Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6636
Research Article(ISSN: 2637-6636) 
A Study on Scaling and the Success Rate of Implants After Implantation Volume 5 - Issue 5
Hee Ja Na1 and Jo Se Rim2*
- 1Department of Dental Hygiene, Honam University, Korea
- 2Department of Dental Hygiene, Dankook University, Korea
Received:February 04, 2021 Published: March 02, 2021
*Corresponding author: Jo Se Rim, Department of Dental Hygiene, Dankook University, Korea
DOI: 10.32474/IPDOAJ.2021.05.000221
Abstract
Objective: In this study, patients wearing dental prostheses after implantation were constantly observed for their masticatory function to measure the amount of marginal bone loss obtained for 1 and2 years after mounting prostheses clinically, investigate the relationship between the amount of marginal bone loss occurring for a year after wearing prostheses and the gender, age, and scaling, and use the results as reference for performing implantation and determining prognosis.
Methods: From January to February 2021, a study on scaling and the success rate of implants after implantation was carried out in a total of 31 patients including 20 male and 11 female patients with dental prostheses implanted a year ago in Y dental hospital located in Kwangju City. G-Power program was used for the study subjects of 31 patients. A survey was conducted on 31 patients from Y dental hospital in Kwangju who has agreed upon information collection about the age, gender, implantation site, length of time wearing prostheses, marginal bone loss, showing symptoms of implantation success rates, follow-up management, scaling after implantation, and investigating marginal bone loss of 1mm within a year, and those who understood the purpose of the study and agreed to participated, and was the analyzed. This study was conducted after approval of Bioscience Institutional Review Board (IRB) (NO 1041223-202011-HR-24) of Honam University.
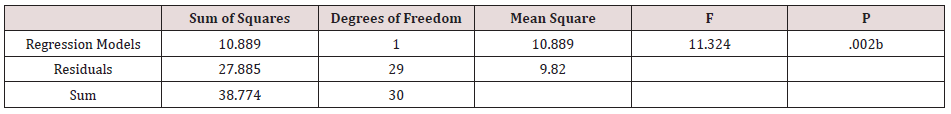
Results: The statistical significance was tested for a model measuring the implant success rates of independent variables such as marginal bone loss, management after implantation, duration of wearing prostheses, implantation period, and scaling shown in Table. According to the results, marginal bone loss, management after implantation, duration of wearing prostheses, and implantation period were excluded because they were not significant, indicating significantly that scaling of f-statistic was 11.324, and significance probability was .002, with the overall success rate of 26% (25% by modified coefficient of determination) described by independent variables which are included in the model.
Conclusion: In terms of the period of marginal bone loss, it occurred by less than 1.2mm in 10 people (32.3%) and more than 1.2mm in 5 people (16.1%) within a year, and by less than 0.2mm in 3 people (9.7%) and more than 0.2mm in 13 people (41.9%) for more than two years. The average and standard deviation were 2.61(1.334), t=8.82, respectively and p=.00.
Keywords: Implantation; scaling; successful implantation; marginal bone loss; implant mounting
Introduction
Recently, because of the high success rate of implant procedures and constant development, it has been replacing the existing complete dentures, removable partial dentures, and fixed partial dentures in many ways. The long-term success results of implants decided by maintenance of supporting bone around the implants. The stability of bone sites around the implants and maintenance of osseous integration may be most important for successful implants procedure. Moreover, the criteria for implant success were suggested as follows: there should never be implant mobility in single subject experiments of implants; there should be no radiolucent lines; there should be no pain, swelling, numbness, etc.; the average amount of marginal bone loss around implants should be less than 1.5mm for a year after functioning; and after that, the amount of marginal bone loss around implants should be less than 0.2mm every year. Multiple studies were carried out on, among success criteria, marginal bone loss around implants during the initial period. The early marginal bone loss on the surface connecting implants and tissues begins at the marginal site in intraosteal implants with successful interosseous integration [1]. Particularly, marginal bone loss around implants for a year after functioning progresses up to the first spiral of a titanium screw or a little beyond it, and it shows a dish (V,U) shape in radiography. The first article which quantitated the amount of the early marginal bone loss reported that, in implants of a fully edentulous patient who had been observed for 15 years, marginal bone loss around implants for a year after functioning which is the healing and regenerating period of bone tissue was 1.2mm on average, while the average amount of bone loss was 0.1mm every year [2]. The criteria for implant survival rates by Buser et al. were evaluated with the method of the study. The criteria in clinical examinations of each implant were: there should be no mobility; there is no pain or subjective paresthesia; there is no peri-implant inflammation; there is no constant peri-implant radiolucency [3].
In addition, the success rate of implants was set in accordance with the criteria by Albrektsson that there should be no mobility, pain, paresthesia, radiolucent lesions, peri-implant inflammation, and progressive bone resorption, and marginal bone loss is less than 1mm within a year after implantation and less than 0.2mm after that [1]. Practicing personal oral hygiene after implant procedures is emphasized. In order to prolong the longevity of implants, the utility of various oral hygiene tools such as a toothbrush, dental floss, interdental brush is important, and regular dental scaling is necessary most of all. Non-surgical periodontal therapy (NSPT) is also known as scaling and root planning (SRP) of teeth and the surfaces of the roots, which prevents chronic periodontitis (CP) [4-6] and contributes to the increase in the success rate of implants. In this study, the distance between the implant shoulder and the attachment sites of the mesial and distal alveolar bone was measured to calculate the average, using a radiographic ruler in intraoral periapical x-rays at the time of mounting prostheses after implantation and in periapical and panoramic x-rays within a year after that. In addition, it is questioned that marginal bone loss and scaling have significant impact on t the success rate of implants. Based on these previous studies, in this study, patients practicing masticatory function with prostheses after implantation were constantly observed to measure the amount of marginal bone loss obtained for 1 and 2 years after wearing prostheses clinically, investigate the relationship between the amount of marginal bone loss occurring for a year after prosthesis mounting and the gender, age, and scaling, and use the results as reference for implant procedures and prognosis determination. In future study ranges after this study, it is desired to redeem insufficiency of domestic studies on the success rate of implants and oral hygiene management.
Material & Method
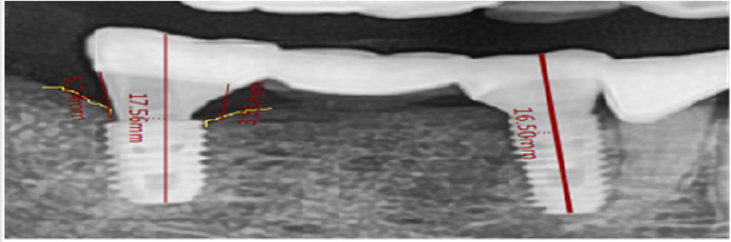
From January to February 2021, the study was conducted with a total of 31 patients including 20 male and 11 female patients wearing and using dental prostheses after implant procedures a year ago in Y dental hospital located in Kwangju City. G-Power program was used for the study subjects of 31 patients. The distance between the implant shoulder and the attachment sites of the mesial and distal alveolar bone was measured to calculate the average, using a radiographic ruler in intraoral periapical x-rays at the time of mounting prostheses after implantation and in periapical and panoramic x-rays within a year after that (Figure 1). Ossification symptoms of bone (DP-80-P/PM2002 EC Proline, Planmeca, Helsinki, Finland) (Figure 2) by the lapse of time after implantation were evaluated on radiographs A survey was conducted on 31 patients from Y dental hospital in Kwangju who has agreed upon information collection about the age, gender, implantation site, length of time wearing prostheses, marginal bone loss, showing symptoms of implantation success rates, follow-up management, scaling after implantation, and investigating marginal bone loss of 1mm within a year, and those who understood the purpose of the study and agreed to participated, and was the analyzed. This study was conducted after approval of Bioscience IRB (NO 1041223- 202011-HR-24) of Honam University.
In terms of age, 30s were No.1, 40s No.2, 50s No.3, 60s No.4, and 70s No.5, showing that the higher the score, the older the age. The gender was measured as No.1 in male and No.2 in female, and the implantation sites were measured as No.1 of maxillary anterior regions, No.2 of maxillary molar regions, No.3 of mandible anterior regions, No.4 of mandible molar regions, and No.5 of the full mouth. Duration of wearing prostheses was investigated as No.1 of 3 months, No.2 of 6 months, No.3 of 1 year, No.4 of 1.5 years, and No.5 of 2 years, and marginal bone loss with No.1 of less than 1.2mm within a year, No.2 of more than 1.2mm within a year, No.3 of less than 0.2mm for more than 2 years, No. 4 of more than 0.2mm for more than 2 years, and No. 5 of 0.3mm for more than 2 years. In terms of showing symptoms of implant non-success rates, No.1 was for ‘strongly disagree’, No.2 for ‘disagree’, No.3 for ‘neither agree nor disagree’, No.4 for ‘agree’, and No.5 for ‘strongly agree’. Regarding management after implantation, No.1 was a decline in the immune system, No.2 inadequate compression after implantation, No.3 oral hygiene management, No.4 filthy mouth, and No.5 drinking and smoking. Scaling after implantation was measured as No.1 of twice, No.2 of 3 times, No.3 of 5 times, No.4 of 7 times, and No.5 of 9 times, and marginal bone loss of 1mm within a year was measured with No.1 ‘strongly disagree’, No.2 ‘disagree’, No.3 ‘neither agree nor disagree’, No.4 ‘agree’, and No.5 ‘strongly agree’. For marginal bone loss, based on a five-point Likert scale, 1 point was given to ‘Strongly disagree’ and 5 points to ‘Strongly agree’, where the higher scores mean the higher level of showing symptoms of implant success rates. The questionnaires were prepared according to the criteria of Zarb and Albrektsson [7] for the success rate of implants, including no mobility, pain, paresthesia, radiolucent lesions, and peri-implant inflammation, and a case where there is no progressive bone resorption (set as less than 1mm within a year after implantation and less than 0.2mm after that).
Results
General characteristics
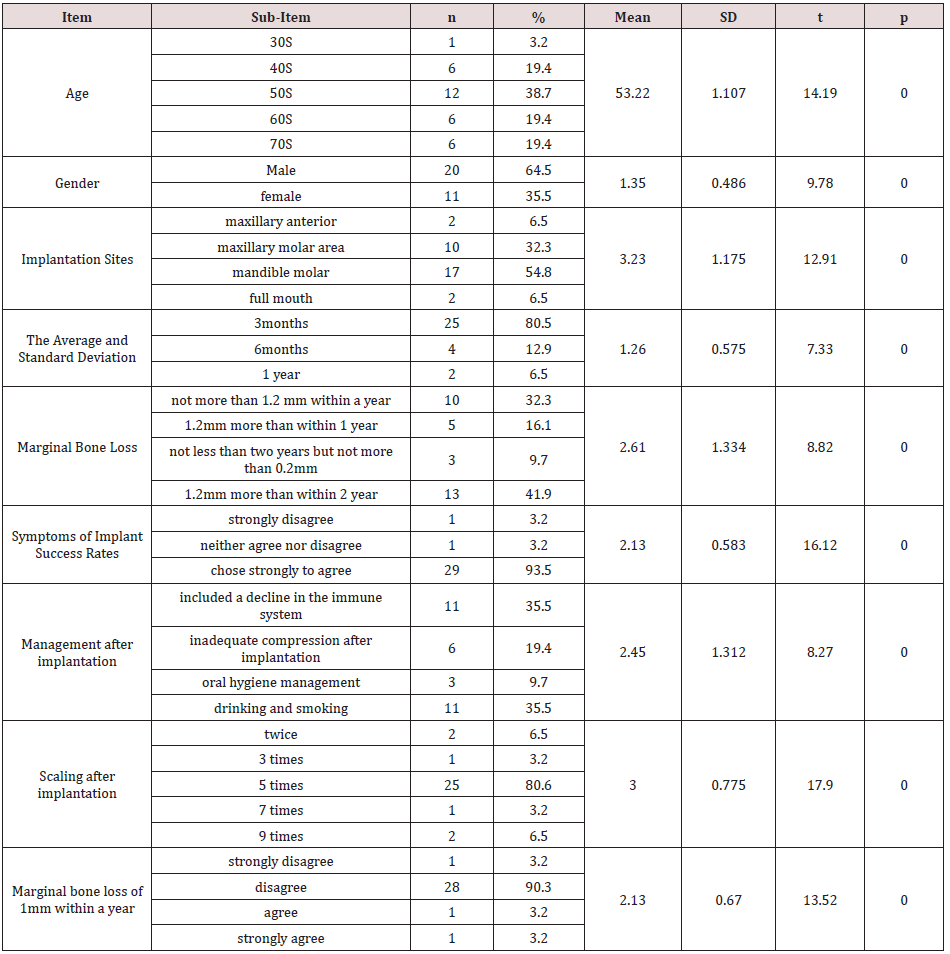
Table 1 of this study shows general characteristics in which 1 person (3.2%) was in one’s 30s, 6 people (19.4%) in 40s, 12 (38.7%) in 50s, 6 (19.4%) in 60s, and 6 (19.4%) in 70s. The average and standard deviation were 53.2(1.107) and t=14.19, respectively, and p=.00. In terms of gender, male accounted for 64.5% (20 people), and female 35.5% (11 people), and the average and standard deviation were 1.35(.486) and t=9.78, respectively, and p=.00. Regarding the implantation sites, a maxillary anterior region was shown in 2 people (6.5%), a maxillary molar region in 10 people (32.3%), and a mandible molar region in 17 (54.8%). The full mouth was shown in 2 people (6.5%), and the average and standard deviation were 3.23(1.175) and t=12.91, respectively, and p=.00. Length of time of wearing prostheses was 3 months in 25 people (80.5%) and 6 months in 4 people (12.9%), and the average and standard deviation were 1.26(.575) and t=7.33, respectively, and p=.00. Marginal bone loss occurred in 10 people (32.3%) by less than 1.2mm within a year, 5 people (16.1%) by more than 1.2mm within a year, 3 people (9.7%) by less than 0.2mm for more than 2 years, and 13 people (41.9%) by more than 0.2mm for more than 2 years, and the average and standard deviation were 2.61(1.334) and t=8.82, respectively and p=.00.
In terms of showing symptoms of implant success rates, 20 people (93.5%) chose strongly to agree, 1 person (3.2%) neither agree nor disagree, and 1 person (3.2%) strongly disagree, and the average and standard deviation were 2.13(583) and t=16.12, respectively, and p=.00. Management after implantation included a decline in the immune system in 11 people (35.5%), inadequate compression after implantation in 6 people (19.4%), oral hygiene management in 3 people (9.7%), and drinking and smoking in 11 people (35.5%), and the average and standard deviation were 3.00(.775) and t=17.90, respectively, and p=.00. Scaling after implantation was shown twice in 2 people (6.5%), 3 times in one person (3.2%), 5 times in 25 people (80.6%), and 7 times in 1 person (3.2%). As for the response about marginal bone loss of 1mm within a year, 1 person (3.2%) chose ‘strongly disagree’, 28 people (90.3%) ‘disagree’, 1 person (3.2%) ‘agree’, and 1 (3.2%) ‘strongly agree’. The average and standard deviation were 2.13 (.670) and t=13.52, respective and p=.00. This study analyzed data of the age and gender of patients, implantation sites, duration of wearing prostheses, marginal bone loss, showing symptoms of implant success rates, management and scaling after implantation, and marginal bone loss of 1mm within a year, and also showed the implant success rate answered with ‘strongly agree’ in 20 people (93.5%), ‘neither agree nor disagree’ in 1 person (3.2%), and ‘disagree’ in 1 (3.2%). The average and standard variation were 2.13(583) and t=16.12, respectively and p=0.00 (Table 1).
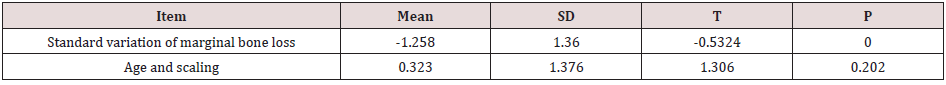
Standard variation of marginal bone loss
In this study as well, as results of the paired sample t-test, the average and standard variation of marginal bone loss were -1.258 and 1.36, respectively, and the average of age and scaling was 0.323 while the standard variation was 1.376. The statistical significance was tested with the results that for gender and marginal bone loss, t=-.5324 and the significance probability was 0.000, showing the significant difference in the significance level of 0.05 (Table 2).
Success rates of implants correlation analysis
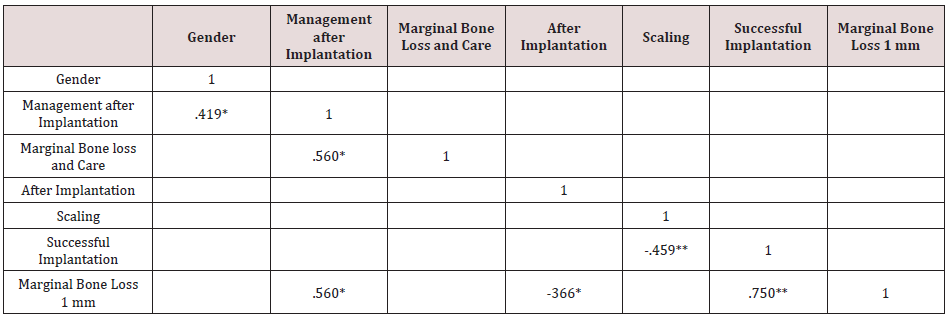
This study showed the correlation coefficient of .419* between the age and management after implantation, the correlation coefficient of .560** between marginal bone loss and management after implantation, and a negative correlation coefficient of -3.66** between the implantation period and marginal bone loss of 1mm within a year. In addition, a negative correlation coefficient between scaling and successful implantation was -.459**, while the correlation coefficient between marginal bone loss of 1mm and success rates of implants was .750**. The relationships between the gender and management after implantation and between marginal bone loss and management after implantation were significant in the significance level of 0.05, scaling and implant success rates were correlation coefficients, and marginal bone loss of 1mm within a year and successful implantation were significant in the significance level of 0.01 (Table 3).
Table 3: Gender, management after implantation, marginal bone loss and care scaling, marginal bone loss 1 mm, successful implantation Correlation (n=31).
Management after implantation., management after implantation, duration of wearing prostheses after implantation, scaling ANOVA
The statistical significance was tested for a model measuring the implant success rates of independent variables such as marginal bone loss, management after implantation, duration of wearing prostheses, implantation period, and scaling shown in Table 4. According to the results, marginal bone loss, management after implantation, duration of wearing prostheses, and implantation period were excluded because they were not significant, indicating significantly that scaling of f-statistic was 11.324, and significance probability was .002, with the overall success rate of 26% (25% by modified coefficient of determination) described by independent variables which are included in the model.
Medium-variable analysis according to implant success rate
Contribution of individual independent variables to dependent variables and statistical contribution were tested with the results that scaling (t=-2.483, p=.020) significantly affected successful implantation in the significance level of 0.05 (Table 5).
Table 5: Medium-variable analysis according to implant success rate (N=31).
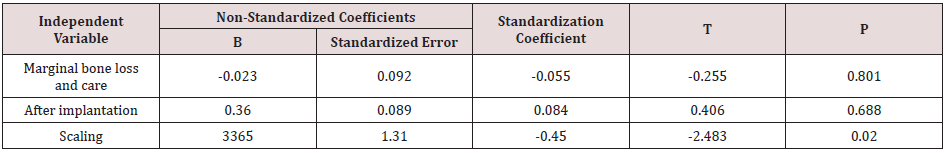
Dependencies: Implants successful.
Discussion
Looking into the literature related to the success and failure of implant treatment, Kim et al. [8] reported the success rate of 96.8% up to the stage before mounting prostheses after inserting 1058 implants in 306 patients, and Drago et al. [9] reported only one failure in implant restoration using just 83 internal connection implants in 45 patients, while Zarb and Schmitt reported the failure rate of 11%, Lekholm and Gunne 11%, and Quirynen and Listgarten 6% [10,11]. The success rate of implants means the ratio of implants meeting the success criteria after the specific period of time, based on the evaluation criteria for clinical adequacy of implants but the success in implants cannot be affirmed until the time passes. On the contrary, the survival rate is defined as the ratio of implants remaining in the mouth until before the implants are removed or it is decided to remove implants. Table 1 of this study shows general characteristics in which 1 person (3.2%) was in one’s 30s, 6 people (19.4%) in 40s, 12 (38.7%) in 50s, 6 (19.4%) in 60s, and 6 (19.4%) in 70s. The average and standard deviation were 53.2(1.107) and t=14.19, respectively, and p=.00. In terms of gender, male accounted for 64.5% (20 people), and female 35.5% (11 people), and the average and standard deviation were 1.35(.486) and t=9.78, respectively, and p=.00. Regarding the implantation sites, a maxillary anterior region was shown in 2 people (6.5%), a maxillary molar region in 10 people (32.3%), and a mandible molar region in 17 (54.8%).
The full mouth was shown in 2 people (6.5%), and the average and standard deviation were 3.23(1.175) and t=12.91, respectively, and p=.00. Length of time of wearing prostheses was 3 months in 25 people (80.5%) and 6 months in 4 people (12.9%), and the average and standard deviation were 1.26(.575) and t=7.33, respectively, and p=.00. Marginal bone loss occurred in 10 people (32.3%) by less than 1.2mm within a year, 5 people (16.1%) by more than 1.2mm within a year, 3 people (9.7%) by less than 0.2mm for more than 2 years, and 13 people (41.9%) by more than 0.2mm for more than 2 years, and the average and standard deviation were 2.61(1.334) and t=8.82, respectively and p=.00. In terms of showing symptoms of implant success rates, 20 people (93.5%) chose strongly to agree, 1 person (3.2%) neither agree nor disagree, and 1 person (3.2%) strongly disagree, and the average and standard deviation were 2.13(583) and t=16.12, respectively, and p=.00. Management after implantation included a decline in the immune system in 11 people (35.5%), inadequate compression after implantation in 6 people (19.4%), oral hygiene management in 3 people (9.7%), and drinking and smoking in 11 people (35.5%), and the average and standard deviation were 3.00(.775) and t=17.90, respectively, and p=.00. Scaling after implantation was shown twice in 2 people (6.5%), 3 times in one person (3.2%), 5 times in 25 people (80.6%), and 7 times in 1 person (3.2%). As for the response about marginal bone loss of 1mm within a year, 1 person (3.2%) chose ‘strongly disagree’, 28 people (90.3%) ‘disagree’, 1 person (3.2%) ‘agree’, and 1 (3.2%) ‘strongly agree’. The average and standard deviation were 2.13 (.670) and t=13.52, respective and p=.00. This study analyzed data of the age and gender of patients, implantation sites, duration of wearing prostheses, marginal bone loss, showing symptoms of implant success rates, management and scaling after implantation, and marginal bone loss of 1mm within a year, and also showed the implant success rate answered with ‘strongly agree’ in 20 people (93.5%), ‘neither agree nor disagree’ in 1 person (3.2%), and ‘disagree’ in 1 (3.2%).
The average and standard variation were 2.13(583) and t=16.12, respectively and p=.00 (Table 1). Results of studies on the success rate of implants associated with the age and gender of patients vary by scholars. Bryant et al. reported that bone resorption increases more than bone generation in bone metabolism as people age, leading to a tendency of decrease in bone density, cortical bone thinning, and an increase in porosity of cancellous bones, which can affect the success rate of implants [12], while Smith et al. reported that age has no impact on implant success rates. In this study as well, as results of the paired sample t-test, the average and standard variation of marginal bone loss were -1.258 and 1.36, respectively, and the average of age and scaling was .323 while the standard variation was 1.376. The statistical significance was tested with the results that for gender and marginal bone loss, t=-.5324 and the significance probability was .000, showing the significant difference in the significance level of .05 (Table 2). This study showed the correlation coefficient of .419* between the age and management after implantation, the correlation coefficient of .560** between marginal bone loss and management after implantation, and a negative correlation coefficient of -3.66** between the implantation period and marginal bone loss of 1mm within a year. In addition, a negative correlation coefficient between scaling and success rates of implants was -.459**, while the correlation coefficient between marginal bone loss of 1mm and success rates of implants was .750**.
The relationships between the gender and management after implantation and between marginal bone loss and management after implantation were significant in the significance level of 0.05, scaling and implant success rates were correlation coefficients, and marginal bone loss of 1mm within a year and implant success rates were significant in the significance level of 0.01 (Table 3). It was presented in several articles that in the case of edentulous patients wearing overlay dentures or fixed full-arch implants after implantation, the amount of marginal bone loss around implants was 1.64mm a year after functioning and 0.05-0.13mm every year after that, while in the case of partial edentulous patients wearing fixed partial dentures supported by implants, the amount of marginal bone loss around implants was 0.4-1.5mm a year after functioning, and 0.05-0.10mm every year after that [13]. It was also shown in this study that duration of marginal bone loss was within a year with less than 1.2mm in 10 people (32.3%), within a year with more than 1.2mm in 5 people (16.1%), for more than 2 years with less than 0.2mm in 3 people (9.7%), and for more than 2 years with more than 0.2mm in 13 people (41.9%). The average and standard deviation were 2.61(1.334) and t=8.82, respectively and p=.00 (Table 1). Since the first one year after implantation is the period of healing and regeneration, bone tissue is not strong enough yet, showing lots of marginal bone loss by various causes. The causes include surgical damage, overloading, peri-implant inflammation, the micro space between implants and abutments, reformation of biologic width, sloping of upper implants, etc.
Surgical damages may include heat occurring in forming intraosseous space for implantation and injury occurring in stress concentration and lifting periodontal membrane [14], however, this study showed a decline in the immune system in management after implantation in 11 people (35.5%), inadequate compression after implantation in 6 (19.4%), oral hygiene management in 3 (9.7%), and drinking and smoking in 11 (35.5%), and the average and standard deviation were 3.00(.775) and t=17.90, respectively and p=.00. Scaling after implantation was practiced twice in 2 people (6.5%), 3 times in 1 (3.2%), 5 times in 25 (80.6%), and 7 times in 1 (3.2%) (Table 1). Toothbrushing removes acquired pellicle attached between the surface of teeth and the adjacent surface, food residue, and dental plaque, and increases blood supply to the gums by massaging them and improves resistance to infection by promoting keratinization of gingival epithelium. Toothbrushing is the basic of prevention strategy and the use of an interdental brush and dental floss which are auxiliary oral hygiene devices should be practiced. Scaling 1-2 times a year and professional mechanical tooth cleaning (PMTC) for the applicable parts can reduce the growth of oral bacteria and prevent oral diseases [15]. In general, toothbrushing and scaling should be practiced based on a person wearing fixed prostheses and damage to dental implants should be avoided. Dental plaque is easily attached to the boundary area of implants mounted with an artificial crown; therefore, dental education is needed so that the lifespan of implants can be prolonged by intensive and careful brushing. The statistical significance was tested for a model measuring the implant success rates of independent variables such as marginal bone loss, management after implantation, duration of wearing prostheses, implantation period, and scaling shown in Table 4. According to the results, marginal bone loss, management after implantation, duration of wearing prostheses, and implantation period were excluded because they were not significant, indicating significantly that scaling of f-statistic was 11.324, and significance probability was .002, with the overall success rate of 26% (25% by modified coefficient of determination) described by independent variables which are included in the model.
Contribution of individual independent variables to dependent variables and statistical contribution were tested with the results that scaling (t=-2.483, p=.020) significantly affected the success rate of implants in the significance level of 0.05 (Table 5). The difference between this study and previous studies is that the result of testing statistical significance about a model measuring implant success rates of independent variables such as marginal bone loss, management after implantation, duration of wearing prostheses, implantation period, scaling, etc., scaling was indicated significantly with f-statistic of 11.324 and significance probability of .002 and the overall implant success rate of 26% (25% in modified coefficient of determination) are elucidated by independent variables included in the model. The importance of this study is that a new attempt was made in this study predominantly showing the success rate of implants after marginal bone loss, management after implantation, and scaling, in comparison with other studies. Therefore, it aims to increase the success rate of implants by performing scaling for implant patients. The limitation of this study that follow-up period was no longer than one year. In future studies, it is aimed to increase the success rate of implants by following up for 2 years of more.
Conclusion
From January to February 2021, the study was conducted with a total of 31 patients including 20 male and 11 female patients wearing dental prostheses after implantation a year ago in Y dental hospital located in Kwangju City. G-Power program was used to evaluate the study subjects of 31 patients.
a) In general characteristics, the age of patients consisted of 1 person (3.2%) in 30s, 6 people (19.4%) in their 40s, 12 (38.7%) in 50s, 6 (19.4%) in 60s, and 6 (19.4%) in 70s.
b) This study also showed the success rate of implants from the survey answers with ‘strongly agree’ in 20 people (93.5%), ‘neither agree nor disagree’ in 1 person (3.2%), and ‘disagree’ in 1 (3.2%). The average and standard variation were 2.13(583) and t=16.12, respectively and p=.00.
c) The correlation coefficient of between the age and management after implantation was .419*, the correlation coefficient between marginal bone loss and management after implantation was .560**, and a negative correlation coefficient between the implantation period and marginal bone loss of 1mm within a year was -3.66**. In addition, a negative correlation coefficient between scaling and success rates of implants was -.459**, while the correlation coefficient between marginal bone loss of 1mm and success rates of implants was .750**. The relationships between the gender and management after implantation and between marginal bone loss and management after implantation were significant in the significance level of 0.05, scaling and implant success rates were correlation coefficients, and marginal bone loss of 1mm within a year and implant success rates were significant in the significance level of 0.01.
d) In terms of duration of marginal bone loss, 10 people (32.3%) showed less than 1.2mm within a year, 5 people (16.1%) more than 1.2mm within a year, 3 people (9.7%) less than 0.2mm for more than 2 years, and 13 people (41.9%) more than 0.2mm for more than 2 years. The average and standard deviation were 2.61(1.334) and t=8.82, respectively and p=.00.
e) Management after implantation included a decline in the immune system in 11 people (35.5%), inadequate compression after implantation in 6 people (19.4%), oral hygiene management in 3 people (9.7%), and drinking and smoking in 11 people (35.5%), and the average and standard deviation were 3.00(.775) and t=17.90, respectively, and p=.00. Scaling after implantation was shown twice in 2 people (6.5%), 3 times in one person (3.2%), 5 times in 25 people (80.6%), and 7 times in 1 person (3.2%) [6].
f) Contribution of individual independent variables to dependent variables and statistical contribution were tested with the results that scaling (t=-2.483, p=.020) significantly affected the successful implantation in the significance level of 0.05.
References
- Albrektsson T, Zarb G, Worthington P, Eriksson AR (1986) The longterm efficacy of currently used dental implants: A review and proposed criteria of success. Int J Oral Maxillofac Implants 1: 11-25.
- Adell R, Lekholm U, Rockler B, Branemark P-I (1981) A 15-year study of osseointegrated implants in the treatment of edentulous jaw. Int J Oral Surg 10(6): 387-416.
- Buser D, Mericske-Stern R, Bernard JP, Behneke A, Behneke N, et al. (1997) Long-term evaluation of non-submerged ITI implants. Part 1: 8-year life table analysis of a prospective multi-center study with 2359 implants. Clin Oral Implants Res 8(3): 161–172.
- AlAhmari F, Ahmed HB, Al-Kheraif AA, Javed F, Akram Z (2019) Effectiveness of scaling and root planning with and without adjunct antimicrobial photodynamic therapy in the treatment of chronic periodontitis among cigarette-smokers and never-smokers: a randomized controlled clinical trial. Photodiagnosis Photodyn Ther 25: 247-252.
- Jia L, Jia J, Xie M, Zhang X, Li T, et al. (2020) Clinical attachment level gain of lasers in scaling and root planing of chronic periodontitis: a network meta-analysis of randomized controlled clinical trials. Lasers Med Sci 35920: 473-485.
- Mohan R, Varghese J, Bhat V, Chianeh YR (2019) The effect of nonsurgical periodontal therapy on pentraxin 3 levels in smokers and nonsmokers with chronic periodontitis. Gen Dent 6(2): 1-6.
- Albrektsson T, Branemark PL, Hansson HA, Lindstrom, J (1981) Osseo interated titanium implants. Requirements for ensuring a long –lasting, direct bone-to-implant anchorage in mam. Acta Ortho p Scand 52: 155-170.
- Kim JS, Chang HH, Chang CH, Rhyu SH, Kang JH (2001) Pre prosthetic Stage Dental Implant Failure. J Kor Oral Maxillofac Surg 27: 178-83.
- Carl J Drago, C Garry O'Connor (2006) A clinical report on the 18-month cumulative survival rates of implants and implant prostheses with an internal connection implant system. Compend Contin Educ Dent 27(4): 266-271.
- Schmitt A, Zarb GA (1993) The longitudinal clinical effectiveness of osseo integrated dental implants for single-tooth replacement. Int J Prosthodont 6(2): 197-202.
- Lekholm U, Gunne J, Henry P, Higuchi K, Linden U, et al. (1999) Survival of the Branemark implant in partially edentulous jaws: a 10-year prospective multicenter study. Int J Oral Maxillofac Implants 149(5): 639-645.
- Bryant SR (1998) The effects of age, jaw site, and bone condition on oral implant outcomes. Int J Prosthodont 11(5): 470-490.
- Henry PJ, Tolman DE, Bolender C (1993) The applicability of osseo integrated implants in the treatment of partially edentulous patients: three years results of a prospective multicenter study. Quintessence International 24: 123-129.
- Esposito M, Hirsch JM, Lekholm U, Thomsen P (1998) Biological factors contributing to failures of osseo integrated oral implants. Etiopathogenesis Eur J Oral Sci 106: 721-764.
- Mcgrath C, Bedi R (2004) A national study of the importance of oral health to life quality to inform scales of oral health related quality of life res 13(4): 813-818.
Editorial Manager:
Email:
pediatricdentistry@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...