Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6636
Research Article(ISSN: 2637-6636) 
Evaluation of Pre-treatment with Low-speed Round Bur for Fractured Teeth Surfaces that are Left untreated after Traumatic Injuries Volume 8 - Issue 1
Yoshishige Yamada1*, Yuichi Kimura2, Mozammal Hosaain3 and Tatsuya Shibata4
- 1Division of Operative Dentistry, Department of Conservative Dentistry, Ohu University School of Dentistry, Japan
- 2Division of Endodontics, Department of Conservative Dentistry, Ohu University School of Dentistry, Japan
- 3Department of Conservative Dentistry and Endodontics, Bangabandhu Sheikh Mujib Medical University, Faculty of Dentistry, Dhaka, Bangladesh
- 4Division of Dental Pharmacology, Department of Oral Medical Science, Ohu University School of Dentistry, Japan
Received: May 19, 2023; Published: June 02, 2023
*Corresponding author: Yoshishige Yamada, Division of Operative Dentistry, Department of Conservative Dentistry, Ohu University School of Dentistry, 31-1 Misumido, Tomita-machi, Koriyama-city, Fukushima 963-8611, Japan
DOI: 10.32474/IPDOAJ.2023.08.000292
Abstract
It is not known whether cleaning with a bristle brush can completely remove debris from fractured surfaces in the case of fractured teeth are left untreated after traumatic injuries. Therefore, the present study investigated the necessity of pre-treatment with a low-speed round bur instead of cleaning with a bristle brush and compared the adhesive effect to tooth surfaces with several etching systems by microleakage test and scanning electron microscopic (SEM) observation. Both corners of the incisal edges of 60 extracted human permanent incisors were cut and applied organic debris artificially, then immersed in artificial saliva at 37°C for 7 days and divided into two groups: group A was treated with bristle brush and group B was treated by a stainless round bur. The specimens in each group were divided into five subgroups (subgroup 1: total-etching system, subgroups 2 and 3: two-step self-etching system, subgroups 4 and 5: one-step self-etching system). The tooth surface was then restored with composite resin. The teeth in each fractured area were evaluated leakage condition and gap formation by microleakage test and SEM observation. As a results, specimens in group A showed the presence of residual organic debris and microleakage in some cases and this group showed significantly more gap formation than group B. There were no significant differences between each subgroup in group A and group B respectively. In conclusion, removal of debris by a low-speed round bur along the fractured surfaces would be required in this case of a few days after injury.
Keywords: traumatic injury; residual organic debris; microleakage test; gap formation
Introduction
Although loss of the crown structure is mainly caused by caries, dental trauma is not a rare contributing factor. Researchers reported that the most commonly traumatized teeth were the maxillary central incisors [1-3] and the most frequent type of injury was crown fracture, especially enamel-only fracture and enamel– dentin fracture without pulp involvement (no pulp exposure) [1-7]. These fractures are usually restored with composite resin due to esthetic considerations. The success of composite resin restoration is strongly dependent on the bonding force between tooth surface and composite resin. The adhesive effects are influenced by the surface condition; therefore, cleaning the fractured surface is one of the most important steps determining success of the composite resin restoration. Usually, patients visit the dentist immediately after dental trauma. However, some patients do not seek treatment soon after injury and the injured tooth is left untreated for a few days to months. Ekanayake & Perera reported that half of the patients who had traumatized teeth had been treated more than 1 month after the traumatic injury [8]. Zuhal et al. also reported that only 22.8% of patients visited a dental clinic in the first 3 days [9] and Rajab revealed that only 17.1% of patients sought treatment the same day or the day after the injury [3]. Most of these cases were simple crown fractures without pain.
The surfaces of fractured teeth can become contaminated by plaque and organic debris during the untreated period, and they are usually cleaned by a bristle brush with prophylaxis paste before restoration. However, it is not known whether cleaning with a bristle brush adequately removes debris from fractured surfaces before restoration. There is a possibility that cleaning using a bristle brush and prophylaxis paste is not sufficient to remove debris, and that pre-treatment with rotary burs before composite resin restoration is necessary to remove enamel and dentin contaminated by plaque and organic debris.
The aims of this study were to clarify the influence of pretreatment with bristle brush and low-speed hand round bur of fractured surfaces before restoration on the adhesiveness of the material, and to compare the adhesive effect of different adhesive systems, such as a total-etching system, a one-step self-etching system and a two-step self-etching system, by microleakage test and scanning electron microscopic (SEM) observation.
Materials and Methods
Sample collected and artificial crown fracture preparation
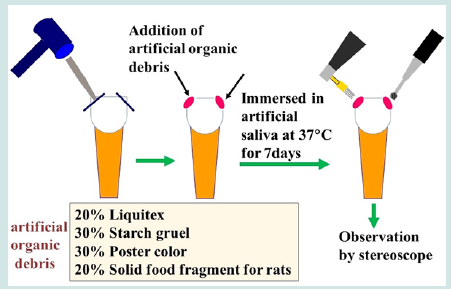
Sixty extracted human permanent incisors with intact crown surfaces were used in this study. The teeth were extracted for orthodontic and periodontal reasons after obtaining informed consent from patients. The teeth were brushed and washed with distilled water at room temperature. Both corners of the incisal edge of the central incisors were cut by dental mallet and Chisel (diameter, 3 mm) as shown in Figure 1 to represent an artificial traumatic crown fracture, and artificial organic debris was applied to each fractured surface. Artificial organic debris was prepared according to a previous report [10]. It contained 20% of Liquitex (Liquitex Co.OH, USA), 30% of Starch gruel (Fueki-ko, Fueki Co., Yao, Japan), 30% of Poster color (Sakura Co., Osaka, Japan), and 20% of solid food fragments for rats (MR-stock, Nihon-Nosan Co., Yokohama, Japan) normally used as animal feed. All ingredients were mixed together to simulate a clinical debris condition. After applying artificial organic debris to the surfaces, all specimens were immersed in artificial saliva (Salivate, Teijin, Tokyo, Japan) at 37°C for 7 days.
Group classification, and experimental procedures for fractured surface
After storage for 7 days, each fractured surface was washed with distilled water to remove the excess debris on the surrounding surface, and the following procedure was performed. In group A, the right-side crown-fractured surfaces were cleaned with a dry pointed bristle brush (Merssage brush CA, YDM Co, Tokyo, Japan) and prophylaxis toothpaste (Profylaxpasta CCS, Clean Chemical Sweden A.B., Borlänge, Sweden) using a low-speed hand piece (550 cycles per minute), but this process was stopped in 5 minutes even if debris remained on the surfaces. In group B, the left-side fractured surfaces were pre-treated with #2 stainless steel round burs using a low-speed hand piece (550 cycles per minute). This process continued until the debris was removed from the surfaces. After this procedure, all surfaces were rinsed with water, dried with oil-free compressed air for 20 seconds, and subjected to the following investigations.
Stereoscope observation and microleakage test
To verify the surface characteristics, fractured surfaces from each group were examined using a stereoscope (SMZ-10, Nikon, Tokyo, Japan), and then all surfaces in each group were subjected to a microleakage test.
The specimen teeth were randomly divided into five subgroups (12 teeth each) based on the adhesive system. In subgroup 1, a total etching system was used. The surfaces were acid-etched with 30% phosphoric acid gel (Clearfil K-etchant, Kuraray Co., Kurashiki, Japan) using a disposable microbrush for 20 seconds. Thereafter, they were washed with water spray for 10 seconds, thoroughly dried with oil-free compressed air. They were then treated with bonding agent (Clearfil Photo Bond, Kuraray Co.) with light-cured for 10 seconds each. and filled with composite resin (Beautyfil II, Shofu Inc., Kyoto, Japan). After the fractured surface was restored with composite resin, it was light-cured for 20 seconds. A twostep self-etching system was used for subgroups 2 and 3. The surfaces were washed and air-dried as in subgroup 1, treated with priming agent for 10 seconds, and thoroughly dried with oil-free compressed air for 5 seconds. Then, a bonding agent was applied (subgroup 2: Clearfil Mega bond FA, Kuraray Co.), (subgroup 3: FLBOND II Shofu Inc.), light-cured for 5 s and restored with composite resin (Beauty Fill II, Shofu Inc.).
One-step bonding system was used for subgroups 4 and 5. The fractured surfaces were treated with a priming agent (subgroup 4: Clearfil Tri-S Bond, Kuraray Co.), (subgroup 5: Bond Force Tokuyama, Hyogo, Japan) for 10 seconds, gently air-dried for 5 seconds and strongly air-dried for another 5 seconds. Then, the tooth was restored with composite resin according to the same procedure of the previous two systems. Microleakage test was performed according to a previous study [10]. All tooth surfaces except the areas of the filled fractured surfaces and 1 mm outside the margins of the cavities were double-coated with nail varnish. The samples were performed thermal cycling for 10,000 cycles between 5°C (± 2) and 55°C (± 2) with a 1- minute dwell time in each temperature and immersed for 24 hours in a rhodamine-buffered dye solution. The samples were longitudinally bisected with a diamond saw disc (Isomet, Buehler, IL, USA). The degree of microleakage was scored in a blinded manner using dye penetration, based on a modification of a previously reported 3 grade-scale criteria (Table 1), under a microscope by a technician who was not informed of the true nature and purpose of this experiment. Thus, judgment of the degree of microleakage was blinded. Where scores were different on both sides, the worse (higher degree of leakage) score was adopted for this research.
SEM observation for evaluating gap formation
For observation of the enamel/dentine-composite resin interface and investigation of the ratio of gap formation between them, cut sections were polished to a high gloss with waterproof carbide paper of 400 to 2,000 grits, immersed in 40% phosphoric acid gel for 15 minutes, and then observed by SEM. For SEM examination, specimens were dehydrated in a graded series of aqueous ethanol (70%, 80%, 90%, and 100% ethanol) for 24 hours in each solution, dried with liquid CO2 using a critical point dryer device (JCPD- 3, JEOL, Tokyo, Japan), coated with platinum to a thickness of 15 μm, and observed by SEM (JSM-T220A, JEOL) at 15 kV. The gap formation was scored as shown in Table 2. After all results were obtained, statistical analysis of the data was performed using a Mann Whitney U test and Kruskal-Wallis ANOVA. A value of p < 0.05 was considered significant.
Results
Figure 2: Surface condition after debris removal Figures 2 (A, B): Group A (bristle brush and a prophylaxis paste cleaning group). Residual debris was seen in some cases on the fractured surface. Residual debris was most frequently observed at dentino enamel junction (arrows show remaining debris). Figure 2(C, D): group B (rotary bur-pretreated group). Debris was completely removed from the fractured surface.
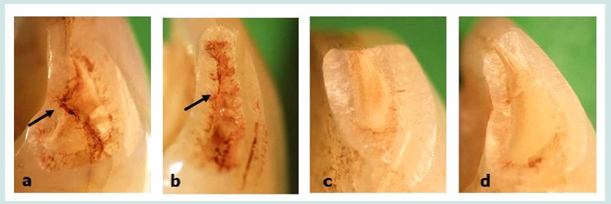
The surface condition in group B showed no residual organic debris. Fractured surfaces also did not exhibit any remarkable problems such as cracks or fractures. On the other hand, residual organic debris was seen in some cases of group A (Figure 2). The percentage of residual debris was 67%; the residual organic debris was most frequently seen at the border of the dentin-enamel junction (47%). However, there were no fractures and cracks of the tooth surfaces in group A.
Results of microleakage test
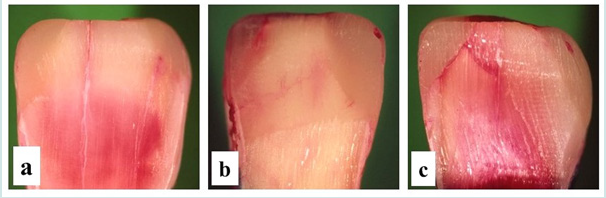
The leakage score values are presented in Table 1. A few cases in both groups did not show any leakage (Figure 3a). However, some degree of microleakage was observed in many cases, especially in group A (Figures 3B & 3C). The ratio of leakage was 43% (score 1 and 2) in the rotary brush group, and 23% (score 1 and 2) in the round bur cleaning group. Although the difference between group A and B in each etching system was not statistically significant, the tendency of leakage was higher with bristle brush cleaning than round bur pretreatment. When compared within each etching system (subgroups 1-5), there were no statistical differences among etching systems in groups A and B. The summary of the results of microleakage test is shown in Table 3.
Figure 3: Results of leakage condition (stereoscopic observation). A few cases in both groups did not show any leakage (Figure 3a). Some degree of microleakage was observed in many cases, especially in group A (Figures 3b, 3c).
Results of gap formation
From SEM observation, the sites with no microleakage showed good adhesion at the enamel/dentine and composite resin interface. Sites where resin tags penetrated into the tooth surface were also observed (Figures 4A & 4B). In contrast, gap formation at the composite-dentin interface was observed at several areas on the specimen in each etching system (Figures 4C & 4D). The tendency of gap formation was obviously higher in group A than in group B, and statistical differences were seen between the two groups in each etching system. However, comparing each subgroup, statistically significant differences were not recognized among each etching system in groups A and B, respectively. The summary of the result of gap formation is indicated in Table 4.
Figure 4: SEM observation of tooth material-resin composite interface Figure 4(A, B): no gap formation. Immersed resin tags were observed in adhesive tooth materials. Figure 4(C, D): gap formation. Gap formation was observed in many cases in group B (arrow shows the location of gap formation).

Discussion
Many researchers reported that the highest frequency of tooth injury occurs in school children aged around 6 to 12 years old [3,11,12]. However, adults are also vulnerable to tooth damage by several types of traumatic injuries. Many cases of such injuries resulting in tooth fractures are repaired by restorative materials. However, re-restoration is sometimes necessary because of loss of the restorative material, residual debris or development of new caries from the margin of the restorative material–tooth interface. The result of the present study also indicated that residual debris is commonly seen on the fractured surfaces cleaned by a bristle brush, especially at the marginal area of the dentin-enamel junction. Organic debris such as food particles easily accumulate at the dentin-enamel junction, and it is difficult to remove debris from this site. Previous studies demonstrated that carious dentine and several bacteria are also hard to remove completely, and they partially remain at the dentin-enamel junction [13-15]. Moreover, dental plaque looks similar to the dentin in color, and it is possible to mistake residual debris as tooth dentin after cleaning with a bristle brush.
To resolve this serious problem, it is therefore strongly proposed to use a round bur on a low-speed hand piece to remove the thin surface layer of organic debris and expose the healthy tooth surfaces. In the case of untreated fractured crown surfaces, a round bur with a low-speed hand piece should be used before restoring with composite resin. Otherwise, organic debris will not be removed completely; consequently, the surface layer of the specimen will be infected by bacteria. This is also supported by some of the previous studies that when debris or smear layer are present on the surface, resin tags are not able to penetrate into enamel or dentin, consequently causing the interface to be more sensitive to degradation [16,17]. The adaptation between composite resin and dentin seems to improve by removing the smear layer from intertubular dentin [18].Therefore, achievement of tight adhesion between composite resin and dentine surfaces is a necessary element to establish good adhesion, and removing the smear layer on the fractured surfaces is one of most important factors to achieve stable bond strength.
The results of microleakage test also revealed that cleaning with bristle brush treatment showed more leakage and gap formation than the groups with round bur treatment. This indicates that cleaning by bristle brush and prophylaxis paste might not be adequate as pre-treatment before composite resin restoration. This is also supported by some of the previous studies that it is hard to remove debris and plaque completely by cleaning with a bristle brush. Furthermore, several researchers also demonstrated that even saliva contamination reduced adhesion [19,20]. Wang & Spencer reported that the acid etching process was not able to remove debris and the smear layer completely, resulting in remaining denatured collagen within the smear layers [21]. Consequently, thorough cleaning of the tooth surfaces is essential for composite resin bonding. These findings indicated that stain and debris on the tooth surfaces are not easy to remove using ordinary methods. Using of low-speed round bur could be an alternative method to bristle brush. The results of the present study also showed that there was no statistically significant difference among each etching system. This result indicated that the adhesive strength between tooth and composite resin might not be influenced by differences among the adhesive systems. Even though the total-etching system (Photo Bond) showed high tendency of microleakage and gap formation in both bristle brush-treated and round bur-treated groups, statistical significance was not revealed in this study and these results were in agreement with previous studies [22,23].
However, this study evaluated the specimen after 10,000 thermal cycles; therefore, it is possible that different results of microleakage test and gap formation in each adhesive system would be obtained when the specimen is subjected to over 10,000 cycles. Further studies using 20,000 or 30,000 cycles are necessary. In clinics, bevel creation along the marginal area of fractured tooth is often performed in anticipation of increasing adhesive effect [24- 26]. However, this additional option is not effective if there is any barrier to prevent bonding to teeth and will result in problems such as recurrent caries under composite resin restoration, fracture of composite resin or detachment of resin from teeth. The results of this study indicate that performing pre-treatment with a low-speed round bur removes residual debris and infected bacteria. Moreover, SEM observation demonstrated that round bur treatment may not cause serious problems such as cracks or fractures during this process and is a safe method to be applied on fractured teeth surfaces. Therefore, this process could improve the adhesive effect of composite resin yielding satisfactory results in the case of fractured tooth left untreated for a few days or more.
Conflicts of Interest
There are no conflicts of interest.
References
- Oliveira LB, Marcenes W, Ardenghi TM, Sheiham A, Bönecker M (2007) Traumatic dental injuries and associated factors among Brazilian preschool children. Dent Traumatol 23(2): 76-81.
- Sandalli N, Cildir S, Guler N (2005) Clinical investigation of traumatic injuries in Yeditepe University, Turkey during the last 3 years. Dent Traumatol 21(4): 188-194.
- Rajab LD (2003) Traumatic dental injuries in children presenting for treatment at the Department of Pediatric Dentistry, Faculty of Dentistry, University of Jordan, 1997-2000. Dent Traumatol 19(1): 6-11.
- Belcheva AB, Indzhova KN, Manolova MS, Stefanov RS, Mileva SP (2008) Prevalence of crown fractures of permanent incisors in schoolchildren aged 7-11 years from Plovdiv. Folia Med (Plovdiv) 50(2): 43-49.
- Segura JJ, Poyato M (2003) Tooth crown fractures in 3-year-old Andalusian children. J Dent Child (Chic) 70(1): 55-57.
- Goenka P, Marwah N, Dutta S (2010) Biological approach for management of anterior tooth trauma: Triple case report. J Indian Soc Pedod Prev Dent 28(3): 223-229.
- Locker D (2005) Prevalence of Traumatic Dental Injury in Grade 8 Children in Six Ontario Communities. Can J Public Health 96(1): 73-76.
- Ekanayake L, Perera M (2008) Pattern of traumatic dental injuries in children attending the university dental hospital, Sri Lanka. Dent Traumatol 24(4): 471-474.
- Zuhal K, Semra OE, Hüseyin K (2005) Traumatic injuries of the permanent incisors in children in south Turkey: a retrospective study. Dent Traumatol 21(1):20-25.
- Yamada Y, Hossain M, Shimizu Y, Kimura Y, Masuda Y, et al. (2008) Analysis of surface roughness and microleakage of fissure sealants following organic debris removal with Carisolv. J Dent 36(2):130-137.
- Al-Majed I, Murray JJ, Maguire A (2001) Prevalence of dental trauma in 5-6 and 12-14 year-old boys in Riyah, Saudi Arabia. Dent Traumatol 17(4): 153-158.
- Vanka A, Ravi KS, Roshan NM, Shashikiran ND (2010) Analysis of Reporting Pattern in Children Aged 7 to 14 Years with Traumatic Injuries to Permanent Teeth. Int J Clin Pediatric Dent 3(1): 15-19.
- Bönecker M, Grossman E, Cleaton-Jones PE, Parak R (2003) Clinical, histological and microbiological study of hand-excavated carious dentin in extracted permanent teeth. SADJ 58(7): 273-278.
- Frencken JE, Leal SC (2010) The correct use of the ART approach. J Appl Oral Sci 18(1): 1-4.
- Cheng L, Zhang K, Weir MD, Liu H, Zhou X, Xu HH (2013) Effects of antibacterial primers with quaternary ammonium and nano-silver on Streptococcus mutans impregnated in human dentin blocks. Dent Mater 29(4): 462-472.
- De Munck J, Van Meerbeek B, Satoshi I, Vargas M, Yoshida Y, et al. (2003) Microtensile bond strengths of one-and two-step self-etch adhesives to bur-cut enamel and dentin. Am J Dent 16(6): 414-420.
- Combe EC, Owen BA, Hodges JS (2004) A protocol for determining the surface free energy of dental materials. Dent Mater 20(3): 262-268.
- Saraç D, Bulucu B, Saraç YS, Kulunk S (2008) The effect of dentin-cleaning agents on resin cement bond strength to dentin. J Am Dent Assoc 139(6): 751-758.
- Neelagiri K, Kundabala M, Shashi RA, Thomas MS, Parolia A (2010) Effects of saliva contamination and decontamination process on shear bond strength of self-etch dentine bonding system in vitro study. Journal of Conserv Dent 13(2): 71-75.
- Eiriksson SO, Pereira PN, Swift Jr EJ, Heymann HO, Sigurdsson A (2004) Effects of saliva contamination on resin-resin bond strength. Dent Mater 20(1): 37-44.
- Wang Y, Spencer P (2002) Analysis of acid-treated dentin smear debris and smear layers using confocal roman microscopy. J Biomed Mater Res 60(2):300-308.
- Deliperi S, Bardwell DN, Wegley C (2007) Restoration interface microleakage using one total-etching and self-etch adhesives. Oper Dent 32(2): 179-184.
- Owens BM, Johnson WW, Harris EF (2006) Marginal permeability of self-etch and total-etch adhesive systems. Oper Dent 31(1): 60-67.
- Coelho de-Souza FH, Klein Júnior CA, Camargo JC, Beskow T, Balestrin MD, et al. (2010) Double-blind randomized clinical trial of posterior composite restrations with or without bevel: 6-month follow-up. J Contemp Dent Pract 11(2):1-8.
- Swanson TK, Feigal RJ, Tantbirojn D, Hodges JS (2008) Effect of adhesive systems and bevel on enamel margin integrity in primary and permanent teeth. Pediatr Dent 30(2):134-140.
- Coelho de-Souza FH, Camacho GB, Demarco FF, Powers JM (2008) Fracture resistance and gap formation of MOD restorations: influence of restorative technique, bevel preparation and water storage. Oper Dent 33(1): 37-43.
Editorial Manager:
Email:
pediatricdentistry@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...