Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-6921
Research Article(ISSN: 2641-6921) 
Application of Biodegradable PLGA-PEG-PLGA/CPC Composite Bone Cement in the Treatment of Osteoporosis Volume 4 - Issue 2
Chao Guo, Dongyang Niu, Jia Liu, Xiaogang Bao and Guohua Xu*
- Department of Orthopedic Surgery, Spine Center, Changzheng Hospital, Second Military Medical, University, China
Received:March 29, 2021; Published: June 07, 2021
*Corresponding author: Guohua Xu, Department of Orthopedic Surgery, Spine Center, Changzheng Hospital, Second Military Medical University, Shanghai 200003, China
DOI: 10.32474/MAMS.2021.04.000184
Abstract
Objective: To evaluate the biological activity, safety and effectiveness of poly (lactic acid), poly (glycolic acid) and poly (ethylene glycol) / calcium phosphate cement (PLGA-PEG-PLGA/CPC) in vivo and in vitro.
Methods: The PLGA-PEG-PLGA/CPC composite bone cement was used to interact with MC3T3-E1 mouse osteoblasts in vitro, and the in vitro compatibility of the bone cement was tested by CCK8 experiment. Alizarin red staining and alkaline phosphatase activity were used Detect the osteogenic properties of the bone cement. Twenty healthy female New Zealand rabbits were selected for the establishment of ovariectomized osteoporosis model, and imaging and histomorphology were used to evaluate.10 rabbits used 30wt.% PLGA-PEG-PLGA/CPC composite bone cement with good physical and chemical properties and in vitro activity to be implanted into the lumbar vertebral body as the experimental group, and 10 rabbits used polymethyl methacrylate (PMMA) bone cement as the experimental group. Control group. The imaging and histomorphological results of the vertebral body after 12w of implantation were studied. Micro CT examination and hematoxylin-eosin (HE) staining were used to observe the distribution of bone cement, bone cement degradation and regeneration Bone tissue.
Results: In vitro biological activity evaluation: CCK-8 colorimetric method was used to detect cell proliferation. The results showed that the primary osteoblasts proliferated significantly in the PLGA-PEG-PLGA/CPC composite bone cement extract, with clear osteoinductive properties and promotion of osteoblasts The function of cell proliferation. Animal experiment evaluation: The results of the rabbit PVP experiment found that 30wt.% PLGA-PEG-PLGA/CPC composite bone cement has good operability and can completely fill the defect site. Postoperative Micro-CT and histological examination showed that the composite bone cement material was evenly distributed in the vertebral body, and a small amount penetrated into the trabecular bone to achieve a sufficient filling effect. After 12w, a small amount of CPC degradation and absorption and the formation of surrounding new bone matrix can be seen, and the formation of callus around the vertebral body is obvious.
Conclusion: PLGA-PEG-PLGA/CPC composite bone cement has the biological activity of promoting the proliferation of osteoblasts. Through animal PVP experiments, 30wt.% PLGA-PEG-PLGA/CPC composite bone cement has good maneuverability, and its good biodegradability and osteoinductive effect contribute to the formation of surrounding new bone trabeculae.
Introduction
With the advent of an aging society, osteoporosis has gradually become the fourth most common chronic disease in the world. Severe osteoporotic low back pain and osteoporosis-related vertebral fractures (OVCF) have become global diseases that affect the lives and health of the elderly. Percutaneous vertebroplasty, including percutaneous vertebroplasty (PVP) and percutaneous balloon dilatation (PKP), is currently one of the main treatments for elderly osteoporotic low back pain and OVCF [1, 2] and produced a good short-term therapeutic effect. Regardless of PVP or PKP technology, filling materials are one of the core contents of the treatment. At present, the bone cement for vertebral body strengthening is mainly made of polymethyl methacrylate (PMMA) material, and there is no special bone cement for osteoporotic spine in clinical application. The development of special bone cement for vertebral body shaping has become a hot and focus of domestic and foreign research [3]. In addition to polymer medical materials for filling materials, biomedical inorganic materials have also received more and more attention in recent years. Among them, biodegradable and biologically active inorganic bone cement materials have gradually attracted attention [4, 5]. This type of inorganic degradable bone cement provides a scaffold for the growth of new bone, and gradually degrades in the body, and has good osteoconductivity and biological characteristics. Capacitive, so it has great potential in spinal vertebroplasty. Calcium phosphate cement (CPC) is one of the self-setting materials. Because of its good biodegradability, biocompatibility and osteoconductivity, CPC has broad application prospects in PVP filling materials. However, the clinical application of CPC in the weight-bearing bones of the spine has many bottlenecks, such as low compressive strength, poor anticollapse, and poor injection performance. Therefore, the current application of CPC in spinal repair requires further research [6-8].
According to the problems of the above-mentioned bone cement materials, and in view of the biomechanical characteristics of osteoporotic spine vertebrae, our laboratory synthesized a new type of biodegradable composite bone cement system, namely PLGA-PEG-PLGA/CPC. The material is compounded by the ratio of α-TCP, CaCO3 and CaHPO4 to form a composite CPC system (α-TCPMCPM- CC system), focusing on solving the problems of inorganic bone cement setting time, compressive strength, and acid-base balance. At the same time, further use of the poly (lactic acid), poly (glycolic acid) and poly (ethylene glycol) (PLGA-PEG-PLGA) triblock polymer temperature-sensitive hydrogel that has been used in clinical applications is liquid-solid phase transition and high temperature under different temperature conditions. Molecular polymer can improve the adhesiveness of bone cement, and it is mixed with NaH2PO4 in proportion to replace the traditional inorganic liquid phase of bone cement. Quickly mixed with the composite CPC system to form a PLGA-PEG-PLGA/CPC bone cement system, which solves the problem of CPC in the injection process It is easy to produce the filter pressure effect and cause the solid-liquid separation phenomenon and being easily diluted by the blood of the cancellous bone, so that the filling material has the effects of strong compressive strength, high ductility, good injection performance, and strong water resistance, and finally this system is transformed into the hydroxyapatite component of biological bone. This makes it more in line with the requirements of spinal repair and PVP operation and provides a theoretical and experimental basis for the development of special bone cement for spinal repair. This article aims to detect the in vitro biological activity of the bone cement of the system and animal experimental studies, and evaluate its biological activity, safety, and effectiveness in vivo and in vitro [9,10].
Methods and Materials
In Vitro Cell Compatibility Evaluation
Culture MC3T3-E1 (mouse osteoblast) cells, use CPC bone cement column and various proportions of PLGA-PEG-PLGA/CPC composite bone cement (10wt.%, 20wt.%, 30wt.%, 40wt.% PLGAPEG) -PLGA/CPC) After the column is processed, use the CCK8 kit to detect. the relative growth rate (RGR) of the cells can be calculated based on the OD value: RGR = (OD value of the experimental group/ OD value of the blank control group) ×100 %; When RGR>75%, the cell compatibility of the material is good; when RGR>100%, the material is considered to promote cell proliferation.
Alizarin Red Staining and Quantitative Detection
Take 2 parallel samples for each ratio of PLGA-PEG-PLGA/ CPC composite bone cement column (for example, as mentioned above), cut into powder and sterilize the mixed culture liquid at a concentration of 10 mg/ml. The stem cells were seeded in a 24-well plate. After 24 hours, the old culture medium was removed, and 0.5 ml of osteogenic induction medium was added. Induction for 7-14 days. Fix for 15 min with 4% paraformaldehyde. Stain with Alizarin Red staining solution for 3 min, observe under microscope and take pictures. Subsequently, hexadecyl chloride was added and left at room temperature for 30 minutes, the supernatant was drawn, and the absorbance of the sample was measured at 560 nm using a microplate reader, and the absorbance of the supernatant of a group of simple cells was measured at the same time. The measured value of the sample = the absorbance value of the sample-the absorbance value of the simple cell group.
Quantitative Detection of Alkaline Phosphatase (Alp) Activity
The grouping and culture are as described above, the cells are lysed, the supernatant is taken, and the alkaline phosphatase kit is tested. The absorbance of each sample is repeated 3 times and the average is taken.
Rabbit Model of Osteoporosis
The classic method of ovariectomy to induce osteoporosis reported in the literature 9, 10. 20 New Zealand rabbits, take a 3 cm midline incision in the abdomen (approximately 3~4 cm from the upper edge of the lowest nipple as the midpoint) into the abdominal cavity, ligate the fallopian tubes and remove the ovaries.
Rabbit Vertebroplasty Model
The 20 experimental rabbits of the pre-osteoporosis model were divided into two groups A and B (10 rabbits in each group, weight 2.5~3.0 kg, each group was half male and female). Group A was the experimental group (PLGA-PEG-PLGA) /CPC composite bone cement), group B is the control group (PMMA bone cement). Using the bilateral iliac bones corresponding to the upper edge of the lumbar 7 vertebral body as a mark, locate the spinous processes and kyphotic processes of the L5 and L6 vertebral bodies, centering on the upper articular processes of L5 and L6, make a longitudinal incision about 4 along the line of the two articular processes ~6 cm straight incision, exposing the upper articular process and mastoid process of the spine, and exploring the transverse process. Continue to separate from the junction of the transverse process and the base of the vertebral body to the head side, exposing the vertebral accessory process, and its tail is the intervertebral foramen. Use the intersection of the vertical line of the midpoint of the spine mastoid and the horizontal line of the lower edge of the spine as the puncture point. Use a manual electric drill to gradually break through the cortex, and then gradually penetrate the vertebral body. the four walls are probed with a probe to make sure that the four walls of the needle track are intact without breaking through the surrounding bone cortex, and then the 2~3 mm bone tissue puncture needle is used to expand the channel. Probe the integrity of the four walls and then perform bone cement injection. At 12w after operation, rabbits in each group were sacrificed and the experimental vertebral body segments were removed for imaging and histomorphology.
Statistics
Use SPSS (IBM version 21) statistical software for data processing. The quantity data of the normal distribution meter is expressed as X ̅±s, and the related data of D1~D5 continuous normal distribution is compared with one-way analysis of variance (Duncan method) to analyze the significance of differences between multiple groups of samples, p<0.05 indicates that the difference is statistically significant.
Results
PLGA-PEG-PLGA/CPC Composite Bone Cement Has the Function Of Significantly Promoting The Proliferation Of Osteoblasts And Osteoinductive Properties
Figure 1: PLGA-PEG-PLGA/CPC composite bone cement has the function of significantly promoting the proliferation of osteoblasts and osteoinductive properties.
(A) Cytocompatibility of PLGA-PEG-PLGA/CPC Bone Cement.
(B) Relative growth rate of each proportion at different time. Alizarin red staining results of various proportions in culture for 7d.
(C) and 14d.
(D). [ A-E are 0wt.%, 10wt.%, 20wt.%, 30wt.%, 40wt.% PLGA-PEG-PLGA/CPC;a-e are the microscope images of A-E in sequence.].
(E) Quantitative results of Alizarin Red staining in each group.
(F) ALP activity quantitative results.
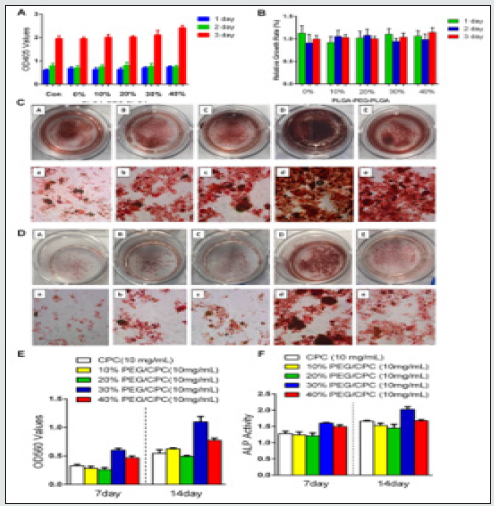
The cell proliferation activity was detected by CCK-8 colorimetry, the results showed that the cell proliferation in each group was good, the cell proliferation ability of PLGA-PEG-PLGA/ CPC composite bone cement group was slightly better than that of CPC composite bone cement group alone, and the cell proliferation activity reached the maximum on the third day with the increase of PLGA-PEG-PLGA content. PLGA-PEG-PLGA polymer itself has good biocompatibility and biodegradability and contains many hydroxyl groups in the molecule. The presence of hydroxyl groups can increase the hydrophilicity and cell adsorption of CPC, thereby proliferating osteoblasts on its surface. Create better conditions (Figure 1A). To further compare the cell proliferation of each group, the concept of relative growth rate was introduced. Through statistical analysis, the relative growth rate of cells in each proportion of composite bone cement was above 90%, (Figure 1B). The cell growth rate of 40wt.% PLGA-PEG-PLGA/CPC on the third day is comparable to that of CPC bone cement alone. The relative growth rate of cement is significantly different (p<0.05).
The results of alizarin red staining showed that the staining degree of each group increased gradually with the passage of time. (Figure 1C & 1D). After 7 days, the staining degree of Alizarin Red in the 10wt.% and 20wt.% PLGA-PEG-PLGA/CPC groups was not significantly different from that of CPC bone cement alone, but both groups showed an increase in the level of staining over time. The staining was in the mirror at 14 days. The formation of calcified nodules in the two groups of 10wt.% and 20wt.% PLGAPEG- PLGA/CPC can be observed, showing a darker red color. The staining degree of 30wt.% and 40wt.% PLGA-PEG-PLGA/CPC was significantly increased on the 7th day compared with the CPC bone cement group alone. After 14 days, the 30wt.% group can be macroscopically observed a significant difference, suggesting that Alizarin Red and cytoplasm The calcium ions combine to form many red calcium nodules. The quantitative results (Figure 1E) showed that the absorbance of each group gradually increased over time. After 7 and 14 days, the PLGA-PEG-PLGA/CPC of each group was higher than that of the CPC group, especially the 30w. % and 40w. % PLGA-PEG-PLGA/CPC increased significantly compared with that of the CPC group, and the difference was statistically significant (p<0.05). Therefore, as the content of PLGA-PEG-PLGA increases, the absorbance value of alizarin red staining gradually increases first and then gradually decreases. The activity of 30wt.% PLGA-PEG-PLGA/CPC is the strongest. With the passage of time, the cell ALP activity change trend in each group of materials (Figure 1F), the results found that after 7 days and 14 days, 10wt.% and 20wt.% PLGA-PEG-PLGA content of bone cement ALP activity was lower than that in the CPC group. When the content of PLGA-PEGPLGA increased to 30%, the ALP activity on the 7th day (1.61±0.08) and the ALP activity on the 14th day (2.03±0.12) were significantly higher than that of the simple CPC group (1.28± 0.10, 1.66±0.03), there is a statistical difference (p<0.05), and 30wt.% PLGA-PEGPLGA/ CPC has the strongest activity. It indicates that the PLGA-PEGPLGA/ CPC composite bone cement has the function of significantly promoting the proliferation of osteoblasts and the osteoinductive properties.
Postoperative Imaging Examination of PLGA-PEGPLGA/ CPC Composite Bone Cement in The Treatment of Osteoporosis With PVP In Rabbits
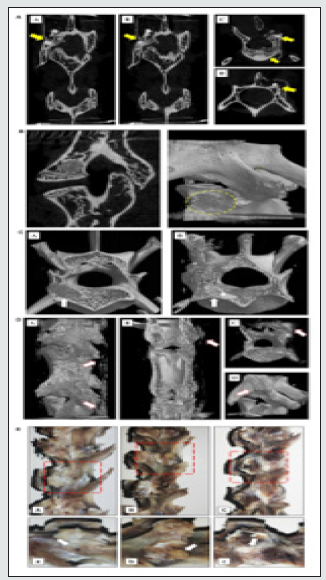
12w after PVP, Mirco-CT of rabbit experimental specimens in group A showed that the bone cement was partially absorbed, and the bone cement was tightly combined with the new bone trabecula. There were dense trabecular bones in the vertebral body around the bone cement, and bone cement vertebral body was implanted Many calluses were formed nearby (Figures 2A). The experimental specimens of the rabbits in group B showed that the bone cement was not absorbed and was fully wrapped by the surrounding bone trabeculae. There was bone hyperplasia near the vertebral body. There was no obvious new bone formation on the side of the vertebral body implantation. The bone cement density was quite different from the surrounding bone tissue (Figure 2B). Comparing the three-dimensional reconstruction images of the vertebral body after 12w between the two experimental groups, the bone composition of group A is more obvious than that of group B. Not only is the proliferation of bone tissue inside the vertebral body obvious, but also the irregular callus formation on the side of the vertebral body is more obvious (Figures 2C & 2D). The general picture shows (Figure 2E) that there is still exposed bone cement in the PMMA group, and no obvious bone formation around it; while in the PLGA-PEG-PLGA/CPC group, there is no bone cement around the puncture point, and there is no bone formation around the vertebral body, obviously.
Figure 2: Postoperative imaging examination of PLGA-PEG-PLGA/CPC composite bone cement in the treatment of osteoporosis in rabbit vertebroplasty.
(A) Results of the vertebral body and mirco-CT of the PLGA-PEG-PLGA/CPC group 12 weeks after surgery. The distribution and location of the implanted material in the vertebral body (A/B coronal plane; C/D level), yellow arrows indicate implant material, and C/D shows surrounding callus formation.
(B) Results of the vertebral body and mirco-CT of PMMA implantation material 12 weeks after surgery The distribution and location of the implantation material in the vertebral body (Exposed PMMA can be seen around the vertebral body, without obvious callus formation)( A: sagittal plane; B: Three-dimensional reconstruction).
(C) Comparison of perivertebral osteogenesis between the PMMA group and the PLGA-PEG-PLGA/CPC group at 12 weeks postoperatively indicates the arrow of bone cement implantation. (A was the PMMA group, and the density difference between the implant material and the surrounding was great; B was the PLGA-PEG-PLGA/CPC group, and the density difference between the implant material and the cancellous bone was small. The osteogenesis in and out of the vertebral body was obvious, and the surrounding bone callus was formed).
(D) Comparison of bone callus around vertebral body 12 weeks after PMMA bone cement was made between PLGA-PEGPLGA/ CPC group A and group B. (A-C group A PLGA-PEG-PLGA/CPC bone cement group, obvious vertebral osteogenesis and irregular callus formation around the vertebral body, D group B PMMA bone cement group, no obvious osteogenesis around the vertebral body, no obvious callus formation).
(E) The lateral profile of the vertebrae of the blank control group, PMMA group and PLGA-PEG-PLGA/CPC group were compared 12 weeks after surgery. (A: blank control group, B: PMMA group, C: PLGA-PEG-PLGA/CPC group; Figure A, B and C: enlarged view of the red area in Figure A, B and C. The puncture hole indicated by arrow A has healed without obvious callus formation around it. B The arrow indicates exposed PMMA bone cement with no apparent osteogenesis around it; Arrow C indicates the surrounding callus, where osteogenesis is evident around the puncture site.)
PLGA-PEG-PLGA/CPC Composite Bone Cement Promotes the Formation of New Bone Trabeculae in Rabbits with Osteoporosis
Tissue sections after 12w (Figures 3A & 3B) showed that the PLGA-PEG-PLGA/CPC group had obvious formation of new bone matrix around the implanted material, bone trabecula was reconstructed, osteoblasts were active, and bone formation The phenomenon was obvious, while the bone cement in the PMMA group showed unabsorbed implant material, the surrounding bone trabecula still had signs of destruction and had not been reconstructed, and there was no obvious new bone matrix around.
Figure 3: PLGA-PEG-PLGA/CPC composite bone cement promotes the formation of new bone trabeculae in rabbits with osteoporosis.
(A) 12-week tissue section of PMMA group. [A shows the macrophages surrounding the implanted material with obvious foreign body reaction; the arrow in B shows the damaged trabecular bone tissue, with no reconstruction or new bone matrix.]. (B) Tissue sections of PLGA-PEG-PLGA/CPC group at 12w. [The white arrow in A picture shows the formation of new bone matrix around the original bone trabecula, vascular tissue can be seen in it, and the red arrow shows osteoblasts; the white arrow in picture B is the callus around the cortical bone of the vertebral body, and the new bone matrix is visible inside, red the arrow is the active osteoblast.]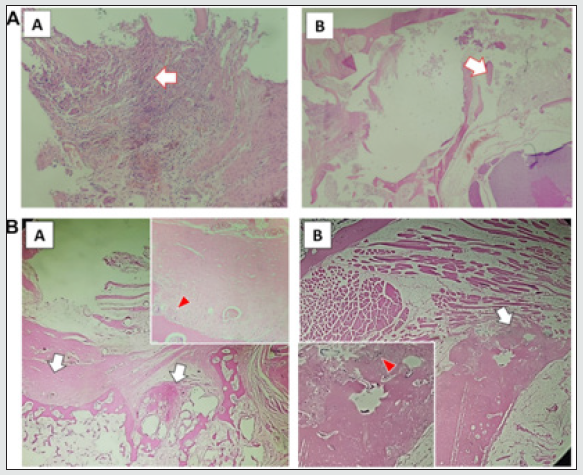
Discussion
With the gradual research and development of self-curing CPC, the clinical application potential of injectable CPC artificial bone products has gradually attracted attention [11]. It has certain properties such as biodegradability, good biocompatibility [12], and bone conduction. In the internal environment, it can also be mixed with blood, tissue fluid, etc. to undergo a hydration reaction and transform into the mineral phase of bone [6,13]. Among them, most of CPC bone cement products have achieved good clinical effects and are still being improved and continuously expanded in clinical applications [14-16]. Bone cement used in the human body must have good biocompatibility. Biocompatibility is defined as a material that causes an appropriate reaction in a specific part of the body. Good biocompatibility is not only conducive to the repair and balance of biological tissues, but also conducive to the effectiveness of implant materials. Through in vitro experiments, we have proved that PLGA-PEG-PLGA/CPC composite bone cement has good cell compatibility, no toxic side effects, and the PLGA-PEGPLGA polymer molecule contains many hydroxyl groups, which may increase CPC hydrophilicity and cell adsorption sex, which creates better conditions for osteoblasts to proliferate on their surface. Current studies believe that bio-substitution materials will excessively cause an increase in the reactive oxygen species (ROS) of osteoblasts around the material, thereby inhibiting the activity of osteoblasts, which is not conducive to the repair process of surrounding bone.
The PLGA-PEG-PLGA hydrogel not only has physical and chemical properties like the human body environment, but also has a certain role in scavenging oxygen free radicals and has a certain promotion effect on surrounding bone formation. Experiments have shown that the addition of PLGA-PEG-PLGA polymerization It can not only avoid the excessive increase of intracellular ROS, but also reduce the degree of oxidative damage of surrounding cells to a certain extent and promote the survival rate of cells17. As the temperature-sensitive hydrogel degrades, the pore structure formed is conducive to the expansion and proliferation of osteoblasts. Our results show that in the PLGA-PEG-PLGA/CPC composite bone cement, the addition of PLGA-PEG-PLGA polymer does not affect the osteogenic differentiation ability of MC3T3-E1, but at a certain concentration, it will significantly increase the material itself Osteogenic performance, considering that the addition of polymer increases the surface electronegativity of the CPC material, it is more conducive to the adhesion and proliferation of MC3T3-E1 cells on the CPC material. Therefore, the composite PLGA-PEG-PLGA copolymer and CPC have good biological activity, and osteoblasts can show adhesion and expansion, grow well, and have good osteoconductivity.
From the results of imaging examination, PLGA-PEG-PLGA/ CPC composite bone cement has good biocompatibility and osteoconductivity, which is mainly related to the clear osteoinductive effect of CPC [17,18]. After the introduction of temperaturesensitive hydrogel, the degradation rate of composite bone cement is faster than previous research results, which is like previous research results [19,20]. CPC materials are mainly biodegraded in two ways, one is passive absorption by chemical dissolution, and the other is active absorption process mediated by cells [14, 15]. However, the degradation rate of simple CPC is relatively slow, which can range from several months to several years, and a relatively large amount of filling material cannot even be completely degraded, which is not conducive to the formation of new bone in the vertebral body. Klein et al. found that CPC material as a filler for PVP surgery will gradually degrade and absorb over time, and that CPC material that leaks out of the bone will almost completely degrade and absorb in about 2 years [16]. The introduction of PLGA-PEG-PLGA temperature-sensitive hydrogel can accelerate the degradation of the composite bone cement, and the degradation rate can be controlled by adjusting the content of the hydrogel. The experiment showed degradation of a small amount of implanted PLGA-PEG-PLGA/CPC composite bone cement at 12w. This is like the results of previous studies. Felix et al. compounded the rapid pore-forming polylactic acid-glycolic acid copolymer and CPC material. The biodegradation rate of bone cement is 55% higher than that of the CPC control group [19,20]. Over time, the vertebral body defect in the experimental group was filled with composite bone cement, and there was a small amount of bone cement inside the trabecular bone structure. The CPC component in the bone cement has osteoinductive properties, which is beneficial to the regeneration of trabecular bone. Further growth [18,21]. Through bone conduction, new bone is formed and connected to the CPC, thereby increasing the strength of the vertebral body as a whole. PMMA organic polymer materials cannot be fused with autologous bone, and PMMA lacks biological activity, and the elastic modulus does not match with autologous bone. For example, it has been reported in the literature that PMMA bone cement is filled with peripheral osteonecrosis, re-fracture of adjacent vertebrae, and material toxicity. disease. The PLGA-PEG-PLGA/CPC composite bone cement has suitable biomechanical strength. Although the early strength is not as good as the PMMA material, it is conducive to the regeneration of trabecular bone in the vertebral body and the overall vertebral body is resistant to compression over time. The intensity continues to increase. Therefore, the composite bone cement has potential application prospects in spine bone repair.
In summary, we found that PLGA-PEG-PLGA/CPC composite bone cement maintains the biological activity of calciumphosphorus- based bone cement to induce mineralization and promote osteoblast proliferation. Through animal PVP experiments, 30wt.% PLGA-PEG-PLGA/CPC composite bone cement has good maneuverability, and its good biodegradability and osteoinductive effect contribute to the formation of surrounding new bone trabeculae. Therefore, this study provides a promising bone repair material for the treatment of osteoporosis. Small animal experiments have further verified the biological properties of the material and provided a preliminary experimental basis for clinical application. But at the same time, we should conduct in vivo experiments on large animals (such as pigs and sheep) that are closer to the structure of the human body to study the biocompatibility, degradability and osteogenic properties of the composite bone cement in the body, and further study it’s in the vertebral body The effect and mechanism of internal osteogenesis, angiogenesis and local anti-osteoporosis, and through relevant biomechanical tests, it is clear that the composite material has clinical value in the treatment of osteoporotic vertebral fractures and traumatic vertebral fractures. The new generation of selfcuring materials do a good job in basic research.
Acknowledgement
Not applicable
Conflict of Interests
All authors declare that they have no conflict of interests.
References
- Clark W, Bird P, Gonski P, Terrence H Diamond, Peter Smerdely et al. (2016) Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet 388(10052): 1408-1416.
- Bouza C, López-Cuadrado T, Almendro N, Amate JM (2015) Safety of balloon kyphoplasty in the treatment of osteoporotic vertebral compression fractures in Europe: a meta-analysis of randomized controlled trials. Eur Spine J 24(4): 715-723.
- He Z, Zhai Q, Hu M, Chengbin Cao, Jihui Wang, et al. (2014) Bone cements for percutaneous vertebroplasty and balloon kyphoplasty: Current status and future developments. J Orthop Translat 3(1): 1-11.
- Beig B, Liaqat U, Douna I (2020) Current Challenges and Innovative Developments in Hydroxyapatite-Based Coatings on Metallic Materials for Bone Implantation: A Review. Coatings 10: 1249.
- Chen JS (2019) Characterization of Sol-Gel Derived Calcium Hydroxyapatite Coatings Fabricated on Patterned Rough Stainless-Steel Surface. Coatings 9(5): 334.
- O'Neill R, McCarthy HO, Montufar EB, Ginebra MP, Wilson DI, et al. (2017) Critical review: Injectability of calcium phosphate pastes and cements. Acta Biomater 50: 1-19.
- Burguera EF, Xu HH, Sun L (2008) Injectable calcium phosphate cement: effects of powder-to-liquid ratio and needle size. J Biomed Mater Res B Appl Biomater 84(2): 93-502.
- Montufar EB, Maazouz Y, Ginebra MP (2012) Relevance of the setting reaction to the injectability of tricalcium phosphate pastes. Acta Biomater 9(4): 6188-6198.
- Kotak DJ, Devarajan PV (2020) Bone targeted delivery of salmon calcitonin hydroxyapatite nanoparticles for sublingual osteoporosis therapy (SLOT). Nanomedicine 24: 102153.
- Luo E, Hu J, Bao C, Yunfeng Li, Qisheng Tu, et al. (2012) Sustained release of adiponectin improves osteogenesis around hydroxyapatite implants by suppressing osteoclast activity in ovariectomized rabbits. Acta Biomater 8(2): 734-743.
- Dorozhkin SV (2008) Calcium orthophosphate cements for biomedical application. Journal of Materials Science 43(9): 3028.
- Lakouraj MM, Alipour A, Najafiroudbari M, Ojani R (2020) Fabrication of a Nanocomposite Based on Pectin/ Polyaniline/Graphene Oxide as Novel Electrically Conductive Biomaterial for Biosensing Detection of Hemoglobin. Modern Approaches on Material Science 2(5).
- Klein R, Tetzlaff R, Weiss C, Meike-Kristina Schäfer, Michael Tanner, et al. (2013) Osteointegration and Resorption of Intra-and Extravertebral Calcium Phosphate Cement. Journal of Spinal Disorders & Techniques 30(3).
- Sheikh Z, Abdallah MN, Hanafi AA, Misbahuddin S, Rashid H, et al. (2015) Mechanisms of in Vivo Degradation and Resorption of Calcium Phosphate Based Biomaterials. Materials (Basel) 8(11): 7913-7925.
- Gumpert R, Bodo K, Spuller E, Poglitsch T, Bindl R, et al. (2014) Demineralization after balloon kyphoplasty with calcium phosphate cement: a histological evaluation in ten patients. Eur Spine J 23(6): 1361-1368.
- Maestretti G, Sutter P, Monnard E, Peter Wahl, Henri Hoogewoud, et al. (2014) A prospective study of percutaneous balloon kyphoplasty with calcium phosphate cement in traumatic vertebral fractures: 10-year results. Eur Spine J 23(6): 1354-1360.
- Vojtova L, Michlovska L, Valova K, Zboncak M, Trunec M, et al. (2019) The Effect of the Thermosensitive Biodegradable PLGA⁻PEG⁻PLGA Copolymer on the Rheological, Structural and Mechanical Properties of Thixotropic Self-Hardening Tricalcium Phosphate Cement. Int J Mol Sci 20(2):391.
- Albee FH (1920) Studies in Bone Growth: Triple Calcium Phosphate As A Stimulus To Osteogenesis. Ann Surg 71(1): 32-39.
- Félix Lanao RP, Sariibrahimoglu K, Wang H, Wolke JG, Jansen JA, et al. (2014) Accelerated calcium phosphate cement degradation due to incorporation of glucono-delta-lactone microparticles. Tissue Eng Part A 20(1-2): 378-388.
- Félix Lanao RP, Leeuwenburgh SC, Wolke JG, Jansen JA (2011) In vitro degradation rate of apatitic calcium phosphate cement with incorporated PLGA microspheres. Acta Biomater 7(9): 3459-3468.
- Palmer I, Nelson J, Schatton W, Dunne NJ, Buchanan FJ, et al. (2016) Biocompatibility of calcium phosphate bone cement with optimized mechanical properties. J Biomed Mater Res B Appl Biomater 104(2): 308-315.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




