Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-6070
Research Aticle(ISSN: 2638-6070) 
How Beneficial are Statins and PCSK9-Inhibitors?
Volume 2 - Issue 3Richard M Fleming1*, Matthew R Fleming1 and Tapan K Chaudhuri2
- 1FHHI-Omnific Imaging-Camelot, USA
- 2Eastern Virginia Medical School, USA
Received: September 23, 2019; Published: October 10, 2019
*Corresponding author: Richard M Fleming, PhD, MD, JD, FHHI-Omnific Imaging-Camelot El Segundo, Los Angeles, CA, USA
DOI: 10.32474/SJFN.2019.02.000136
Abstract
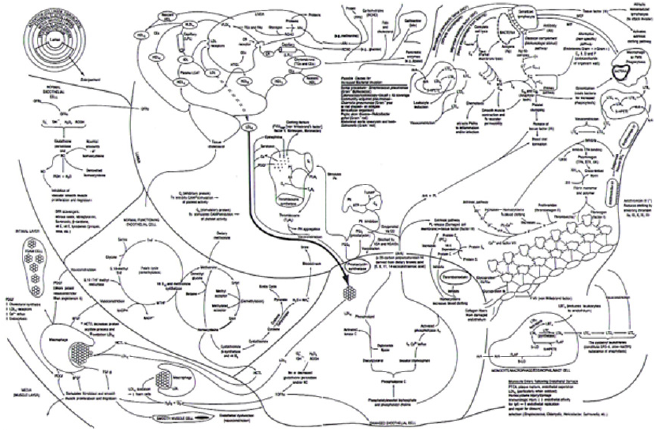
Everyday people take their cars into the mechanic to be worked on. Sometimes it’s for routine maintenance, other times it’s because a warning light has come on or something just doesn’t feel or sound right when the car is running. People frequently visit their doctors for the same reason. Either something just doesn’t feel right – perhaps an unusual ache or pain, sometimes that pain is in your chest - or one of your blood tests (warning lights) came back in an abnormal range. Your doctor will frequently run blood tests looking for a problem, much like the mechanic will check the oil in your engine. Except the auto mechanic shuts the car off to run his tests; something your doctor doesn’t have the luxury of doing. You can infer a lot by looking at the engine oil, or getting a blood test. But you can only infer something is going on. Neither the engine oil nor the blood test tells you what the problem actually is – only hopefully where to look for the answer to the problem When people get their cholesterol levels checked, it’s usually because they’re worried about their heart – even though cholesterol by itself doesn’t cause heart disease (Figure 1) – inflammation does. To begin with you should also know there is more than one type of cholesterol in your body.
The combination of these various types of cholesterol, when put together, are called your total cholesterol (TC). It’s the sum of your good (HDL) and bad (LDL) cholesterol, along with the fats (triglycerides) in your blood, which are either made in your liver (very low density lipoprotein cholesterol; VLDL) or consumed (fats and chylomicrons) by you in the foods you eat. Another type of cholesterol is called intermediate density lipoprotein cholesterol (IDL), because it is intermediate in density, compared with the other types, and when compared with the other types of cholesterol IDL is composed almost equally of cholesterol and fat.
TC = HDL + LDL + VLDL/5 + Chylomicrons + IDL
You probably already realize this, but you do need cholesterol for your body to work. You need cholesterol for your cells to grow and maintain themselves and you need cholesterol for hormones, for the lining of the axons of nerves in your body – including your brain. You really don’t need to worry about eating it because your liver is designed to make it. In fact, most people only absorb about 10% of the cholesterol they eat, which means for most people, they are absorbing somewhere between 25 and 50 mg each day from the food they eat. If you had to depend upon that, you would probably either die or become seriously ill. Fortunately you don’t need to depend upon what you absorb from the foods you eat, because your liver will make around 1000 mg each day – 20 to 40 times the amount you get from your diet – as long as you don’t have liver disease. One of the interesting characteristics of carnivores is that their livers don’t make cholesterol to meet their needs, so carnivores have to consume cholesterol from the foods they eat to survive.
All this begs the question, if we need cholesterol, why do so many doctors say cholesterol is bad for you? The answer is both simpler and much more complex (Figure 1), than many people think. Most foods that are high in cholesterol are also high in saturated fat and it is this saturated fat, once oxidized, which is a primary, although not only, cause of inflammation, within the walls of the arteries of the heart that produces coronary artery (CAD)/heart disease [1,2], angina and death.
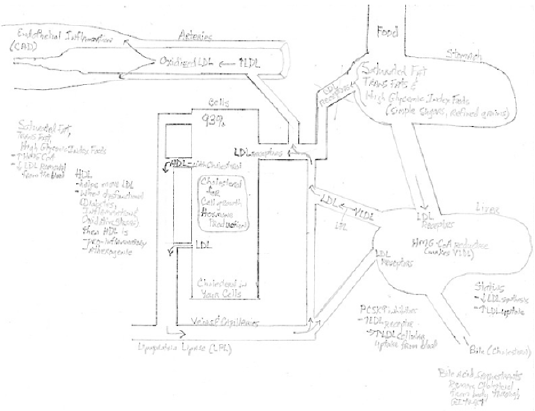
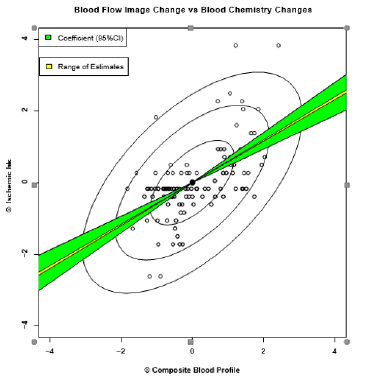
Increased dietary saturated fat intake not only increases the amount of cholesterol made by your liver, but it can also reduce the ability of cells in your body to remove the LDL cholesterol (Figures 1 & 3) from the blood, by interfering with the LDL receptors themselves–i.e., the part of your cells responsible for recognizing cholesterol and removing it from the blood for use by the body. Just like insulin receptors, which respond to increased levels of glucose (sugar) in the blood stream, so too do the LDL receptors, respond to increased levels of LDL cholesterol. However, there is no actual relationship between measured changes in blood tests like cholesterol and measured changes in CAD [3], when physiologically measured [4], as shown in (Figure 2) [2]. These changes cannot be measured using mere coronary arteriograms [5]-the basis for most if not all of the clinical data supporting the use of cholesterol lowering medicines - as coronary arteriograms neither measure the ability of the coronary arteries to respond to increased demand for coronary blood flow, nor the inflammation within the walls of the arteries themselves. This is an extremely important point and one that is frequently overlooked, given that up to 70% of all myocardial infarctions (heart attacks) occur in people whose arteries have less than 30% narrowing of the lumen – the area where the blood flows - and it is only this lumen narrowing, which coronary arteriograms can evaluate.
Figure 2: There is no correlation between changes in blood cholesterol and changes in coronary artery disease [3].
What types of foods raise your cholesterol levels?
While there are many studies which reveal that many different types of diets may initially show improvements in weight loss and blood cholesterol levels, most (not all) people would agree that there are three basic types of foods, which have been associated with increased cholesterol levels. These include:
a. Saturated Fat
b. Trans Fats, and
c. Highly refined, processed foods.
An increased consumption of any, or a combination of these, can be associated with increased cholesterol levels, increased insulin resistance, increased LDL receptor resistance, and increased weightobesity. Consequently resulting in heart disease, strokes, diabetes and a variety of other diseases. One of the common themes running through medicine and social media is the belief, that medicines can solve your problems or at least ameliorate them, thereby shifting the burden of responsibility. Something Big Pharma and Big Food are all too happy to accept, as this shift in responsibility results in profits for these corporations. Clearly you don’t solve what you put in your mouth by putting something else in your mouth–including medications or more of another type of food. You solve the problem by not putting the first problem in your mouth.
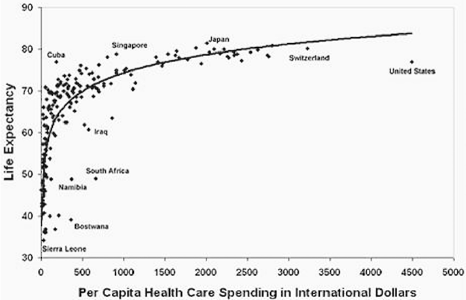
While the approach of putting more food or medications in your mouth is lucrative for Big Food and Big Pharma, it has been disastrous for everyone else. Let’s be very clear here-there has not been a shift in genetics in the last 100 years. Evolutionary mutations don’t work that way and such changes when they do occur, provide a survival benefit or they become extinguished. As Figure 4 shows [6], there is little, if any, survival benefit from this increased expenditure of healthcare monies being thrown at the problem and no appreciable increased life expectancy. One of, if not the, major health care expenditure currently confronting us, is the cost of prescription medications; with statins, PCSK9-inhibitors and diabetes medications leading the way. Before we address how these medications work, lets first look at the issue of cholesterol itself.
How much cholesterol is too much?
People unfortunately have a tendency to think of things in black and white, true false, right wrong - absolutes. For decades physicians have talked about levels of cholesterol that we want to keep your blood cholesterol below to reduce your risk of heart disease. The truth is that there is no absolute value, which is safe for everyone. What may be safe for you may kill someone else and vice-versa.
In the 1980’s and 1990’s, the first author was a member of the American Heart Association - Physician Cholesterol Education Faculty, and we used to tell people that total cholesterol levels should be kept below 150 milligrams/deciliter (mg/dl or %) or 3.879 mmol/l (millimole per liter) in standard international (SI) units. The use of this number was somewhat arbitrary as 50% (half) of all people who have heart attacks, have total cholesterol levels less than 150 mg/dl. At the same time, other people with higher cholesterol levels do not have heart attacks. There are a number of reasons for this including the differences in genetic handling of cholesterol levels, the other factors involved in the inflammatory process (Figure 1) and our sheer lack of real data about tissue levels of cholesterol and CAD where the real problem lies, versus blood levels of cholesterol and CAD.
The important take away point is that oxidized cholesterol builds up in the walls of the arteries of the heart and elsewhere, interfering with the ability of these arteries of the heart to do their job and the result, which isn’t measured by looking at the cholesterol in the blood, is a heart attack, stroke, loss of limb, etc. Cholesterol flowing through the blood stream without depositing is not actually causing an issue, at least not while flowing freely through the blood.
The cholesterol causing heart disease isn’t the cholesterol floating around in your blood stream to be sampled by your doctor
Only about 7% of your total BODY cholesterol is found in your BLOOD. The remaining 93%, which we don’t measure, is stored inside the cells of your body. Within the cells, the cholesterol is being used for cell growth, repair and to make hormones along with other substances needed by your body. It is also here where cholesterol is undergoing oxidation and participating in the inflammation within the walls of your arteries - where the real problem exists. When too much cholesterol is stored in the walls of your arteries, and oxidized, inflammation will occur (Figure 1) and these arteries will not be able to do their job. When that happens, you can have a heart attack, stroke, need kidney dialysis or lose a limb. It will just depend upon which artery is being damaged. The smaller the artery the sooner the damage is likely to occur and be noticed.
LDL receptor resistance is just as important, if not more so, than Insulin resistance (Figures 1 & 3)
A lot of people are talking about insulin resistance - the reason why many people ultimately develop diabetes. When you have more sugar than the cells of your body need, the cells protect themselves by becoming less responsive to the insulin. Less responsive = insulin resistance.
The same thing happens with cholesterol. Most, but not all, of your cholesterol is taken up for use by the cells of your body via LDL cholesterol receptors. Just like the insulin receptors for glucose (sugar), when the cells in your body don’t need more cholesterol, the LDL cholesterol receptors become less response (Figure 3). Less responsive = LDL resistance. When these LDL receptors become less responsive, the LDL cholesterol remains in your blood stream longer, where with time it becomes damaged (oxidized). This oxidized cholesterol can enter the walls of the arteries which supply blood to your brain, heart, kidneys, liver; in other words, everywhere. Once inside the walls of your arteries, this oxidized cholesterol - which is an inflammatory irritant to the artery - is taken up or consumed (phagocytized) by a special type of cell, called a macrophage.
Macrophages are specialized cells intended to protect your body. They are part of your defensive immune system designed to fight disease and foreign invaders. By consuming the oxidized cholesterol, the damaged cholesterol is removed from the wall of the arteries. Unfortunately, this results in the death of these macrophages, which have died in defense of your body; thus beginning an inflammatory build up within the walls of your artery, which we call atherosclerosis - or coronary artery (heart) disease.
This inflammatory buildup within the walls of arteries interferes with the ability of the coronary arteries to relax and carry more blood flow to the heart when needed [4,5]. This is atherosclerosis and it is not seen by conventional cardiology tests. Coronary arteriograms with their limitations and reliability problems [5], do not see this buildup within the walls of the artery. Coronary calcium (CAC) scoring, which looks for the presence of calcium – which may or may not be present (Figure 1) - only sees calcium (if present) but tells us nothing about the ability of the arteries to increase their blood flow when needed.
Both arteriograms and CAC scoring are merely anatomic tests. They are limited to seeing a narrowing or calcium, but their failure to see something and their inability to tell you what the arteries are capable of doing [4], provide us limited information. Up to eightyfive percent of people will have a heart attack due to the rupture of this built up inflammatory material, inflammation, which began years earlier within the walls of the arteries. As such the use of coronary arteriograms and CAC scores for assessing the impact of cholesterol lowering drugs is extremely limited and should be cautiously considered.
How do the cholesterol lowering drugs work?
Ninety-three (93) percent of the low-density lipoprotein (LDL) cholesterol in your body, the cholesterol we call the bad cholesterol - because it is this cholesterol, which eventually causes most of the harm to the arteries of your body once oxidized, causing heart attacks, strokes and other major medical problems – is actually in the cells of your body and not the blood stream. It is in the cells of your body, where this LDL is needed – where it is actually being used for cell growth, repair, hormone production, et cetera, where it cannot be measured. However, even too much of a good thing, can be a problem.
This 93% of your body’s cholesterol isn’t measured by sampling your blood for cholesterol. This cholesterol is inside the cells and cannot be measured, at least without taking biopsies (pieces) of your muscles, heart, brain, liver, et cetera. To get this LDL inside your cells to be used requires, as we have mentioned, a special receptor that recognizes the LDL - just like there are insulin receptors that recognize insulin to bring glucose into the cells.
Many of the drugs physicians use to lower your cholesterol, work either by slowing down how much cholesterol your liver makes (that 1000 mg per day) or they work by trying to increase how much LDL cholesterol is taken up from the blood, into the cells of your body. Just because you lower the amount of LDL in your blood, doesn’t mean you are reducing the amount of LDL in your body. In fact if you’re removing it from the blood and putting it inside the cells, you’re clearly not removing it from the body. The consequence of this is an increase in the amount of cholesterol within the cells of the body proper. When those cells are within the walls of the coronary arteries, inflammation can worsen promoting CAD. Coronary arteriograms and CAC scores are not going to see this.
The main drugs for slowing the production of cholesterol by your liver are HMG Co-A reductase inhibitors - affectionately called statins. This is the slowest step in the production of cholesterol by your liver. There is ample evidence that these drugs interfere with co-enzyme Q 10, needed for normal cellular function. There is also unpublished data, showing that damage to muscles, resulting from the use of statins is much higher than previously thought, with studies showing muscle damage even when blood tests for that muscle damage are not elevated.
Another older group of drugs, included here for purpose of being complete, are the bile acid sequestrants. These drugs work inside your gastrointestinal (GI) tract, where they combine with the cholesterol in the bile secreted through your liver and gallbladder to help digest fats you have eaten. By binding with the cholesterol in your bile, the cholesterol is removed from your body when you evacuate your bowels. Thus these drugs actually lower the total body cholesterol burden.
A relatively new group of drugs are the PCSK9 inhibitors. These drugs are antibodies to proprotein convertase subtilisin kexin9 (PCSK9). PCSK9 removes LDL receptors from your liver as part of the naturally occurring clean up (recycling) sequence. The function of PCSK9 is to reduce the number of LDL receptors your liver has, which will reduce the amount of LDL your liver can remove from your blood. Block this with a PCSK9 inhibitor, and the LDL receptors remain in place, resulting in more LDL being removed from your blood by your liver; thereby lowering your blood LDL cholesterol, while increasing your liver LDL cholesterol.
Finally, we have Niacin - also known as vitamin B3. Niacin increases your good (HDL) cholesterol, which you can also do by exercising, not smoking if you are a smoker and reduce the fats and refined foods in your diet. Again, not putting the first thing in your mouth.HDL is a scavenger mechanism. By removing LDL from other parts of the body, HDL can reduce the level of LDL in your blood - but not your body. HDL merely moves the cholesterol around from one place to another, to be dealt with another day. In some instances, HDL can actually harm your body. If the HDL is dysfunctional, which happens either due to genetics or when you have diabetes, inflammation or oxidative stress, this same HDL that was once thought to be only helpful, can actually be pro-inflammatory and cause atherosclerotic heart disease.
Conclusion
The focus of using cholesterol lowering medications, is to lower blood cholesterol levels. However, as we have seen, the real harm occurs within the cells of the body and in particular within the walls of the arteries, where inflammatory plaques result from a combination of factors (Figure 1), including but not limited to oxidized LDL cholesterol. By actually lowering the serum LDL levels, many of these drugs work by increasing the uptake of LDL into the cells of the body proper.
The proposed benefit of these medications, are based upon the lowering of blood LDL cholesterol levels, and reported changes in coronary arteriograms. However, the lack of correlation between changes in blood cholesterol levels and changes in measured physiologic CAD [3] - by simply removing the LDL cholesterol from the blood and placing it into the cells of the body where oxidation may occur – raise significant questions as to the real cost benefit ratios of these drugs.
Given these limitations, it would appear that greater emphasis should be placed on lowering total body cholesterol burden, either through the use of medications which actually lower LDL body cholesterol levels, or through dietary and lifestyle changes which limit the oxidative impact of LDL cholesterol in addition to the other components (Figure 1) responsible for inflammatory coronary artery disease.
Acknowledgment
FMTVDM is issued to the first author. The “Inflammation and Heart Disease” theory was developed by the first author. All figures reproduced with the expressed consent of the first author.
References
- Fleming RM (1999) The Pathogenesis of Vascular Disease. Textbook of Angiology, pp. 787-798.
- Fleming RM (1999) Atherosclerosis: Understanding the relationship between coronary artery disease and stenosis flow reserve. Textbook of Angiology, pp. 381-387.
- Fleming RM, Harrington GM (2008) "What is the Relationship between Myocardial Perfusion Imaging and Coronary Artery Disease Risk Factors and Markers of Inflammation?" Angiology 59:16-25.
- Fleming RM (1999) Atherosclerosis: Understanding the relationship between coronary artery disease and stenosis flow reserve. Textbook of Angiology, pp. 381-387.
- Fleming RM, Kirkeeide RL, Smalling RW, Gould KL (1991) Patterns in Visual Interpretation of Coronary Arteriograms as Detected by Quantitative Coronary Arteriography. J Am Coll Cardiol 18: 945- 951.
- Shah U (2011) Quality and cost of healthcare: an Indian prespective an assessment of direct cost of quality across hospitals in India. Management in Health 15(3).

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...