Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6636
Research Article(ISSN: 2637-6636) 
A Study on the Coronavirus-19 Response of Implant Patients and Dental Workers Volume 6 - Issue 5
Sujunpan* and Hee Ja Na
Department of Dental Hygiene, Honam University, Korea
Received:September 29, 2021; Published: October 13, 2021
*Corresponding author: Sujunpan, Department of Dental Hygiene, Honam University, Korea
DOI: 10.32474/IPDOAJ.2021.06.000250
Abstract
Objective: The Dental clinic studies Infection control and Differences in Hygiene Management in Dental Manager to provide data based on safe Dental clinic by enhancing the Prevention of Infectious Diseases in Immigration and Dental Manager.
Methods: The study was conducted in January 2021 by 30 implant patients and 30 permanent workers who were receiving post-implant care in the G city area. The Implant patient’s coronavirus–19 prevention questionnaire includes age, gender, scaling after implant implantation, 1mm Loss of Limbic bone, wearing a mask, body temperature measurement, and disinfectant. Fourteen questions for Dental workers under management include scaling after implantation, Dental cartilage Loss 1MM, Dental hygiene age, mask repetition, indoor ventilation, disinfectant hand washing, paper towel use, medical gloves, gloves disposal, kf94 mask, mask disposal, eye protection, and disposal.
Results: In a simple regression analysis, the independent variable that significantly affects the wearing of kf94 masks at a significant Level of .05 is the age of Dental hygiene (t=-2.259, p=).It was significantly shown as 033). However, wearing a mask repeatedly (t=-).626, p=.537), Ventilation(t=-1.697, p=.102.), Wash hands with disinfectant (t=).264, p=.There is no significant difference in 794.
Conclusion: The new study is very significant, and we conducted a new perspective to check closely with Dental managers to see if there is thorough prevention of infectious diseases in order to prevent cross-infection from implant patients to Dental managers in COVID-19 situations
Keywords:Inverted mesiodens; palatal impaction; supernumerary
Introduction
Dental Clinic contains not Only Blood and Saliva, but also blood and saliva. in aerosol exposed environment to droplet spreader Infection Adequately adhering to the Infection control principle to block the transmission of the contagious Coronavirus-19 is very important to protect Patients and Dentists. Centers for Disease control and Prevention’s Coronavirus Infectious Diseases-19 Response Guidelines [1]. The study was based on guidelines for Behavior in Patient Care, Dental workforce management, and infection control in Dental installations in response to coronavirus infections-19. First of all, hand hygiene is Before and after patient contact and implemented. It shall be conducted in all cases where the patient’s blood, bodily fluids, secretions, excrements, or other pollutants have been contacted or exposed to the patient’s surroundings. If contaminated, disinfect it with water and soap, and if not, alcohol hand sanitizer may be used. Hand hygiene is performed for 40-60 seconds with water and soap, and 20-30 seconds with alcohol hand sanitizer. Personal protective equipment shall then be worn to select appropriate personal protective equipment according to medical treatment, procedures, and activities. When using personal protective equipment, the proper means of wearing and taking off shall be observed. After removing personal protective equipment, it should be properly collected so that outsiders are not exposed. If there is a possibility of contact with objects contaminated with blood or body fluids, mucous membranes, damaged skin, or contaminated skin, wear gloves and use them for single use. When wearing gloves, take them off immediately after use, and replace them for each patient.
Perform hand hygiene immediately after removing gloves. If contact with blood, bodily fluids, secretions, or effluents is expected, wear a gown suitable for the work to protect the skin and prevent contamination of the clothes. When clothes are at risk of exposure to blood, body fluids, secretions, or effluents in treating patients, disposable plastic aprons are worn, and Long-sleeved waterproof gowns are worn if they can be widely splashed. Hand hygiene is performed without gowns before Leaving the patient’s surroundings or hospital rooms. Disposable aprons or gowns are changed for each procedure or patient. In addition, treatment equipment and equipment shall be disinfected and used in accordance with the manufacturer’s recommendation guidelines using certified disinfectants from the Licensed agency after use. Use disposable equipment or items if possible. Treatment devices for patients contaminated with blood, bodily fluids, secretions, and excrement treat skin or mucosal exposure and contamination of clothing or the spread of pathogens to other patients and the environment. Reuse equipment shall be properly cleaned and disinfected and used in other patients, and reprocessing methods shall be in accordance with the type of equipment, the manufacturer’s recommendation, hospital guidelines or regulations, and disposable items shall be discarded after use. Equipment cleaning staff shall wear personal protective equipment when washing. Check the disinfectant manufacturer’s recommendations to ensure thorough compliance with the recommended criteria, such as disinfectant dilution and application time, disinfectant validity period and effective concentration [2].
Employees in charge of cleaning or disinfection in cleaning and environmental management shall receive education on infection prevention (use of protective equipment, cleaning methods, etc). Wear appropriate personal protective gear for cleaning or disinfection. Wear personal protective gear (waterproof gloves, health KF94 mask, disposable waterproof long-sleeved go, waterproof apron, boots, goggles, etc.) in accordance with the guidelines. If the surface of the environment is contaminated with blood or secretions, remove the contaminants first and clean them. Wipe with a mop dampened with cleaning solution or Disinfectant rather than using a broom or vacuum cleaner. Without spraying disinfectant, wet the Disinfectant on a clean towel or thoroughly wipe the environmental surface with a commercialized disinfectant tissue. Cleaning tools are used as disposable or exclusively as possible. Provided, that where cleaning tools are reused, the used cleaning tools shall be disinfected using a suitable Disinfection, dried, and stored. Disinfectant is a Disinfectant commonly used by medical institutions that recommends Hypo-chlorous acid sodium chlorate (1,000 ppm] On disinfection Personal protective gear (waterproof gloves, health KF94 mask, disposable waterproof long-sleeved go, waterproof apron, boots, goggles, etc.) may be worn and 70% alcohol may be used on local surfaces. When using disinfectants, recommendations such as dilution magnification, contact time, handling precautions, etc. suggested by the manufacturer shall be followed [3-5].
Environmental surfaces contaminated with blood, bodily fluids, secretions, and excrement are immediately decontaminated and disinfected. After a doctor’s patient visits in the case of coronavirus-19, environmental management thoroughly disinfects all environmental surfaces, including door handles, waiting chairs, reception counters, and clinic chairs, along the patient’s path. Disinfection uses a 50-foLd dilution chlorine-based disinfectant (1,000 ppm effective chlorine concentration) [6,7]. Waste disposal shall be in accordance with the Medical Waste Disposal Regulations. Waste shall be disposed of separately from the place where it is generated for proper and safe handling. Sharp tools, such as needles and blades, are collected in non-piercing waste containers, and containers should be placed where the goods are used. Collect solid, non-sharp infectious waste in a non-Leaking waste container and keep the Lid closed. A 1982 U. S. A Dental worker test for the infection virus reported 13% of Dental assistants, 17% of Dental hygienists, 14% of Dental engineers, and 24% of dentists [8]. Therefore, this study aims to study differences in infection management, patient management, patient hygiene management Level, and Dental manager’s hygiene management in the Dental clinic to increase the prevention of infectious diseases in the Dental clinic.
Materials and Methods
Objects of the study
In January 2021, this study conducted a hospital infection management survey of 30 patients undergoing post-implant care at Y Dental Clinic and 30 female Dental workers working at Y Dental Clinic and continuing care in G City. He/she visited the dentist in person, explained the purpose of the study and how to fill out the questionnaire, and retrieved it after filling it out. It was measured on the Likert 5-point scale with total infection control questions. The IRB (1041223-20211-HR-24) of this study was approved by Honam University’s Bioethics Research Committee.
Experimental method
The questionnaire for this study utilizes ‘Prevention of Cross- Infection in the Dental System’ [9]. The Covid-19 prevention survey for implant patients was 7 questions, and the Dental worker’s Covid-19 prevention practice was 14 questions, measured on the Likert 5-point scale. On the likert 5-point scale, 5 points are given to “very important”, and 1 point is given to “not important at all,” meaning that the higher the score, the higher the practice. There are seven questions about the corona prevention of implant patients, including age, gender, scaling after implantation, 1mm Loss of marginal bone, wearing a mask, body temperature measurement, and use of disinfectants. Fourteen questions for Dental workers under management include scaling after implantation, Dental cartilage Loss 1MM, Dental hygiene age, mask repetition, indoor ventilation, disinfectant handwashing, paper towel use, medical gloves, gloves disposal, KF 94 mask, mask disposal, eye protection, and disposal.
Data analysis
The SPSS 18.0 program was used for the collected data, which uses descriptive statistical analysis and practices prevention of Covid-19 in implant patients. Both the mean and standard deviation were obtained to determine the degree of practice and the response of Dental workers to infection control. In addition, the age of Dental hygienists and the sample t-test for preventive practice were conducted, and correlation analysis such as using paper towels and wearing kf94 was conducted. We then perform a regression analysis of wearing kf94 masks at a significance Level of .05 in a simple regression analysis.
Results
Common situation of implant patients and practice preventing covid-19
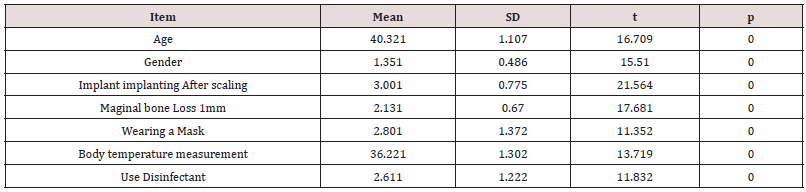
Implant patients, general conditions, and preventive practice of Covid-19 are older than 40.321 (1.1072), Gender 1.351 (.486) men, implant implanting after scaling 3.001 (.775), and more men. Marginal bone Loss 1mm 2.131 (.670), mask repeat 2.801 (1.372), paper towel 3.221 (1.302) and f94 mask wear 2.611 (1.222)
General situation of Dental hygienists and the practice of preventing Covid-19
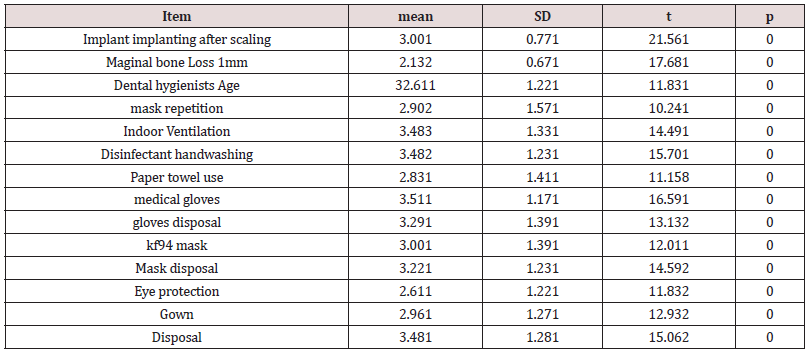
(Table 2) General situation of Dental hygienists and the practice of preventing Covid-19 (n=31). In the general situation of Dental hygienists and in the practice of preventing Covid-19, implant implanting after scaLing3.001(.771), marginal bone Loss 1mm2.132(.671), Dental hygienists Age32.611(1.221),mask repetition 2.902(1.571), indoor ventiLation3.483(1.331), disinfectant hand washing 3.482(1.231), paper towel use 2.831(1.411), medical gloves 3.511(1.171), gloves disposal 3.291(1.391), kf94 mask 3.001(1.391), mask disposaL3.221(1.231), eye protection 2.611 (1.221), gown 2.961 (1.271), and disposaL3.481 (1.281) (Table 2).
Age of Dental hygienists and samples of preventive practice t-test
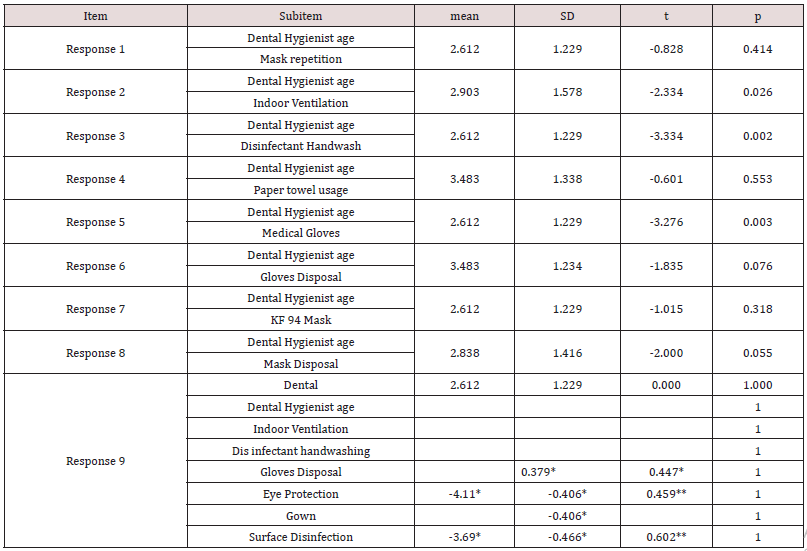
In correlation analysis such as wearing a mask repeatedly, using a paper towel, and wearing a kf94, the correlation coefficient between wearing a kf94 and using a paper towel is .447*, and the correlation coefficient between using a paper towel and surface disinfection is .379*.It shows 369*. And the correlation coefficient between wearing kf94 and glove disposal is .447*. Negative correlation coefficient between Dental hygiene age and wearing safety glasses (Table 3). It’s 411*. The correlation coefficient between indoor ventilation and surface disinfection is .602** and the correlation coefficient between hand washing and surface disinfection is. It is 602** and the negative correlation between the disposal of gloves and the safety glasses is -.406*, the correlation coefficient between the disposal of gloves and the complementary gown is -.It turned out to be 406*. The correlation coefficient between discarding masks and wearing safety glasses is. It turned out to be 459** (Table 4).
*Note at 0.05 Level (both sides), **Significant at correlation coefficient 0.01 (both sides).
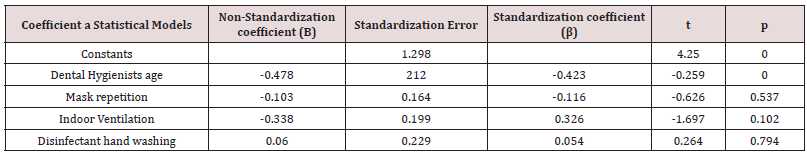
Regression with KF 94 Masks
In simple regression analysis, independent variables that significantly affect the wearing of kf94 masks at a significant Level of 0.05 are Dental hygiene age (t=-2.259, p=).033) was significant. However, repeat mask wear (t=-).626, p=.537), Ventilation(t=-1.697, p=.102.), Disinfectant Hand Washing (t=).264, p=.There is no significant difference in 794 (Table 4).
Discussion
In order to prevent the recent epidemic of infectious diseases, Dental workers should check whether they are vulnerable to infections such as underlying diseases or pregnant women, while making sure they have no symptoms of COVID-19 such as fever, cough, sore throat, and muscle pain. Masks, gowns, gloves, face guards, and personal protective equipment should be equipped to thoroughly disinfect the doctor’s office and waiting room. During Dental treatment, a mask, goggles, and facial protective equipment should be worn to prevent the patient’s blood or body fluid from splashing into the Dental worker’s eyes, nose, and mouth mucosa, and the mask (n95) should be replaced for each patient. In addition, implants have become popular as treatments for lost tooth recovery. For the Long-term success of implants after high cost and Long-term implant treatment, not only the dentist’s treatment ability but also the patient’s own maintenance and management are important. In particular, in the COVID-19 era, implant surgery should be performed, and maintenance should be more focused on preventing infectious diseases and treatment management (10). In this study, 40.321 (1.1072), 1.351 (1.486) males were Lower in general situation with implant patients[11.12] and COVID-19 prevention practice, scaling 3.001 (7.775), marginal cartilage Loss 1mm 2.131 (6.70), mask repetition 2.801 (1.372), mask usage 3.221 (1942) (Table 1). In the general situation of Dental hygienists and the practice of preventing COVID-19, scouring 3.001 (771) after implant eating, Marginal bone Loss 1MM 2.132 (1.671), Dental hygiene age 32.611 (1.221), mask repetition 2.902 (1.571), ventilation 3.483 (1.331), disinfectant hand washing 3.482 (1.231), paper towel uses 2.831 (1.411), medical gloves worn 3.511 (1.171), gloves disposal 1.391 (Table 2).
The patient’s oral cavity should be disinfected with 1.6% hydrogen peroxide or 0.2% povidone, and treatment should be started, and oral radiography or extracorporeal radiography should be performed instead of panoramic photographs should be performed. Handpiece is used to prevent retreatment, rubber dam installation is prohibited, and Large-capacity inhalers should be used. Non-surgical root canal treatment is performed when treating pain, intraoral edema, and hemorrhoids, and the importance of 4handed techniques, a collaborative treatment between dentists and Dental hygienists, is emerging. After Dental treatment, disinfect personal protective equipment with soap and water, and replace it with a new one if contaminated. Disinfect chairs and Lighting Lights. The handpiece removes foreign substances every time it is used and sterilizes at high temperatures [10-12]. When returning home, you should take off your personal clothes and shoes and take a shower immediately. Disinfect the soles of your shoes. These guidelines were published in the Journals of the Dental Association. Direct contact with blood or oral secretions, contaminated instruments, indirect contact through equipment in the clinic and its surrounding surfaces, or contact with pollutants, including droplets of Liquid generated in the oral cavity or floating in the air due to aerosols. Therefore, in order to prevent infection in the Dental clinic, it is necessary to prevent contamination sources of the patient in advance by thorough medical history investigation, post-menorrhea investigation, and identifying the health status of the whole body and mouth. Medical staff should thoroughly wash their hands, wear protective equipment such as masks, gloves, safety glasses, and medical clothing, dispose of infectious waste according to the prescribed method, and disinfect the doctor’s table and equipment. And sterilization of equipment used for medical treatment. Disinfection should be observed to prevent cross-infection between patients and patients, medical staff and patients. p=.In 794), there is no significant difference (Table 4). CDC regularly recommends that you stay at home before receiving treatment, call a medical institution in advance, wear a mask before entering a medical institution’s office, cover coughs and sneezes with tissue when in a room or vehicle with others. Sneeze your hands with soap and water, and avoid sharing household items [13,14]. The back is being announced. The importance and importance of this study were conducted from a new perspective in that Dental workers were able to closely check whether the disinfection and sterilization of various instruments, materials, and equipment used to prevent cross-infection from implant patients to patients. The Limitations of the research method of this study and the vulnerabilities of research design are explained as follows. In the COVID-19 era, Dental hygienists in charge of general affairs from patient counseling to management at the forefront of Dental clinical sites should also be provided with institutional procedures, administrative and financial support to improve infection control.
Conclusion
In January 2021, this study conducted a questionnaire survey on 30 patients undergoing management after implantation at Y Dental Clinic and 30 female Dental workers working at Y Dental Clinic and continuing to perform management in G City. After visiting the dentist in person, explaining the purpose of the study and how to fill out the questionnaire, it was self-filled and collected. The COVID-19 prevention practice questionnaire of implant patients was 7 questions, and the Dental worker’s COVID-19 prevention practice was 14 questions, measured on the Likert 5-point scale. The COVID-19 prevention practice questionnaire of implant patients is 7 questions, incLuding age, gender, scaling after implant eating, 1mm Loss of marginal cartilage, wearing a mask, measuring body temperature, and using disinfectants. 14 questions for Dental workers under management are scaling, 1MM Loss of peritoneum, Dental hygiene age, repetitive wearing of masks, indoor ventilation, disinfectant handwashing, paper towels, wearing medical gloves, wearing kf94 masks every time, mask peg, safety glasses, supplementary gown, peg.
References
- (2016) Summary of infection prevention practices in dental settings. CDC (Centers for Disease Control and Prevention).
- (2020) Cleaning and disinfection of environmental surfaces in the context of COVID-19, WHO.
- (2019) Best Practices for Environmental Cleaning in Healthcare Facilities: in Resource-Limited Settings (ver 1).
- (2020) Novel coronavirus (2019-nCoV) Guidance for primary care Management of patients presenting to primary care Version 5.0.
- (2020) Novel coronavirus (2019-nCoV) infection prevention and control guidance.
- (2020) Cleaning and disinfection of environmental surfaces in the context of COVID-19.
- (2020) Novel coronavirus (2019-nCoV) infection prevention and control guidance.
- Jung WK, Kang EJ, Yoon MS (2002) Dental Infection Control. Daehan Narae Publishing Co pp. 33-171.
- OH SG, Kim GG (1994) Recommended infection control practice for dental circles. Journal of the Korean Dental Association 32: 409-416.
- Yoo Em, Shim Hj (2008) The Relationship between Dental Medical Consumers' Knowledge and Expectations for Implants. Korean Society of Dental Hygiene 10(4).
- Lindhe J, Nyman S (1984) Long-term maintenance of patients treated for advanced periodontal disease. J CLin Periodontol 11(8): 504-514.
- Garrett JS (1977) Root planing: a perspective. J Periodontol 48(9): 553-537.
- Viral Load Exposure Factors.
- (2020) Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant Community-Based Transmission. U.S. Centers for Disease Control and Prevention (CDC).
- (2020) Scientific Brief: SARS-CoV-2 and Potential Airborne Transmission. COVID-19 Published Science and Research. US Centers for Disease Control and Prevention (CDC).
- Centers for Disease Control and Prevention (2020). What to Do if You Are Sick. U.S. Centers for Disease Control and Prevention (CDC).
Editorial Manager:
Email:
pediatricdentistry@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...