Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6636
Research Article(ISSN: 2637-6636) 
Experiences of Mothers of Affected Children on Family Impact of Amelogenesis Imperfecta: Findings of A Qualitative Explorative Study From Sri Lanka Volume 6 - Issue 5
Chandra Herath1, Irosha Perera2*, Primali Jayasooriya3 and Manosha Perera4
1Division of Paedodontics, Department of Community Dental Health, Faculty of Dental Sciences, University of Peradeniya, Sri Lanka
2Preventive Oral Health Unit, National Dental Hospital (Teaching) Sri Lanka, Sri Lanka
3Department of Oral Pathology, Faculty of Dental Sciences, University of Peradeniya, Sri Lanka
4Alumnus, School of Dentistry and Oral Health, Griffith University, Australia
Received:August 24, 2021 Published: September 02, 2021
*Corresponding author: Irosha Perera, Preventive Oral Health Unit, National Dental Hospital (Teaching), Sri Lanka
DOI: 10.32474/IPDOAJ.2021.06.000246
Abstract
Background: Amelogenesis Imperfecta (AI) denotes a heterogenous group of conditions characterized by inherited enamel defects among children which affect the structure and clinical appearance of the enamel of teeth of primary and permanent dentitions. Hence, it is well known that AI negatively impact on families and parents especially mothers and fathers as primary caregivers of affected children. However, little is known on the context in developing countries in this regard. Objective: To explore the experiences of mothers in Sri Lanka: a developing middle-income country on the family impact of having a child affected by Amelogenesis Imperfecta (AI).
Study design: A qualitative, explorative study was conducted among mothers of children having confirmed diagnoses of AI attended the Pediatric Dentistry Department, Faculty of Dental Sciences; University of Peradeniya. A series of semi-structured interviews were conducted among mothers of affected children prior to commencing treatment. The Family Impact Scale (FIS) of Locker 2002, was used for the interviewer guide. Thematic analysis was conducted to analyze the transcribed interviews.
Results: Participating mothers expressed their deep concern about having a child with AI in terms of disturbed parental/family activities, negative parental emotions and family conflict. Furthermore, mothers were much worried about quality present and future of life of their children.
Conclusions: Present findings supported the need for emotional support for mothers receiving treatment for AI. Moreover, suitability of the 4-dimensional- Family Impact Scale as a theoretical framework for family impact assessment of having children with AI in a developing country context was indicated by the findings. Explicit theoretical framework-based family impact assessment might enhance child and family- centered treatment outcomes in longstanding management of children with inherited developmental defects of teeth and craniofacial complex such as AI. Nevertheless, further research warranted to confirm the present findings.
Keywords: Amelogenesis Imperfecta; Family Impact; theoretical framework; Sri Lanka
Background
Teeth contribute to essential daily functions such as eating, speaking, smiling, aesthetics and overall quality of life of an individual. Importantly, the appearance of teeth is fundamental to facial attractiveness of children and adolescents. An aesthetically pleasing face with attractive smile ranks first among all other attributes of attractiveness of an individual [1]. Amelogenesis Imperfecta (AI) denotes a heterogenous hereditary development disorder characterized by enamel defects which affect the structure and clinical appearance of enamel of all or nearly all teeth of primary and permanent dentitions [2,3]. Further, AI is associated with mutations in five genes (AMEL; ENAM; MMP20; KLK4 and FAM83H) giving rise to a wide range of clinical presentations (phenotypes) [4]. The reported global prevalence of AI paints the portrait of a picture of variations ranging from 1:700 to 1: 14000 with population and geographic specificities [2]. The clinical presentation of AI could be hypoplastic (deficient enamel), or hypomineralized (poorly mineralized enamel) with autosomal dominant, recessive and x-linked inheritance as well as some patients demonstrating sporadic inheritance [2-4].
As a consequence, the colour of the affected teeth may vary from normal to opaque, white or yellow-brown Furthermore, affected teeth are weak and prone to damage as well as susceptible to dental caries [5,6]. Hence, the negative outcomes of AI could be summarized as significant tooth disfiguration, tooth substance loss, sensitivity, increased calculus formation and risk of gingivitis and dental caries, loss of vertical dimension and the requirement for committed life-long oral health care [2-7]. As a consequence, long term management of children with AI by provision of restorative dental treatment coupled with preventive oral health care becomes essential. AI, therefore, poses a considerable challenge not only for affected children, but for their parental care givers, the Pediatric Dental Surgeons and the oral health care service provision of a country (Figure 1). The visible unaesthetic appearance of AI affected teeth compounded by sensitivity could give rise to a significant psycho-social impact on affected children and adolescents such as negative self-perception, emotional disturbance, inhibited interactions, being teased/bullied, anxiety, low self -esteem, learning disabilities, low school achievement and social withdrawal [4,8-12]. Coffield et al. [13], reported that having AI impacted on the psychosocial health of affected people especially at younger ages such as social avoidance and distress, higher levels of discomfort, dysfunction and high fear for negative evaluation. Moreover, there is evidence to support that oro-facial and dental anomalies affecting aesthetics of teeth could be an important cause for children and adolescents to being subjected for bullying at school and even at their home environments [14-17]. Childhood chronic conditions could severely impact not only on the affected child but the whole family disturbing usual family routines and adding financial burden as the given conditions need frequent use of health care facilities [13,14,17]. Therefore, childhood oro-facial conditions have an overarching impact on the family [13,14,17].
Accordingly, the children affected by AI may aggravate the existing negative emotional status of their parental caregivers. For example, a recent qualitative study conducted among a group of Irish parents having children affected by AI and Dentinogenesis Imperfecta revealed that the parents thought their young children were aware of the different dental appearance they had [15]. Moreover, fathers who did have same conditions reported that they were feeling guilty for passing the diseases to their offspring [14,15]. In addition, the majority of parents who sought dental treatment for their children prior to commencing schooling were promulgated by worries of getting the children bullied at schools [14,15]. Therefore, as, craniofacial anomalies could significantly influence the quality of life of affected children and their families, family impact assessment has garnered importance in health research as highlighted by Locker et al., 16. Further, as the pivotal role in child’s health is being played by the parents, health care interventions should address parental concerns and needs as that of the child’s [14,17]. In addition, the parental reports on child’s condition may be influenced by the degree to which the parental care givers are being psychologically and socially affected by child’s condition [15-17]. Moreover, there is controversy on effectiveness of restorative dental treatment for teeth affected by AI as treatment failures are quite common. For example, studies have shown that longevity of composite resin restorations is significantly lower in patients with AI and those patients require frequent replacements of fillings.
On the contrary, there is research evidence to suggest that definitive restorative treatment could improve the quality of life of children affected by AI [17]. Nevertheless, a Cochrane Systematic review revealed that there is currently insufficient reliable evidence to support which of these treatments are more effective [18]. Furthermore, AI has garnered paradigm shift in research interest from clinical perspectives to public health through to molecular/genetic perspectives [6-20]. Findings of such research could enhance patient and family- centered care and optimized treatment outcomes for children affected by AI pertaining to risk assessment and provision of precision restorative treatment [19- 21]. AI is a hereditary disease. It has no cure, and is associated with fractures of teeth, pain, loss of restorations, frequent emergency visits, and decreased oral health-related quality of life, factors all that could contribute to increased stress in the family [21]. Against this backdrop, present manuscript aimed to qualitatively explore the perceived family impact of mothers having children affected by AI using the dimensions of Family Impact Scale (FIS) of Locker [16]. It was a component of a comprehensive study to assess occurrence, clinical sub-types, socio-demographic background, and family impact as well as treatment outcomes of children diagnosed with AI attended the Department of Pediatric Dentistry, Faculty of Dental Sciences Peradeniya, University of Peradeniya, Sri Lanka. Some data on socio-demographic background, family impact and histological sub-type details of AI have been published previously [6,20].
Methods
Ethics approval
Ethical approval for the present study was obtained from the Faculty Research Committee, Faculty of Dental Sciences, University of Peradeniya, Sri Lanka (RERC/2009/11/HERATH1).
Study design
A qualitative exploratory study design was used among a purposive sample of mothers of children diagnosed with AI who attended the Department of Paediatric Dentistry, Faculty of Dental Sciences, University of Peradeniya Sri Lanka with their children.
Data collection Instrument
Data collection instrument was a semi-structured interviewer guide. An extensive literature search and evidence synthesis was conducted on psychometric scales and different study instruments used for assessment of family impact as well as psycho-social impact on oral and oro-facial anomalies of children and adolescents. Of them the 14-item- Family Impact Scale (FIS) to assess oro-facial anomalies developed by Locker [16] was chosen by the researchers as the most suitable scale for the semi-structured interviewer guide for the present study. The original English version FIS scale was first translated into native Sinhala language and then translated backward into English language by independent translators. It was pre-tested among a group of mothers having children with Cleft Lip and Palate prior to corrective surgery who attended the Oral & Maxillo-Facial Unit of a rural Provincial General Hospital in Sri Lanka, which provided a similar socio-cultural setting for the present study. Necessary modifications were made to the interviewer guide based on the findings of pretesting to improve the clarity. Data were collected using face-to-face, semi structured interviews with mothers of children affected by AI aimed at collecting comprehensive, flexible and respondent- centred mode to gain in-depth understanding on perspectives of family impact. In-depth interviews and data collection were conducted by the Principal Investigator thus overcoming the inter-interviewer variability. Basic socio-demographic information of the mothers was collected prior to conducting the interview. Interviews were conducted prior to starting treatment for children diagnosed with AI (Figure 2).
Children were allowed to play in the ‘playroom’ of the Department of Pedodontics specifically designed with an attractive, child-friendly environment with toys and story books while mothers were being interviewed. This ‘playroom’ also served the purpose of acclimatization of children to dental treatment as well as to gain their co-operation. Firstly, the participating mothers were welcomed with greetings. The purpose of the study and the procedure were explained in simple native language. Both verbal and written informed consent followed by a 3-week consideration period were obtained. They were clearly informed that participation in the study was entirely on voluntary basis without any compromise to comprehensive oral health care services for their children affected by AI. Each respondent was allocated a pseudonym for the duration of interview to safeguard their identity and confidentiality. All the interviews were conducted by the principal investigator (CH) who is experienced in conducting qualitative research. Maternal respondents were approached in a courteous and comforting manner to talk and express their feelings and perceptions in an uninhibited manner. The audio content of the interviews was digitally recorded (Digital Voice Recorder WS-813; Olympus) and transcribed in verbatim.
Theoretical basis
The topic guide was based on 4-dimensions of Family Impact Scale of Locker [16]. Maternal respondents were inquired about how the teeth condition of their children affected their families in terms of dimensions of parental/ family impact, parental emotions, family conflict, financial burden and an additional question on mothers’ perception on how child’s teeth condition has had impact on the quality of life of the child in the past, present and future contexts. Moreover, during the interviews participants were made comfortable to share their first-hand experience without restricting them only to the interviewer guide.
Data Analysis
The transcripts were subsequently subjected to concurrent analysis to arrive at data saturation without emergence of new experiences and perceptions. The data analysis was performed using thematic approach which comprised of an iterative process that involved reading of the verbatim transcripts many a times. Two researchers (CH and IP) performed familiarization with the transcripts using first 8 interviews. Subsequently each researcher (CH, PI, PJ & MP) independently and meticulously went through the transcripts to identify the relevant themes, sub themes and repetitions that emerged from the data. Controversies in clarity and content with regard to categorizing into respective themes and sub themes were resolved by discussing among researchers. Agreement was arrived at all aspects by this endeavor.
Results
Participants
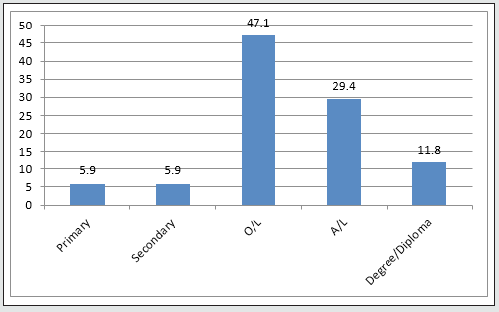
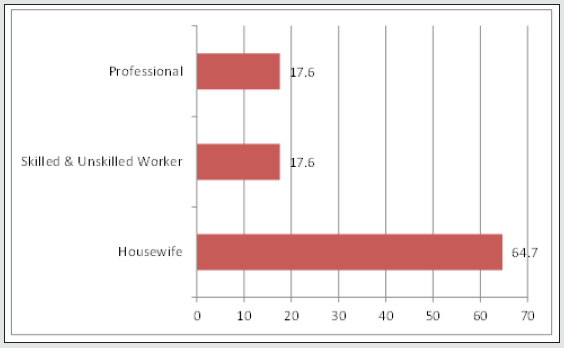
A total of 17 mothers participated in the present study. All mothers of at least one child diagnosed with AI. Of 10 out of 17 had family history of AI. The mean age of maternal respondents was 39.24 (± 5.48). The mean age of the children was 11. 29 (± 3.38) years, ranging from 3 to 16 years. Moreover, 10 out of 17 had family history of AI. The mothers represented 3 main ethnic groups in the country dominated by Sinhalese (64.7%), Tamil (11.8%) and Moor (23.5%). The occupational and educational status of the fathers and mothers is shown in Figures 1 & 2. Parents presented with varying levels of educational attainments. Accordingly, the majority 47.1% of them had completed General Certificate of Education-Ordinary Level (GCE-O/L) which is below the high school level equivalent and another 29.4% had accomplished GCE-Advanced Level (Figure 1). The overwhelming majority (64.7%) of fathers of children affected by AI were employed as skilled and unskilled manual workers and 23.5% were self-employed. Of mothers, the majority (64.7%) were housewives fully devoted for child rearing and household chores and only 35.3% of mothers were employed as skilled and unskilled manual workers (17.6%) and professionals (17.6%) (Figure,2). In overall, the children and their families predominantly represented lower middle socioeconomic group.
Perceived family impact of having children affected by AI
The four main themes and sub themes emerged from the interviews of mothers affected by AI were the parental/ family impact, parental emotions, family conflict, financial burden and the additional theme of child’s quality of life. Each theme has subthemes are schematically presented in Figure 1.
Parental/Family Activity
Interruption to Parental/family activity
This dimension of FIS inquired how parental/family activities were affected by the unsightly teeth condition of the child in 5-subdimensions ranging from work loss to interrupted family activities. Engaging in family activities, i.e., going for a family event such as a wedding ceremony, party, family outings etc. are some examples. In Sri Lankan socio-cultural context, family bond and extended families especially in rural context is highly valued and venerated. Participation of families i.e., parents and children together for various social events is a usual practice. ur family recently went for a wedding ceremony of a close relative of my husband. It was a family gathering. My daughter started having fun with her cousins and she was playing and smiling. People noted the bad colour of front teeth of my little daughter and they started inquiring about it especially the older ones. As the mother I became tearful immediately and I could not provide an answer…..!! (Kamala). I become embarrassed and sad when people start becoming curious about the bad colour of my 10-year-old son’s teeth when we take part in family events. I just can’t bear up when he becomes sad in such encounters! (Kumari)
Interference to work of the mother
According to Sri Lankan socio-cultural context the majority of mothers tend to be full-time housewives looking after children and engaging in household chores. However, cooking, washing, cleaning, accompanying children to schools, gardening keep the mothers busy much time. Hence, the theme was re-phrased as how child’s condition affected mother’s household chores. “When my baby was born I and my husband were beaming with happiness. She was so pretty. I expected pearly white teeth for her. When I think of the bad colour of her teeth I often get distracted and at times I cannot do my routine household work properly. My husband is employed as an Executive in a Private Bank. It is difficult for him to take leave from work (Nishani). I am a primary school Teacher by profession. Today there is an art exhibition at school and my presence was most needed, but I could not postpone coming over here to get the necessary treatment for my son who is 8 years old as his front teeth are badly discolored (Thamara).
Has your child required more attention from you or the other parent?
Family bond is very strong in Sri Lankan socio-cultural context. Until reaching adulthood and finding employment in major cities or given in marriage, children do tend to live with their parents. Children living in a closely knit-family structure do seek attention from their parents in general. When a child is affected by AI with badly discolored teeth and feeling pain and sensitivity quite often he or she tend to seek much attention from parents and especially from the mother. Responding mothers shared their experience in this regard. “ My daughter seems so upset with the look of her teeth. She asks a series questions from me about it and as she has been receiving some comments from her friends. Hence, now she wants me to pay more attention to her than for her younger brother. Especially on days when she’s upset she wants me to feed her food and at times to carry her and console her. Sometimes, she expects the same from her father too”( Seetha). “ My son finds it very difficult to brush his pitted bad coloured teeth. Though he is 11-years old, I got to brush his teeth daily in the morning as he is trying to escape from brushing teeth saying they hurt. I use a soft brush and slowly brush his teeth trying my best to minimize his pain. Sometimes, I can’t do a proper job thinking that he is in pain while brushing his teeth. At night it becomes even worse as he tries to go to sleep without brushing his teeth if I do not pay my attention” (Nandani). “My son’s teeth have become discoulered and I think they are brittle too. He finds it difficult to eat some food like pickles and ice-cream. I just saw a hole in one of his back tooth. He complaints of toothache as well. I am sad, as I do try my best to pay much attention to him sometimes neglecting my other two children” (Nalini).
Have Mothers had less time for themselves or other family members
Mothers hardly take time off to look after themselves leaving their children behind in rural Sri Lankan socio-cultural context. Nevertheless, within the perspective of extended family system, at times they got to take care of their older parents. Having children with oral or oro-facial conditions could add extra burden to such mothers. “I used to go to the beauty palour very often before marriage as I do like to look good. With my daughter’s teeth problem, I am always in a bad mood. I spend my time to look after my daughter and accompanying her to school back and forth as I do not want anyone to bully her or to pass bad remarks at her. Now I have not visited a beauty palour for ages” (Shyama). “My husband is the only child in his family, and we live in his ancestral home with his parents. Both of them are ailing and hardly mobile. As my husband is a Police Officer having much demanding work I got to look after his parents. Recently I got to employ a domestic helper to attend to them as I am fully occupied with my son having this bad teeth. He is very unhappy at times because of this, and I got to console him all the time! (Lalitha).
Interrupted Sleep of Mothers
In general, mothers provide the predominant source of care and sense-of-security for their children. One of the contrast phenomenon of child rearing practice compared to Western countries among Sri Lankan families is children sharing the same bed to sleep with their parents especially the mother until they grew up. Such a context not only might provide a renewed bond between the mother and the child, yet holding a child affected by AI, could make a mother constantly bearing the enormous burden of its impact subconsciously even at sleep. “ My two children sleep with me at night holding me tight. My youngest son is having badly stained teeth many a-times my sleep gets disturbed as I see bad dreams: the bad look of my son’s teeth seems deeply ingrained into my subconscious mind” (Sumana)“ I brush my child’s teeth which have become badly discoloured and brittle. Each time when I see her brownish set of teeth I cannot bear up….why my bundle of joy could not get a set of normal looking teeth. She sleeps with me at night holding me tight and I find it difficult to fall asleep at night as I keep on thinking of my precious child” (Geetha)
Parental Emotions
Being Upset
This sub-dimension inquired as to which extent mothers were upset with the appearance and problems with teeth of her child and its negative consequence of their affected children. I have been dreaming of having a healthy beautiful baby. But my daughter is having brownish set of teeth. When she smiles or talk people keep on asking as to what’s wrong with her teeth that makes me terrible and upset (Kamaladevi, 36 years).
Feeling Guilty
When people start curiously staring and questioning about brown coloured and brittle front teeth I get hurt and upset. Some of them have asked whether I have not given her vitamins and calcium or even whether I have not brushed here teeth properly. That makes me feel guilty too! (Sunethra). I do feel guilty about the colour and condition of my daughter’s teeth. I am having brownish teeth as well. Have I passed bad genes to my daughter? Or is it due to akusal (sins) from my previous birth??? I don’t know…..Chaya.
Worrying about the child having fewer life opportunities
In Sri Lankan socio-cultural context mothers (and fathers) indulge in two great expectations: firstly, to give a daughter/son in marriage and secondly to educate them well. Displaying a beautiful smile at the wedding ceremony is expected from the bride and mothers having daughters affected by AI got deep concerns about their daughters in this regard. Accordingly, in the present study almost all the responding mothers expressed their deep concerns on hindrance to academic success and career opportunities for their sons and daughters.
Feeling uncomfortable when others inquired about tooth condition of their child
The majority of mothers expressed how they become uncomfortable when others inquired about tooth condition of their child with AI due to poor aesthetics. As revealed by the mothers, the negative emotions of feeling upset, sad and guilty was mostly perpetrated during family activities with the local communities which was much inherent to rural Sri Lankan socio-cultural context.
Family Conflict
Arguments within the family could arise due to many reasons. Nevertheless, family conflict due to having a child affected by AI was more common among having adolescent children with AI.
Has your child argued with you?
“At times my son argues with me for having discolored teeth while all his cousins have normal looking teeth. Sometimes he becomes aggressive especially on days when his classmates crack jokes at him. I’m afraid when he grows older I don’t know how he would behave!” , Nanda.
Has your child been jealous with other siblings?
“ I have noted my daughter seems jealous with her brother. She compares looks of her teeth with her own brother. I am worried about this behavior of my daughter and feeling bad about her future! Uma- 40 years.
Child blames you or other parent
In Sri Lankan socio-cultural context of closely knit family structure, there was no report from mothers on children blaming their parents on bad status of their teeth. However, adolescent children affected by AI were more prone to argue with parents on unsatisfactory appearance of their teeth and the problems they encountered with them.
Disagreement in Family
“My husband at times accuses me that my side got bad genes as if the discolored teeth of my daughter were from my side. There are my cousins who got discolored teeth. At times there is disagreement in our family” –Mala 35 years.
Financial Burden
As the dental care services are provided free of charge at the point of service delivery, financial burden was not a considerable problem as perceived by mothers having children with AI in Sri Lankan context compared to other dimensions of FIS. Nevertheless, some mothers expressed their concern on losing their daily income when both parents got to seek oral health care services more often for their children,
Worried About Quality-Of-Life Affected Children
As revealed by the findings, the majority of mothers expressed their worries about quality of life of their affected children with AI in the past, present and for the future pertaining to academic performance, career opportunities and finding prospective partners for marriage.
Discussion
Present study explored mothers’ perceptions and experience on family impact of having children affected by AI using the 4-dimensions of the Family Impact Scale (FIS) [16]. FIS investigates the impact of child’s oro-facial and oral condition on daily life of the family providing the theoretical framework of dimensions/ constructs. It has been translated and validated into many languages [16]. It comprised of 14-items divided into four subscales: parental/family activity, parental emotions, family conflict and financial burden. Present study aimed to qualitatively explore the applicability of 4- broad dimensions of FIS scale. According to the knowledge of researchers this study is the first qualitative exploration on perceived family impact of mothers having children affected by AI in Sri Lankan socio-cultural context. Mothers expressed their serious concerns on parental/family activity, parental emotions and affected quality of life of their children. These findings were in agreement with previous qualitative studies conducted among parental caregivers of children affected by oral and oro-facial anomalies [16,17,21,22].
For example, a recent study conducted by Lundgren et al. that being a parent to a child of severe forms of amelogenesis imperfecta gave rise to feelings of guilt for having passed on a hereditary disease, stress associated with all aspects of dental care, as well as feeling of extra responsibility for the child’s wellbeing compounded by uncertainty about the future [17]. The feeling of guilt is grounded to the experience of stigma with regard to a genetic disorder [14,15]. Moreover, further supporting the findings of the present study, Lundgren et al. reported that both parents and their children had been bullied due to the unaesthetic appearance of their teeth and consequent restricted engagement in communities [17]. Four main themes emerged from the interviews in that study were: feelings associated with passing on a hereditary disorder, knowledge decreases stress, unfamiliarity with the diagnosis, and psychosocial stress. The sub-themes identified were guilt/shame; knowledge about diagnosis in the family and support from dental health care professionals; missed diagnosis, fear of not getting correct treatment, and insufficient pain control and fear of child being bullied and emergency dental visits [23]. Supported by such evidence, assessment of family impact on dental diseases, craniofacial anomalies and treatment outcomes has become a research focus [24-26].
Another study reported that the negative impact of having children with cleft lip and palate was not influenced shortly after reconstructive surgery thus suggesting the importance of appropriate medical care coupled with special psychological support to improve quality of life of affected parents [25]. The negative impact was relatively low for financial burden compared to other dimensions except for the context of work loss for a limited number of mothers and accompanying fathers who were self-employed. Sri Lanka as a lower- middle-income-developing country provides free health care including oral health care in the public sector. This notion was supported by a study conducted in 6 cleft centres in USA involving a diverse sample of 1200 children with cleft lip and palate and their parents assessing 3 domains of family functioning namely: cohesion, expressiveness [26]. Sri Lankan socio-cultural context fosters a closely knit family structure which allows parents and children to share the life together till late. Parents and caregivers play a significant role on children’s oral health, within the context of the family level as described by the conceptual model of Fisher- Owen et al. [27]. It is the period of primary socialization in which dietary practices, oral hygiene practices and health behaviours are being established directly and indirectly influenced by knowledge, attitude and practices of parental care givers. Hence, parental care givers who are in a constant worry about appearance and status of teeth of their children affected by AI, adds an extra burden to them which may hinder parents inculcating behaviours among children that are conducive to good oral health. Moreover, Adar et al. has highlighted the influence of community level cultural factors that influence child’s oral health [28,29].
This notion was reflected in the feelings expressed by mothers as they perceived that children might feel pain when brushing teeth despite taking extra care. Furthermore, discoloured teeth of a child and its negative social impact was perceived by mothers as a feeling guilty and shameful for passing a bad disease to the child as well as other supernatural causes which in turn made the mothers to be anxious. Similar feelings were reported by other recent studies as well [17]. Present study has the strength of representing all ethnic groups in Sri Lanka. Moreover, it allowed for an in-depth appraisal of mother’s concerns on family impact of having a child affected by AI. The study setting was the only University Hospital with the department of pediatric dentistry for the whole country as the prime referral centre for children affected by rare craniofacial disorders. Moreover, one-to-one interview method prior to commencing treatment for the child which allowed mothers to better express their concerns and experiences on child’s tooth condition. The findings synthesized the evidence for high impact on families posed by having children with AI. Given sociocultural context of a country with norms, traditions and values influence the perceptions of mothers thus demonstrating a social patterning grounded to the extent of social production of anxiety and tension among affected mothers. Mothers also reported that they are overwhelmed by anxiety on future prospects of their affected children. The multi-faceted nature of the experiences shared by the respondents with some convergence/overlapping in sub-dimension constituents of dimensions such as Interrupted family activity and parental emotions highlights coherence of the constituents constructs of composite construct of family impact of having a child with AI. Nevertheless, further explorations should include unexplored dimensions of parental concerns of having a child affected with amelogenesis imperfecta such as arriving at the diagnosis.
If fathers of children with AI were included into the present exploration there could have been different versions of experiences and perceptions on family impact. However, as mothers are the predominant caregivers for their children and their families in Sri Lankan context, maternal concerns deserved priority.
AI significantly impact on quality of life of affected children, adolescents and young adults. Research supported this notion based on findings of a study conducted in Sweden as the adolescents and young adults with AI perceived significantly reduced OHRQOL compared to healthy controls. Importantly extensive dental treatment did not increase dental fear or negative attitudes towards dentistry. The same study found that definitive therapy with porcelain crowns at this age was able to significantly improve their OHRQOL. Hence, as emerged from the findings of the present study mothers’ concerns on quality of life of their children in the past, present and future contexts seem rational as the interviews were conducted prior to commencing definitive treatment for the AI status of children. Qualitative data on family functioning provides important information on health beliefs, specific conflicts and facilitators and inhibitors of family function and cohesion. Such information could be used to plan interventions to bolster competencies within protective factors to enhance resilience in negative circumstances [29].
In conclusion, present findings corroborated the findings of other qualitative explorations on parental perceptions and experience in having a child affected with AI. Across the borders of cultures and countries, commonalities in experiences and family impact while indicating some special concerns with regard to developing country socio-cultural perspective. Pediatric dentists should understand the need for providing psychosocial support for parents of children affected by AI and other oro-facial conditions by raising their awareness on the nature of given disease condition, treatment options available and the possibility of improving the quality-of-life children with optimal treatment will become vital in this regard. Family Impact Scale as a theoretical framework for family impact assessment of having children with AI in a developing country context was indicated by the findings. Explicit theoretical framework-based family impact assessment might enhance child and family- centered treatment outcomes in longstanding management of children with inherited developmental defects of teeth and craniofacial complex such as AI. Nevertheless, further research warranted to confirm the present findings.
References
- Milutinovic J, Zelic K, Nedelikovic N (2014) Evaluation of facial beauty using Anthropometric proportions. The Scientific World Journal 2014: 428250.
- Backman B, Holm AK (1986) Amelogenesis Imperfecta: prevalence and incidence in a Nothern Swedish County. Community Dent Oral Epidemiol 14: 43-44.
- Aldred MJ, Craford PJM, Savarirayan R (2003) AmelogenesisImperfecta- a classification and catalogue for the 21st century. Oral Diseas 9: 19-23.
- Pousette Lundgren G, Hasselblad T, Johansson AS, Johansson A, Dahllöf G (2019) Experiences of Being a Parent to a Child with Amelogenesis Imperfecta. Dent J (Basel) 7(1): 17.
- Gadhia K, McDonald S, Arkutu N, Malik K (2012) Amelogenesis imperfecta: an introduction. Br Dent J 212(8): 377-379.
- Herath EMUCK, Jayasooriya PR, Perera IR (2011) Descriptive analysis of Amelogenesis Imperfecta. Sri Lanka Journal 41(1,2): 17-25.
- Witkop CJ, Sauk JJ (1976) Heritable defects of enamel. In: Stewart R, Prescot G (ed.). Oral Facial Genetics. St Luis Mosby pp. 151-226.
- Alqadi A, O’Connell AC (2018) Parental perception of children affected by Amelogenesis Imperfecta (AI) and Dentinogenesis Imperfecta (DI) : a Qualitative Study. Dent J 6: 65.
- Marquazin MCS, Zanope BR, Pacteco LF, Gaviao MBD (2015) Case-Report: aesthetic and functional rehabilitation of the primary dention affected by amelogenesis imperfects. Case report in dentistry p. 6.
- Parekh S, Almehatab M, Cunninhham SJ (2014) How do children with amelogenesis imperfect feel about their teeth. International Journal of Paediatric Dentistry 24: 326-335.
- Sneller J, Buchhanan H, Parekh S (2014) The impact of amelogenesis imperfect and support needs of adolescents with AI and their parents: an exploratory study. International Journal of Paediatric dentistry 24(6): 409-416.
- Crawford PJ, Aldred M, Bloch-Zupan A (2007) Review. Amelogenesis Imperfecta. Orphanet Journal of Rare Diseases 2: 17.
- Coffield K, Phillips C, Brady M, Robert MW, Strauss R, et al. (2005) The Psychosocial impact of developmental dental defects in people with hereditary Amelogenesis Imperfecta. JADA 136(5): 620-630.
- Dogba MJ, Bedos C, Durigova M, Montpetit K, Wong T, et al. (2013) The impact of severe osteogenesis imperfecta on the lives of young patients and their parents—A qualitative analysis. BMC Pediatr 13: 153.
- Scheffel DLS, Jeremias F, Fragelli CMB, Santos-Pinto LAM, Hebling J, et al. (2014) Esthetic dental anomalies as motive for bullying in schoolchildren. European Journal of Dentistry 8(1): 124-128.
- Locker D, Jokovic A, Stephens M, Kenny D, Tompson B, et al. (2002) Family impact of child oral and oro-facial conditions. Commun Dent Oral Epidemiol 30: 438-448.
- Lundgren GP, Dahllöf G (2014) Outcome of restorative treatment in young patients with Amelogenesis imperfecta. a cross-sectional, retrospective study. J Dent 42: 1382–1389.
- Dashash M, Yeung CA, Jamous I, Blinkhorn A (2013) Interventions for the restorative care of amelogenesis imperfecta in children and adolescents. Cochrane Database Syst Rev (6): CD007157.
- Smith CEL, Poulter JA, Antanaviciute A, Kirkham J, Brookes SJ, et al. (2017) Amelogenesis Imperfecta; Genes, Proteins, and Pathways. Front Physiol 8: 435.
- Herath CK, Perera IR, Jayasooriya PR (2018) The socio-demographic profile of children affected by Amelogenesis imperfecta and its impact on their families: a pilot study based on patients attending a Paedodontic clinic in Sri Lanka. Journal of South Asian Association of Paediatric Dentistry 1(1): 5-8.
- Fink R (1989) Issues and problems in measuring children’s health status in community health research. Soc Sci Med 29: 715-719.
- Osman L, Silverman M (1996) Measuring quality of life for young children with asthma and their families. EurRespir J 9(suppl.) 35s-41s.
- Lundgren GP, Karsten A, Dahloff G (2015) Oral health related quality of life before and after crown therapy in young patients with amelogenesis imperfecta. Health and Quality of Life outcomes 13: 197.
- Barbadosa TS, Gaviao MBD (2009) Evaluation of the Family Impact Scale for use in Brazil. J Appl Oral Sci 17(5): 397-403.
- Macho P, Bohac M, Fedeles J Jr, Feikiacova D, Fedeles J Sr (2017) Impact of cleft lip and palate in children on family quality of life before and after reconstructive surgery. BratisL Lek Lisfy 11(6): 370-373.
- Crerand CE, Rosenberg J, Magee L, Stein MB, Wilson-Genderson M, et al. (2015) Parent-Reported Family Functioning Among Children With Cleft Lip/Palate. Cleft Palate Craniofac J 52(6): 651-659.
- Fisher-Owens S, Gansky S, Platt LJ, Weintraub JA, Soobader MJ, et al. (2007) Influences on children’s oral health: a conceptual model. Paediatrics 120: 510-520.
- Adair PM, Pine C, Burnside G, Nicoll AD, Gillet A, et al. (2004) Familial and cultural perceptions and beliefs of oral hygiene and dietary practices among ethnically and socio-economically diverse groups. Community Dental Health 21(Suppl): 102.
- Gomez R, McLaren S (2006) The association of avoidance coping style, and perceived mother and father support with anxiety/depression among late adolescents: applicability of resilience models. Personality and individual differences 40: 1165-1176.
Editorial Manager:
Email:
pediatricdentistry@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...