Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-6070
Research Article(ISSN: 2638-6070) 
Financial Anxiety in Hospitalized Cardiovascular Patients
Volume 1 - Issue 4Malakeh Meshkati and Niloufar Alikhani*
- Department of Financial Management, Islamic Azad University, Iran
Received: July 09, 2018; Published: July 16, 2018
*Corresponding author: Niloufar Alikhani, Department of Financial Management, Islamic Azad University, Iran
DOI: 10.32474/SJFN.2018.01.000116
Abstract
Introduction: Due to the nature of hospitals, the importance of mental relaxation along with the physical health of patients, this study was conducted to investigate the anxiety of hospitalized patients(discharge), looking at the impact of health costs on the rate Anxiety.
Materials and methods: This cross-sectional descriptive-analytic study was carried out using a researcher-made questionnaire. The statistical population of the study included 80 patients with myocardial infarction referring to the Hospital of Farmanieh, Tehran from 23 October to 21November 2017, 12 of whom were discontinued for some reason and 68 completed the questionnaire. The collected data were analyzed using SPSS software and sequential regression statistical test.
Findings: There was a significant relationship between pay out of pocket, employment status and insurance and the amount of anxiety; variables such as age, gender and marital status did not have a significant relationship with patient anxiety. Among the factors indicating anxiety, they received too much concern about the cost of treatment and sleep disturbances in relation to treatment costs, respectively with the highest and lowest levels of financial anxiety.
Conclusion: According to the results, increasing pay out of pocket has a positive effect on patient’s anxiety.
Keywords: Anxiety, Out of Pocket Payment, Myocardial Infarction
Introduction
Anxiety and anxiety disorder is a great health problem, which involves many dimensions including health, finance, family, and work. Over time, symptoms of anxiety may get worse or better, but usually it gets exacerbated when stress occurs [1]. According to development of health-related issues, and the increase in the cost of health-care interventions, a distinct part of household income is allocated to these costs. On the other hand, the fall in the value of household income, due to rising inflation rates, and economic constraints, leads to double pressure on households. Recent investigations shows that the decline of the socioeconomic level can negatively impact on the health status of individuals, while societies and mortality factors evolve, the decline in socio-economic status of individuals can remove them from access to resources that protect or enhance their health against harm caused by dangers. As a result, socioeconomic benefits can increase the health, and reduce the health risk factors. Education and occupation are two key factors in determining household income, which are important determinants, in the individual and household’s socio-economic status [2].
Family, as the most important unit of society, plays an important role in the individual’s health and ability to adapt to different situations. But some factors can affect the health of the family abruptly and change its structure. Several stressors, such as acute and severe illness, or hospitalization of one of the members, can lead the family to anxiety and crisis. Various studies show that, from every 4 to 5 people, one person suffers from psychiatric disorders each year due to stress. Therefore, it is essential that some protections and strategies used to prevent and reduce the anxiety risk factors [3]. One of these risk factors that always causes increased stress and anxiety at the onset time of illness, is the psychological stress caused by the inability to pay treatment costs.
According to a recent WHO report, death in the 10 past years have been the highest rates of heart disease (15 million deaths in 2015, 17 million deaths in 2008) [4]. Anxiety is always one of the causes of heart disease, which at the same time is one of the side effects of the disease. Anxiety is one of the most commonly diagnosed psychiatric patients’ responses to cardiovascular events which may lead to physical or psychological consequences if they continue or intensify [5,6]. Expecting cardiac surgery, hospitalization, fear of death, hearing about the deaths of people with the same disease, and generally fear of unknowing and unknown causes anxiety in the patient and his fellows [7].
According to a study by Jeff C Huffman [8], the anxiety among heart patients is common, and 20 to 50% of these patients have expressed anxiety. Panthee [9] in their study concluded that patients with myocardial infarction had a high degree of anxiety, which reduced their quality of life [9]. According to these studies, the purpose of this study was to investigate the financial anxiety of patients referred to cardiac problems (with a priority of myocardial infarction), at the time of discharge from the hospital, so that if the cost of treatment is effective on anxiety of patients, in addition to other stressors, we will achieve some strategies to prevent and ultimately reduce the psychological effects of hospital costs, because the main goal of each health center is to reduce suffering and relieve the clients, not to add to their inconveniences and concerns.
Materials and Methods
The present study is descriptive-analytic, cross-sectional, and questionnaire based evaluation (validated by experts). The study population included patients with myocardial infarction referring to the Hospital of Farmanieh, Tehran, from October 23 to November 21, 2017. The reason for randomly choosing of these patients was the high cost of their treatment in all over the world, as well as the high frequency of this disease patient, compared to the rate of disease and its costs in other patient groups. The sample size is 65 and we recruited 15 more patients for sample loss probability. After the census, 68 were willing to participate in the research with oral satisfaction (7 people died and 5 did not agree to do research).
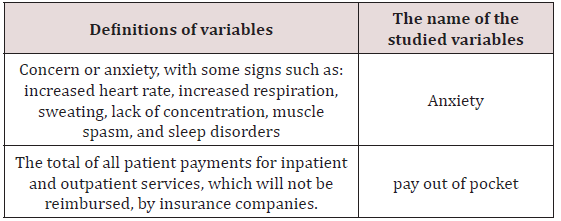
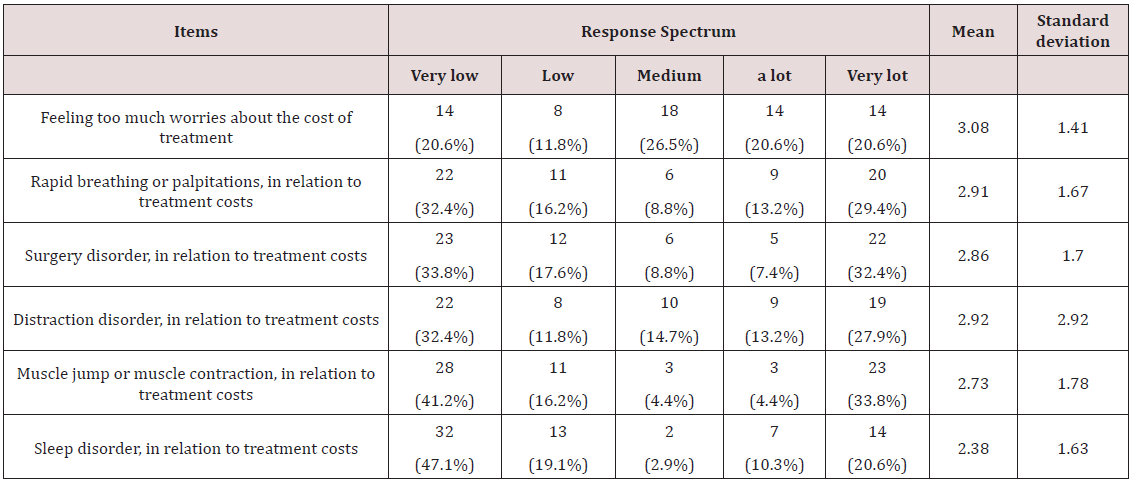
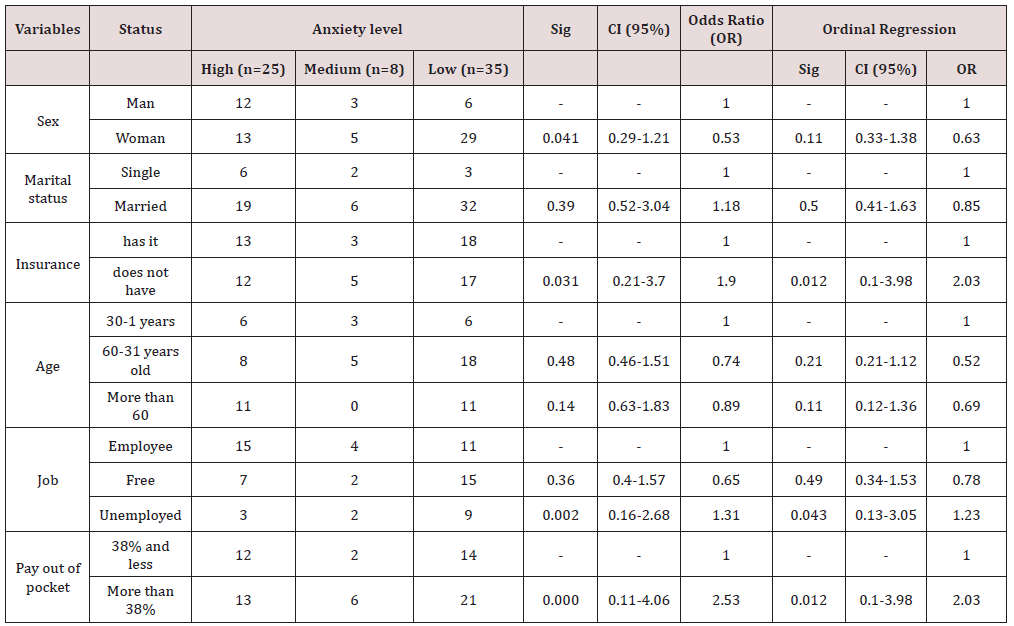
In order to determine the level of financial anxiety of patients, we used 6 questionnaires, five options Likert, with the options, very high (5), high (4), medium (3), little (2), and very little (1). Grades were classified as follows: 1-2.5 for low anxiety levels, 2.5-3.5 for moderate anxiety, and more than 3.5 for high anxiety levels. Also, to investigate the total cost of patients, and the direct payment share, we inquired about the discharge unit, and we filed the sums. Paid patients out of pocket were also 38% nationwide, based on reported rates (referrals), and patients were divided into two groups, pay out pocket up 38%, and pay out of pocket more than 38% . The variables of the research are described in the table below Table 1. The data were analyzed by SPSS software version 22 and sequential regression tests at individual level (crude chance ratio) and overall level, and the findings were reported in terms of odds ratio, confidence interval, and amount meaningful.
Findings
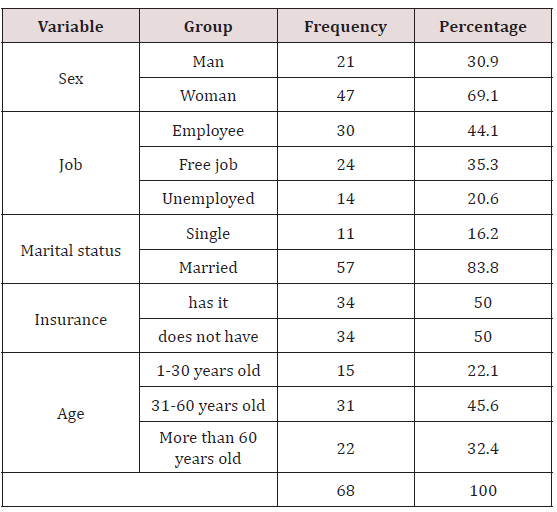
The demographic data of 68 patients were presented in Table 2. Most patients were female (69.1%), employees (44.1%), married (83.8%), and in the age group of 31-60 (45.6%). According to the research findings, the excessive feeling of concern regarding treatment costs and sleep disturbances in relation to treatment costs resulted in the highest and lowest levels of financial stress, with a mean of 1.41 ± 3.08 and standard deviation, and 1.63 ± 2.38 (Table 3). The study of the effective factors on financial anxiety showed that there was no significant difference in the level of anxiety of patients based on variables such as gender, marital status and age (p>0.05). In case of having health insurance, non-insured patients were 2.03 times more likely than those with insurance. The likelihood of exposure to financial anxiety in the treatment costs was p=0.012 (CI: 0.1-3.98 OR=2.03). In terms of job variables, unemployed patients had 1.23 times more chance of financial anxiety and a significant difference was found between the patients in terms of job (p = 0.043; CI: 0.13-3.05; OR=1.23). Pay out pocket, in patients who paid more than 38% of the total cost of the disease, had caused 2.03 times more exposure to financial anxiety, indicating that patients’ financial anxiety increased more with increasing Pay out the pocket, (p=0.012; CI: 0.1-3.98; OR=2.03) (Table 4).
Discussion and Conclusion
The results of the study indicate that the relationship between pay out of pocket patients and their anxiety levels is positive, and if the increase in direct payments exceeds 38% of total costs, patients’ levels of anxiety increase. Patel, Kleinman’s [10] study confirmed the correlation between low incomes in developing countries and the risk of mental illness. Mirsamadi [11] concluded that living costs are one of the main causes of stress in health center managers, they are fully aware that heavier medical costs will reduce the likelihood of their therapeutic interventions on the patient and will lead to a decline in the quality of their health center actions [11]. Pourreza et al. [12] Stated that the adoption of new policies on the payment of heavy costs for cancer patients, in particular by insurance agencies, financial support from financial institutions such as banks, or charities, the distribution of specialized cancer centers, or Providing housing for patients who have come from distant cities, in addition to realizing health equity indicators, can reduce the financial problems facing cancer patients, and helps them to better overcome their own illness with no significant anxiety risk factors changes.
Ross et al. [13], in a study conducted in 2003 and 2004, reported about financial stress in patients with Acute Myocardial Infarction (AMI), half of the patients reported having some levels of financial stress while admitting to the hospital, and close One third of patients reported having a financial stress, that these stressful conditions led to their deterioration, increased hospitalization time, decreased patient response to treatment interventions and increased surgical risk. Along with this study, the increase in treatment costs has led to a worsening of the outcomes of the disease in these patients.
One of the reasons for inducing anxiety among people in cope with health costs is the current limitation of the current and available financial resources of individuals, who are investigating the impact of the status of their clients’ employment, as well as their insurance coverage, on this. The economic conditions in developing countries are such that most people have limited monthly income, and no amount is considered for this treatment. Also, in these countries, the risk of developing cardiovascular disease is higher than other countries, in other words, developing countries have a greater role in the incidence of cardiovascular disease worldwide, more risk factors, and less government support. In current study, it was concluded that the job status has a significant relationship with patient anxiety and non-insurance patients with a higher chance of anxiety. In this regard, Herman [14] announced in his report that health insurance should be available to all individuals globally, as a result of protecting the patient in unexpected circumstances and preventing the debtor from being financially mistreated, is one of the requirements for reforming the health system in any country.
Puccard, et al. (2005) Also noted that individual, interpersonal, social, economic, psychological, and environmental factors, contributed to the anxiety of the family members of the patient hospitalized are effective factors . Particularly, various studies have pointed to the impact of pocket payments on household income cuts [15]. Crawford [16] concluded that there is no significant relationship between age and marital status, and stress . In the present study, the relationship between these two variables and the level of patient anxiety was not significant. Arab [17] state, with increasing health spending, which is more than wage increases, more people need more welfare insurance coverage. Health insurance protects customers, especially those with limited financial resources, or excessive need for health services. Bakar [18] also state that the amount of pay out of pocket costs is one of the factors influencing the decision to buy insurance from stateless people. In this regard, the present study confirms that patients without insurance coverage have anxiety more than those who have insurance coverage.
Therefore, the high cost of treatment in cardiovascular diseases leads to anxiety in patients, anxiety during the hospitalization period, an increase in the length of the hospitalization period, a decrease in the effectiveness of the results of interventions in patients and an increase in mortality rates in these patients. On the other hand, with the improvement in treatment costs, the reduction in community anxiety reduces the incidence of various diseases, including cardiovascular disease [19]. Therefore, government support for treatment costs is a form of economic investment in the health system of the country, and governments are advised to support healthcare costs. Based on the results, it is suggested that research be conducted in the field of patient surveys, in order to receive comments and suggestions on how to deal with the personnel of the clearance unit, and to declare costs by him, the appointment of a psychologist if symptoms are manifested Anxiety in patients, and promotion of solutions to the ill-health of patients who do not have adequate insurance coverage, in addition to ensuring the health of patients, also their mental health during discharge.
Acknowledgements
We would like to thank the participants for their participation and invaluable contribution to this study. Compliance with Ethical Standards
Ethical Approval
All procedures followed were in accordance with ethical standards of the responsible committees on human experimentation and with the Helsinki Declaration of 1975 and its later amendments or comparable ethical standards. This study was a survey and verbal consent was obtained from all participants for completing the questionnaires.
References
- Naseri H, Fathalilavasani F (2015) Guide for general anxiety disorder management. Ministry of health and medical education, Iran.
- Ahmadi AM, Taheri E (2017) Factors Affecting Health Expenditures of Households in Iran: Application of Ordered Probit Model. Journal of health administration 20(67): 89-98.
- Rabie Siahkali S, Avazeh A, Eskandari F, Khaleghdoost Mohamadi T, Mazloom S, et al. (2011) A Survey on Psychological and Environmental Factors on Family Anxiety of the Hospitalized Patients in Intensive Care Units. Iranian Journal of Critical Care Nursing 4(3): 175-180.
- WHO (2018) The top 10 causes of death. United Nations.
- Frasure S (1991) In-hospital symptoms of psychological stress as predictors of long-term outcomes after acute myocardial infarction in men. Am J Cardiol 67(2): 121-127.
- Moser DK (2007) The Rust of Life: Impact of Anxiety on Cardiac Patients. Am J Care 16(4): 361-369.
- Mamishi N, Sami B (2006) Medical Surgical Nursing Cardiovascular Brunner and Suddarth. Tehran: Boshra, p. 163-175.
- Huffman JC, M Celano Ch, Januzzi JL (2010) The relationship between depression, anxiety,and cardiovascular outcomes in patients with acute coronary syndromes. Dove Press journal: Neuropsychiatric Disease and Treatment 6: 123-136.
- Pantheeb, Kritprachach (2011) Review: Anxiety and Quality of life in patients with myocardial infarction. Nurse Media Journal of Nursing, p. 105-115.
- Patel V, Kleinman A (2003) Poverty and common mental disorders in developing countries. Bulletin of the World Health Organization 81(8): 609-615.
- Mirsamadi M, Jafarpour A (2006) Factors Causing Stress in Medical Managers in Tehran. Iranian Journal of Psychiatry and Clinical Psychology 11(4): 449-454.
- Bazyar M, pourreza A, Harirchi I, Akbari F, Mahmoudi M (2011) Medical and non-medical direct costs of cancers in patients hospitalized in Imam Khomeini cancer institution-2010. Hospital Journal 11(1): 39-50.
- Joseph S Ross, Sachin J Shah, Harlan M Krumholz, Kimberly J Reid, Saif S Rathore, et al. (2012) Financial Stress and Outcomes after Acute Myocardial Infarction. PLOS ONE. Volume 7(10): e47420.
- Patricia M, Herman (2011) Health insurance status, medical debt, and their impact on access to care in Arizona. Am J Public Health 101(8): 1437-1443.
- Piamjariyakul U, Yadrich DM, Russell C, Myer J, Prinyarux C, et al. (2015) Patients’ Annual Income Adequacy, Insurance Premiums and Out-of- Pocket Expenses Related to Heart Failure Care. Heart Lung 43(5): 469- 475.
- Crawford JR, Henry J (2005) The Depression Anxiety Stress Scales (DASS): normative data and latent structure in a large non-clinical sample. Br J Clin Psychol 44(2): 111-131.
- Arab M, Kavousi Z, Ravangard R, Ostovar R (2017) Book: Health Isurance Systems. p. 14.
- Abu Bakar A, Regupathi A, Aljunid SM (2012) Factors affecting demand for individual health insurance in Malaysia. BMC Public Health 12(2): A10.
- Pochard F, Darmon M, Fassier T, Bollaert PE, Cheval C, et al. (2005) Symptoms of anxiety and depression in family members of intensive care unit patients before discharge or death: A prospective multicenter study. J Crit Care 20(1): 90-96.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...