Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6628
Research Article(ISSN: 2637-6628) 
Correlation Between Indicators of Blood Cells Aggregation Level and the Number of Lymphoblasts and Monocytes in Patients with Glioblastomas Volume 5 - Issue 4
Pedachenko Eugene Georgievich1, Morozov Anatolyi Nikolaevich1, Gridina Nina Yakovlevna1*, Glavatsky Alexandr Yakovlevich1, Kot Larisa Anatolievna1, Ushenin Yuryi Valentinovich2, Draguntsova Nataliya Gennadievna1, Khristosenko Roman Vasilyevich2 and Belousova Anna Dmitrievna1
- 1Institute of Neurosurgery, A P Romodanov Institute of Neurosurgery, Kiev, Ukraine
- 2Institute of Semiconductor Physics , V E Lashkaryova, Kiev, Ukraine
Received:May 13, 2021 Published:May 21, 2021
Corresponding author:Gridina Nina Yakovlevna , Institute of Neurosurgery, A P Romodanova, Kiev, Ukraine
DOI: 10.32474/OJNBD.2021.05.000220
Abstract
The inflammatory process is an important part of malignant brain gliomas progression mechanism. The inflammation induced by tumor tissue necrosis is called tumor-associated inflammation (TAI). Taking into account the leading role of TAI in the gliomas progression, the aim of the work was to study the correlation between the indicator of the inflammatory process and the number of potential blood stem cells - lymphoblasts and monocytes. These cells are involved in the processes of tissue regeneration in the wound focus after surgery for the removal of tumors. The wound tumor focus was named “non-healing wound” as a result of the activation of TAI which prevents the formation of normal tissue cytoarchitectonics by blood stem cells, which are exposed to the destructive effects of inflammation factors. Studies have found a negative correlation between the indicators of stage II inflammation - the level of blood cells aggregation, measured in SPR (surface plasmon resonance) units using the highly sensitive Plasmon biosensor, and the number of lymphoblasts, formed in the RBTL test in vitro, and Mid cells, containing monocytes in peripheral blood in patients with glioblastomas.
Keywords: Glioblastomas; Tumor-Associated Inflammation; Regeneration; Blood Cells Aggregation; Lymphoblasts; Monocytes; Negative Correlation
Introduction
The study of malignant tumors treatment problems encounters difficulties due to the lack of a deep understanding of malignant growth mechanisms. Many researchers assume that each type of tumor has its own, tissue-specific mechanism, without taking into account of the fundamental pathophysiological laws that postulate a single mechanism for all types of malignant tumors, despite their origin from different organs and tissues. Some authors suggest that the heterogeneity of glioblastomas leads to the manifestation of a systemic factors variety that can become prognostic markers [1-2], which will facilitate the development of individual adjuvant therapy for patients. Such an approach would greatly complicate the treatment of patients with malignant brain tumors, while proving to be ineffective. The difficulty of disclosing the mechanism of tumor growth is that the mechanism of benign brain tumors formation consists of the various mutations appearance in the cellular genome, incl. and nonspecific for tumors; loss of heterozygosity in cerebral gliomas exceeding 90% [3]; aneuploidy and premature divergence of centromeres in chromosomes [4-5]. When a benign process turns into a malignant one, an important condition is the activation of a tumor-associated process, while the severity of these anomalies increases and the main mechanism of malignant tumors will be determined by the result of the interaction of reparative (inflammatory genesis) and regenerative processes (with the participation of stem cells) in damaged body tissues against the background of a prolonged chronic inflammatory process of aseptic origin. Inflammation in the second stage is characterized by a drop in the transmembrane potential, which leads to large changes in the biochemical and cellular composition of the peripheral blood. The main cellular changes in inflammation have been known for a long time and relate to the number of leukocytes, lymphocytes, neutrophils, platelets and other types of peripheral blood cells. Recently, interest has appeared in the study of the relationship between cellular fractions, for example, lymphocytes to monocytes, leukocytes to granulocytes, etc., which, according to researchers, makes it possible to more accurately determine the diagnostic and prognostic capabilities of this approach [3-6].
The question arises, is the appearance of a certain number of cells of various types in the peripheral bloodstream a random or natural process, strictly conditioned by some factor? Most studies are carried out taking into account the protective functions of peripheral blood cells of an inflammatory nature. Of interest are blood cells, which can also participate in regenerative processes, in which tissue defects are replaced not by scar tissue, but by cell mass, taking into account the cytoarchitectonics of the tissues of this organ. Lymphoblasts formed under the action of PHA in the RBTL test acquire the properties of stem cells, which are also inherent in monocytes of the peripheral bloodstream. It has been shown that blood mononuclear cells can be reprogrammed into pluripotent stem cells [7-8]. Monocytes are the largest blood cells [9]. Monocytes, which migrate from the bloodstream to other tissues, then differentiate into tissue macrophages or dendritic cells. Macrophages are responsible for protecting tissues from foreign substances, but they are also thought to play an essential role in the formation of important organs such as the heart and brain. For successful postoperative adjuvant therapy of malignant gliomas, it is necessary to search for indicators that are closely related to the subsequent regulation of other links in the pathogenesis of gliomas. The level of transmembrane potential claims to be such an indicator. In the studies carried out, its ability to regulate the number of potential peripheral blood stem cells for the processes of tissue regeneration in the postoperative focus was studied.
The aim of the research was to find a correlation between the indicator of stage II of the inflammatory process by determining the level of aggregation of blood cells and the number of lymphoblasts in the RBTL test and monocytes in the peripheral bed simultaneously from the same blood samples from patients with neurosurgical pathology.
Materials and Methods
The study was carried out in two parallel methods to confirm the presence of a correlation between the level of aggregation of blood cells and the number of lymphoblastic cells and monocytes in view of the importance of this mechanism in understanding the progression of malignant brain tumors. In our previous studies, it was found that indicators of the level of aggregation of blood cells, measured in modern units of surface plasmon resonance [10], determined on a supersensitive biosensor of the Plasmon type, are decisive in many processes associated with metabolic changes in the body during inflammatory and tumor processes. The proliferative activity of lymphocytes was studied in 21 patients with malignant gliomas and in 15 patients with spinal hernias. Verapamil, an NMDA-dependent calcium channel blocker, has been used to decrease or increase the level of transmembrane potential (TMP) mediated by the level of aggregation of blood cells. Modification of the lymphocyte blast transformation reaction (LBTR) was carried out in vitro experiments using 0.25% solutions of verapamil - hydrochloride (Farmak). The solutions were prepared in dilutions from 10-1 to 10-5 times immediately before culturing blood cells in RPMI medium for 72 hours. To each Petri dish 2 cm in diameter was added 2 ml of RPMI medium, 600 microliters (μl) of blood cells without plasma, 60 μl of various concentrations of verapamil - hydrochloride, 60 μl of phytohemagglutinin (PHA) (Sigma, 5 mg / 5 ml H2O) and 20 μl of gentamicin. Determination of the absolute number of peripheral blood cells was carried out on an automatic hematological analyzer “Mindray - 3000”. Monocytes were detected in the pool of Mid cells of the peripheral bloodstream. Statistical studies were performed using the “Statistics-10v” package. Standardization of diverse indicators was obtained by the formula: Xn - XΣ / σ, where Xn is an individual value; XΣ - average value; σ is the standard deviation.
Method for Determining the Correlation Coefficient
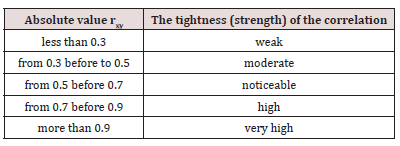
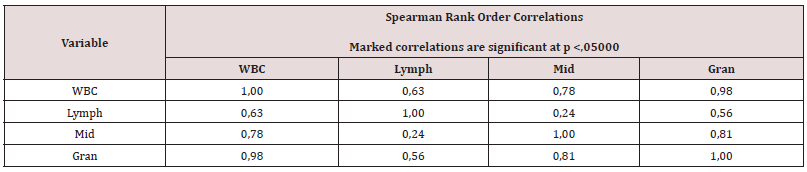
Spearman’s rank correlation coefficient is a nonparametric method that is used to statistically study the relationship between phenomena. In this case, the actual degree of parallelism between the two quantitative series of the studied features is determined and an assessment of the tightness of the established relationship is given using a quantitatively expressed coefficient. The statistical significance of the obtained coefficient is assessed using the Student’s t-test. If the calculated value of the t-test is less than the tabular value for a given number of degrees of freedom, the statistical significance of the observed relationship is absent. If more, then the correlation is considered statistically significant (Table 1).
Results and its Discussion
The use of dilutions of verapamil - hydrochloride from 10 to 100 times led to an insignificant increase in the number of lymphoblasts against the background of an increase in the level of aggregation of blood cells (decrease in SPR indices) compared with the control indices without verapamil in spinal hernias (Figure 1). In the control blood samples of patients with glioblastoma, a decrease in the percentage of lymphoblasts was noted against the background of the same increase in the level of aggregation in spinal hernias (Figure 1 and 2). At first glance, this result is a confirmation of the immunosuppressive status in gliomas, when the proliferative activity of lymphocytes decreases in response to PHA exposure.
The effect of verapamil - hydrochloride on blood cells, diluted 10 times, revealed that immunosuppression is latent and depends on the level of TMP. In Figure 2 shows that an increase in the level of aggregation of blood cells (a decrease in SPR indicators) leads to a significant increase in the proliferation activity of lymphocytes when exposed to a dilution of verapamil by a factor of 10.
Figure 1: Standardized indices of SPR of blood cells in comparison with the number of lymphoblasts (in%) cultured using different dilutions of verapamil- hydrochloride for spinal hernias (in the RBTL test). Legend: ctrl - blood samples without vrapamil - hydrochloride added.
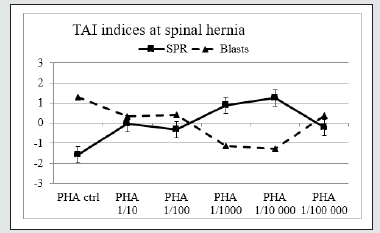
Figure 2: Standardized indices of SPR of blood cells in comparison with the number of lymphoblasts (in%) cultured using different dilutions of verapamil - hydrochloride for malignant gliomas (in the RBTL test).
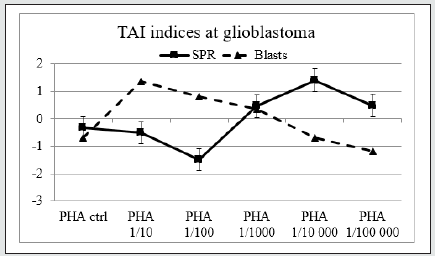
Figure 3: Inverse correlation of blood cells aggregation level indicators (SPR) and the number of Mid cells (the correlation coefficient is - 0.51) in patients with glioblastomas.
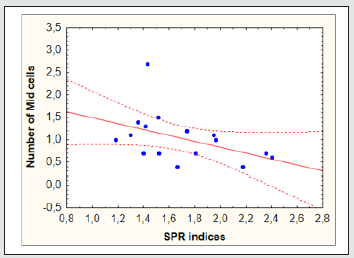
Comparison of the level of cell aggregation (increase in SPR indicators) using the Plasmon biosensor-analyzer and the number of Mid cells containing monocytes in their composition made it possible to find a negative correlation between them when examining blood samples in 16 patients with glioblastomas before surgery (the correlation coefficient is - 0.51). The data obtained may indicate a regulatory value of the transmembrane potential of peripheral blood cells, mediated through the level of aggregation of blood cells, measured in terms of SPR, on the number of potentially stem cells of lymphoblasts, formed in cell culture under the influence of phytohemagglutinin, and monocytes, measured in the pool of Mid cells in the blood of patients with glioblastomas. The revealed negative correlation shows that with a decrease in the transmembrane potential on the cell membrane, the number of monocytes, which are potential stem cells, increases. These data are confirmed by the presence of the mechanism of epithelial-mesenchymal transition (EMT) [11-13], which promotes the beginning of damaged organ tissues restoration, provided that the manifestations of the inflammatory process are inhibited, the presence of which will adversely affect these processes in patients with malignant tumors [14] (Figure 3).
In addition, the lack of correlation between the indices of the monocytes number and lymphocytes indicates differences in the protective and regenerative functions of these cell pools in the peripheral bloodstream (Table 2). At the same time, the rest of the cellular species have a positive correlation coefficient with each other. A long-term decrease in the transmembrane potential can contribute to the dysfunction of mesenchymal stem cells - monocytes, which will further manifest itself in pathological changes in the repair-regenerative relationship, leading to the appearance of recurrent tumor growth both in patients with glioblastomas and in other malignant tumors. The results obtained indicate the important role of the TMP level regulation in the adjuvant treatment of patients with glioblastomas.
Table 2: Lack of correlation when comparing the number of lymphocytes and Mid cells (monocytes) in patients with glioblastomas.
Conclusion
The presence of two mechanisms, apoptosis and epithelialmesenchymal transition (EMT), is vital for the normal implementation of the repair and regeneration processes in living organisms. In this case, the inflammatory process is absent in the embryonic period, when apoptosis predominates, so that embryonic cells are not damaged by various phlogogenic factors that arise during inflammation. The presence of these factors is also undesirable during the regeneration of organs and tissues by stem cells of various origins in the adult period, which is carried out by blocking the inflammation of the EMT. In malignant brain tumors, blocking of tumor-associated inflammation [14-19] does not occur due to the constant presence of necrotic tissues in the tumor focus. As a result, stem cells are damaged and cannot perform their regenerative functions normally [20-23]. Instead of restoring the cytoarchitectonics inherent in this tissue, a chaotic increase in cell mass occurs in the form of a malignant neoplasm. At the same time, the number of blood cells and their relationship between different fractions differ from those in the norm and can serve as indicators of tumor progression.
The work shows on two cell fractions with stem potential, namely on lymphocytes and monocytes, that with a decrease in the level of transmembrane potential, mediated by the level of aggregation of blood cells, the number of lymphoblasts in the cell culture and monoblasts in the peripheral blood increases, indicating a negative correlation between the membrane charge and number of stem cells. The dependence of many indicators on the level of transmembrane potential in the pathogenesis of tumor progression indicates that the correlation of TMP can be very effective in postoperative treatment, since the simultaneous correlation of other indicators regulated by the level of TMP will help prevent the early onset of relapses in patients with glioblastomas.
References
- Aum DJ, Kim DH, Beaumont TL, Leuthardt EC, Dunn GP, et al. (2014) Molecular and cellular heterogeneity: the hallmark of glioblastoma. Neurosurg Focus 37: 11.
- Han Sh, Liu Ya, Li Qi, Li Zh, Hou H, et al. (2015) Pre-treatment neutrophil-to-lymphocyte ratio is associated with neutrophil and T-cell infiltration and predicts clinical outcome in patients with glioblastoma. Cancer 15: 617.
- James CD, Collins VP (1993) Glial tumors, Genetic of nervous system tumors. 240-248.
- Duesberg P, Rausch C, Rasnick D, Haehlmann R (1998) Genetic instability of cancer cells is proportional to their degree of aneuploidy. Proc Natl Acad Sci 95(23): 13692-13697.
- Shvachko LP (2010) Premature Separation of Centromers in the early Mechanism of Aneuploidy During Oncological Progression Topics in Experimental Evolution of Organisms. Collection of Science Practices (9): 471-475.
- Gu L, Li H, Chen L (2016) Prognostic role of lymphocyte to monocyte ratio for patients with cancer: Evidence from a systemic review and meta-analysis. Oncotarget 7(22): 31926-31942.
- Zadora P, Dabrowski W, Czarko K (2015) Preoperative neutrophil-lymphocyte count ratio helps predict the grade of glial tumor-a pilot study. Neurol Neurochir Pol 49(1): 41-44.
- Zheng SH, Huang JL, Chen M (2017) Diagnostic value of preoperative inflammatory markers in patients with glioma: A multicenter cohort study. J Neurosurg 129(3): 583-592.
- Kemerdere R, Akgun MY, Toklu S, Alizada O, Tanriverdi T (2019) Preoperative systemic inflammatory markers in low- and high-grade gliomas: A retrospective analysis of 171 patients. Helion 5(5): 1681.
- Simara P, Tesarova L, Rehakova D, Farkasa S (2018) Reprogramming of Adult Peripheral Blood Cells into Human Induced Pluripotent Stem Cells as a Safe and Accessible Source of Endothelial Cells. Stem Cells Dev 7 (1): 10-22.
- Zao Y, Glesne D, Huberman E (2003) A human peripheral blood monocyte-derived subsets as pluripotent stemj cells. PNAS of the USA 100(5): 2426-243.
- Paxton S, Peckham M, Knibbs A (2018) The Leeds Histology Guide.
- Gridina Nya (2013) Utilizing SPR as a Novel Technique to Measure Cell Aggregation for Ketamine Treated Brain Gliomas. Cancer and Oncology Research 1(1): 1-5.
- Thiery JP (2002) Epithelial-mesenchymal transitions in tumour progression. Nature Reviews Cancer 2(6): 442-454.
- Gavert N and Ben Zeev A (2008) Epithelial-mesenchymal transition and the invasive potential of tumors. Trends in Molecular Medicine 14(5): 199-209.
- Mani SA (2008) The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell 133(4): 704-715.
- Tanno T and Matsui W (2011) Development and Maintenance of Cancer Stem Cells under Chronic Inflammation. Journal of Nippon Medical School 78(3): 138-145.
- Luchnik AN (2000) А common link in the mechanism of self-maintenance of malignant growth: The syndrome of the nonhealing wound. Ontogenesis 3(3): 227-231.
- Multhoff G (2012) Chronic inflammation in cancer development. Frontiers in Immunology 2: 98.
- Blaylock RL (2015) Cancer microenvironment, inflammation and cancer stem cells: A hypothesis for a paradigm change and new targets in cancer control. Surgical Neurology International 6: 92.
- Schwarzburd PM (2006) Chronic inflammation increases risk of epithelial neoplasia by inducing precancerous microenvironment: An evaluation of pathways of dysregulation. Problems in Оncology 52(2): 137-144.
- Mantovani A (2008) Cancer-related inflammation. Nature 7203: 436-444.
- Whiteside TL (2008) The tumor microenvironment and its role in promoting tumor growth. Oncogene 27(45): 5904-5912.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...