Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6636
Research Article(ISSN: 2637-6636) 
Embryonal Rhabdomyosarcoma of the Soft Palate in a Young Adult Volume 7 - Issue 5
Georgakopoulou EA1, Laskaris G2, Kittas C3 and Stoufi E4*
- 1Molecular Carcinogenesis Group, Department of Histology and Embryology, Medical School, National and Kapodistrian University of Athens, Greece
- 2Private Oral Medicine Practice 37 Ipsilantou, Athens, Greece
- 3Medical School, National and Kapodistrian University of Athens, Greece
- 4Athens Euroclinic7-9 Athanasiadou & D Soutsou Streets, Greece
Received: June 17, 2022; Published: June 28, 2022
*Corresponding author: Stoufi E, Athens Euroclinic7-9 Athanasiadou & D Soutsou Streets, Greece
DOI: 10.32474/IPDOAJ.2022.07.000274
Abstract
This is a very rare case report describing a 22-year-old male patient with a soft palate embryonic rhabdomyosarcoma stage 1. Rhabdomyosarcoma is a childhood tissue sarcoma that is believed to be derived from primitive mesenchymal cells and can be found in a number of organs and tissues, with very few cases involving the oral cavity. To add to the current status of knowledge we report this patient
Introduction
Embryonal rhabdomyosarcoma is a very rare tumor with only a few cases reported in the oral cavity [1]. Rhabdomyosarcomas are malignant skeletal muscle neoplasms that derive from embryonic mesenchyma [2]. Embyonal is the most common histological subtype of rhabdomyosarcoma, while the other subtypes are Botryoid, Alveolar and Pleomorphic [3]. This is usually a pediatric malignancy, with few rare descriptions of adolescent and young adult patients. The clinical characteristics are that of an irregularly shaped ulcerated mass and are non-specific. Histology reveals a small, round, undifferentiated cell population with basophilic cytoplasm, a pattern similar to a group of round cell tumors [4]. Accurate diagnosis and classification of tumors is not possible solely on the basis of histological characteristics but requires further laboratory investigations: immunohistochemistry, electron microscopy, cytogenetic analysis, and molecular biology [5,6]. Early diagnosis and disease-specific treatment may have a profound impact on prognosis, a tertiary center study in pediatric patients recorded a high 5-year survival rate(5-year failure-free survival rate of 90%) in patients with embryonic rhabdomyosarcoma stage 1) [7]. Certain reports in head and neck patients showed a significant difference in prognosis when the disease was diagnosed at an early stage without metastatic progression of [8,9]. This case describes a young male post adolescent patient (22 years of age) with a soft palate developmental rhabdomyosarcoma stage 1.
Case Study
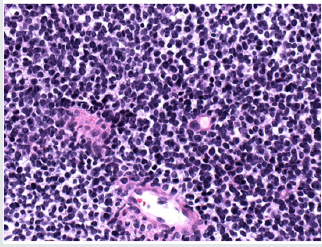
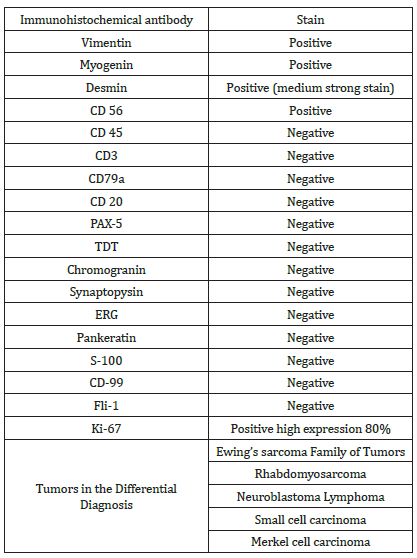
Young male patient complained about soft palate growth. The oral examination showed a non-tender ulcerated mass with an irregular shape and a size of less than 2 cm on the midline of the soft palate (Figure 1). The medical and social history of the patient were unremarkable. A few weeks before the appointment, the palatal lesion was felt by the patient. Based on the clinical features, the working diagnosis was a soft tissue oral malignancy, and a biopsy was scheduled. Histology was consistent with small round cell tumor and a large number of immunohistochemistry stains were scheduled for final diagnosis (Table 1 & Figure 2). Depending on the positivity of Myogenin and Vimentin, the final diagnosis was soft palate embryonic rhabdomyosarcoma. Additional imaging analysis did not reveal any other locations of involvement. The treatment plan consisted of a combination of ifosfamide, vincristine and actinomycin chemotherapy together with 28 radiotherapies (total 5040cGy). The patient had a complete remission of the disease, and no surgery was scheduled. The patient is disease-free one year after initial diagnosis (Figure 3).
Discussion
Rhabdomyosarcoma is a very rare and highly aggressive malignancy that usually affects children and rarely young adolescents [10]. The prognosis is largely dependent on the stage of the tumor. Diagnosis is a challenge. The clinical signs are nonspecific. Histological image is common in a number of malignant tumors grouped together as “small round (blue) cell tumors,” but each has a completely different prognosis and requires a different therapeutic strategy (Table 1). Accurate diagnosis is largely dependent on immunobiological biomarkers. Rhabdomyosarcomas express Myogenin and MyoD1, which are myogenic transcriptional regulatory proteins identified during skeletal muscle differentiation 1. Early and accurate diagnosis is important as it may make the disease manageable. In a pediatric stage 1 group of patients 7, favorable prognosis was observed. There are only limited case reports in adolescent and postadolescent patients and reported variable treatment strategies cannot support accurate prognosis. Treatment includes traditional surgery, chemotherapy (actinomycin D, doxorubicin, ifosfamide, cyclophosphamide, etoposide, or vincristine) and radiotherapy [11]. Our patient was treated with a mixture of chemotherapy and radiotherapy that fully controlled the disease. So far, he has performed excellently. Treatment sequlae, especially in children, are numerous, including dental abnormalities, hypoplastic jaw bones, trism and hyposalivation / xerostomia, and can have a serious impact on patient quality of life [11].
Conclusion
This very rare case shows the need for a thorough investigation of any abnormal growth of soft tissue in the oral cavity. The best screening method for all types of oral malignancies remains the meticulous oral and extraoral clinical examination during dental visits and the prompt referral of any abnormalities observed.
References
- Datta S, Ray JG, Deb T, Patsa S (2016) Embryonal rhabdomyosarcoma: A rare oral tumor. Journal of oral and maxillofacial pathology : JOMFP 20(3): 527-531.
- Chigurupati R, Alfatooni A, Myall RW, Hawkins D, Oda D (2002) Orofacial rhabdomyosarcoma in neonates and young children: a review of literature and management of four cases. Oral oncology 38(5): 508-515.
- Astekar M, Metgud R, Sharma P, Ramesh G (2012) Oral alveolar rhabdomyosarcoma: a case report with immunohistochemical analysis. Clinics and practice 2(1): e17-e17.
- Sharma S, Kamala R, Nair D (2017) Round Cell Tumors: Classification and Immunohistochemistry. Indian journal of medical and paediatric oncology : official journal of Indian Society of Medical & Paediatric Oncology 38(3): 349-353.
- Gordon Nunez MA, Piva MR, Dos Anjos ED, Freitas RA (2008) Orofacial rhabdomyosarcoma: report of a case and review of the literature. Medicina oral, patologia oral y cirugia buccal 13(12): 765-769.
- Morotti RA, Nicol KK, Parham DM (2006) An immunohistochemical algorithm to facilitate diagnosis and subtyping of rhabdomyosarcoma: the Children's Oncology Group experience. The American journal of surgical pathology 30(8): 962-968.
- Meza JL, Anderson J, Pappo AS, Meyer WH (2006) Analysis of prognostic factors in patients with nonmetastatic rhabdomyosarcoma treated on intergroup rhabdomyosarcoma studies III and IV: the Children's Oncology Group. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 24(24): 3844-3851.
- Pontes FS, de Oliveira JI, de Souza LL (2018) Clinicopathological analysis of head and neck rhabdomyosarcoma: A series of 10 cases and literature review. Medicina oral, patologia oral y cirugia buccal 23(2): e188-e197.
- Turner JH, Richmon JD (2011) Head and neck rhabdomyosarcoma: a critical analysis of population-based incidence and survival data. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery 145(6): 967-973.
- Gurria JP, Dasgupta R (2018) Rhabdomyosarcoma and Extraosseous Ewing Sarcoma. Children, Basel, Switzerland 5(12).
- Smith MH, Atherton D, Reith JD, Islam NM, Bhattacharyya I, et al. (2017) Rhabdomyosarcoma, Spindle Cell/Sclerosing Variant: A Clinical and Histopathological Examination of this Rare Variant with Three New Cases from the Oral Cavity. Head and neck pathology 11(4): 494-500.
Editorial Manager:
Email:
pediatricdentistry@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...