clinicians and parents as the lesion may clinically appear as an exophytic verrucous carcinoma or squamous carcinoma. This case report describes a squamous papilloma arising on the tongue of a 12-year old child.
Keywords:Child; Human Papillomavirus (HPV); Squamous Papilloma; Oncogenic Potential; Tongue; Koilocytes
Introduction
Human papillomavirus (HPV) are slow, benign proliferations of stratified squamous epithelium frequently observed in the oral cavity that are the viral etiologic agent for squamous papilloma [1,2]. Squamous papillomata are commonly observed in adults 30-50 years of age and is the fourth most common oral mucosal lesion in both children and adults [3]. Although the entire oral cavity may be affected, the viral lesion has a predilection for the laryngotracheobronchial complex in children and the lower lip, hard and soft palate of the maxilla and uvula in adults [1,4-6]. Clinically, the lesion appears as an exophytic mass and may cause anxiety to the clinician and parents, as the lesion can clinically appear like an exophytic verrucous carcinoma, squamous carcinoma or condyloma accuminatum [1,4,7,8]. This case report describes a squamous papilloma arising on the tongue of a 12-year old child.
Virology
The human papillomavirus is a 55nm non-enveloped icosahedral double-stranded deoxyribonucleic acid (DNA) virus that is a member of the papovavirus group [7-14]. There are over 150 genotypically different types and classified as either mucosal or cutaneous.10-12 The viral types with oncogenic potential include HPVs 16, 18, 31, 33, 35, 39, 45, 51, 55, 56, 58, 59, 66 and 68. Oral squamous papilloma infection is associated with HPV subtypes 6, 11 and 16 [7-13]. Papillomas induced by HPV types 6 and 11 are considered to have low oncogenic potential. However, approximately 85% of dysplastic lesions, carcinoma in situ and squamous cell carcinoma involve the DNA sequence of HPV 16 and 18. DNA replication of HPV occurs in the nuclei of epithelial cells. The HPV capsid proteins enter the host cell delivering the viral DNA to the nucleus which allows proliferation of the viral lesion [7,10,11,12,14].
Case Report
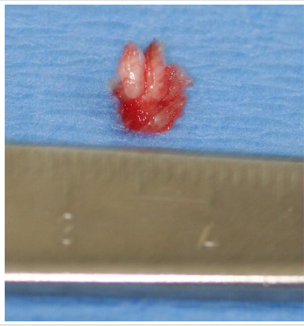
A 12-year old Asian female was referred to the office by her family dentist for evaluation of a soft tissue lesion localized to the dorsal surface of the tongue (Figure 1). The patient stated that the lesion has been present for at least six months. Her past medical history was unremarkable. She was not taking any medications and denied any allergy to medications. The patient also denies being sexually active. Sexual abuse was also ruled-out. Head and neck examination were negative for palpable neck masses and lymphadenopathy. Oral examination of the dorsal surface of the tongue revealed a pink-white colored exophytic lesion that was freely movable. The surface texture had a pebbly appearance that resembled, “cauliflower”. The remaining oral examination was unremarkable. Examination of the upper and lower extremities was negative for any soft tissue lesions resembling HPV. Based on the clinical appearance of the lesion, the differential diagnosis included squamous papilloma, verruciform xanthoma, papillary hyperplasia and condyloma accuminatum of the tongue. The father and patient were informed of the clinical findings and excisional biopsy (Figure 2) for a definitive microscopic diagnosis under local anesthesia was recommended.
Figure 1: Clinical photograph of squamous papilloma on left dorsal surface of the tongue in 12-year old Asian child.

Figure 2: Excised squamous papilloma specimen from dorsal surface of tongue of 12-year old Asian patient.
Histopathology
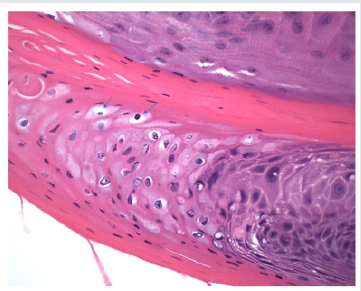
Excisional biopsy was completed under local anesthesia with 1.0mm margins of normal tissue and to the depth of the tongue musculature. The lesion was stained with hematoxylin and eosin for histopathological diagnosis. Histological examination demonstrated long, thin papillary projections of parakeratinized stratified squamous epithelium (Figure 3a). Localized areas of basilar hyperplasia with koilocytes were observed (Figure 3b). The histological findings were consistent with squamous papilloma.
Figure 3(a): Histopathology demonstrating proliferation of hyper keratinized stratified squamous epithelium finger-like projections with thin fibrovascular connective tissue core (Hematoxylin and eosin stain. Original magnification x 40).
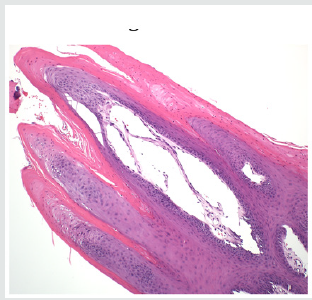
Figure 3(b): Presence of koilocytes (arrows) in the spinous layer of the epithelium that are characteristic histopathologic findings of oral squamous papilloma (Hematoxylin and eosin stain, x 200).
Discussion
In children, viral transmission remains controversial. HPV transmission may occur by any number of different mechanisms, such as autoinoculation, heteroinoculation, perinatal transmission, sexual abuse and contact with fomites [1,4,5,9,10]. However, trauma is one mechanism that should be considered in our patient. Iatrogenic tongue biting may initiate an infection of the basal squamous epithelial cells that allows the entrance of the HPV into the tongue. Viral DNA then enters the nucleus of the infected epithelial stem cells and can replicate causing the HPV infection [15]. Histopathologic features of oral squamous papilloma demonstrate hyperkeratosis in the epithelium, proliferation of the spinous cells that result in long, thin finger-like projections above the mucosa [1- 3,8,14]. The characteristic feature of HPV infection is the presence of koilocytes (Figure 3b) which are virus-infected epithelial cells due to perinuclear cytoplasmic vacuolization of cells of the spinous layer of the epithelium. This results in the nuclei becoming pyknotic and cremated surrounded by an optically clear zone [1-10]. All the described histopathologic findings in our patient are characteristic of HPV infection. Although the prevalence of oral HPV infection is low, a bimodal distribution is observed. The highest prevalence is observed in children less than 1 year of age and the second peak occurs in adolescents, between 13 to 20 years old [9,16]. Despite the bimodal distribution, oral HPV infection is considered low in children [17]. In a study of 4140 children between the ages of 10 to 18 years old, the prevalence of oral HPV infection was 1% and the most common type was HPV 11 [18]. Treatment of HPV is by surgical excision [19]. The United States Food and Drug Administration (2016) approved Gardasil 9 human papillomavirus 9-valent vaccine to prevent infection against HPV types 6, 11, 16 and 18 (Merck & Co., North Wales, Pa). At present, only Gardasil 9 human papillomavirus 9-valent vaccine recombinant has been approved for vaccination in the United States (Center for Disease Control, 2019) [20]. To obtain the greatest clinical efficacy and cost effectiveness of vaccination, the Center for Disease Control (CDC) recommends that both male and female children between the ages of 11-12 years get two HPV vaccinations six months apart before individuals have been exposed to the human papillomavirus. It is also recommended that adult women up to age 26 years and men up to age 21 years also obtain the HPV vaccine [21].
Conclusion
A case of oral squamous papilloma on the tongue of a 12-year old female is presented to create awareness of this soft tissue lesion in the oral cavity of children due to the human papillomavirus. It is only after educating clinicians and parents about the HPV will we observe greater identification, management and treatment in the HPV infected child.
References
- Abbey LM, Page DG, Sawyer DR (1980) The clinical and histopathologic features of a series of 464 oral squamous cell papillomas. Oral Surg Oral Med Oral Pathol 49(5): 419-428.
- Das S, Das AK (1993) A review of pediatric oral biopsies from a surgical pathology service in a dental school. Pediatric Dent 15(3): 208-211.
- Neville BW, Damm DD, Allen CM (2009) Epithelial pathology. In: Textbook of oral and maxillofacial pathology. Ed 3rd. Elsevier, pp. 362- 364.
- Syrjanen S (2010) Current concepts on human papillomavirus infections in children. APMIS 118(6-7): 494-509.
- Castro TP, Bussoloti Filho I (2006) Prevalence of human papillomavirus (HPV) in oral cavity and oropharynx. Braz J Otorhinolaryngol 72(2): 272-282.
- Naik S, Nidoni M (2014) Oral squamous papilloma of the palate- a case report. Int J Dent Sci Res 2 (6B): 17-18.
- Sanclemente G, Gill DK (2002) Human papillomavirus molecular biology and pathogenesis. J Eur Acad Dermatol Venereol 16(3): 231-240.
- Carneiro TE, Marinho SA, Verli FD, Mesquita AT, Lima NL, et al. (2009) Oral squamous papilloma: Clinical, histologic, and immunohistochemical analyses. J Oral Sci 51(3): 367-372.
- Summergill KF, Smith EM, Levy BT, Allen JM, Haugen TH, et al. (2001) Human papillomavirus in the oral cavities of children and adolescents. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 91(1): 62-69.
- Mammas IN, Sourvinos G, Spandidos D (2014) The paediatric story of human papilloma virus (HPV). Oncol Lett 8(2): 502-506.
- Feller L, Hammissa RA, Wood NH, Lemmer J (2009) Epithelial maturation and molecular biology of oral HPV. Infect Agent Cancer 4: 16-23.
- Swygart C (1997) Human papillomavirus: disease and laboratory diagnosis. Br J Biomed Sci 54(4): 299-303.
- Major T, Szarka K, Sziklai I, Gergely L, Czegledy J (2005) The characteristics of human papillomavirus DNA in head and neck cancers and papillomas. J Clin Pathol 58(1): 51-55.
- Park JS, Hur S (2013) Up to date: Comprehensive knowledge of human papillomavirus. Expert Rev Vaccines 12(4): 353-355.
- Egawa K (2003) Do human papillomaviruses target epidermal stem cells? Dermatology 207(3): 251-254.
- Smith EM, Swarnavel S, Ritchie JM, Wang D, Haugen TH, et al. (2007) Prevalence of human papillomavirus in the oral cavity/oropharynx in a large population of children and adolescents. Pediatr Infect Dis J 26: 836-840.
- Ilea A, Miclaus V, Babtan AM, Mesaros A, Crisan B, et al. (2015) Oral human papillomavirus in children. The pediatric infectious disease journal 35(2): 65-68.
- Durzynska J, Pacholska Bogalska J, Kaczmarek M, Tomasz H, Magdalena D, et al. (2011) HPV genotypes in the oral cavity/oropharynx of children and adolescents: cross-sectional survey in Poland. Eur J Pediatr 170(6): 757-761.
- Shafer WG, Hine KH, Levy BM (1983) Oral cavity benign and malignant tumors. In: A textbook of oral pathology. Saunders Philadelphia, USA, pp. 80-82.
- (2019) Human Papillomavirus (HPV) Vaccines.
- (2019) Centers for Disease Control and Prevention. Recommended Child and Adolescent Immunization Schedule for Ages 18 or Younger, USA.
Editorial Manager:
Email:
pediatricdentistry@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




