Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4692
Research Article(ISSN: 2637-4692) 
The Personalized Design and Production of Indirect Bonding Technology Based on CAD and RP Technology in Orthodontics Volume 4 - Issue 5
Huifang Yang*1 and Siwei Wang2
- 1Center of Digital Dentistry, Peking University School and Hospital of Stomatology, China
- 2Department of Orthodontics, Peking University School and Hospital of Stomatology, China
Received: April 24, 2021 Published:May 10, 2021
Corresponding author: Huifang Yang, Center of Digital Dentistry, Peking University School and Hospital of Stomatology, National Center of Stomatology, Research Center of Engineering and Technology for Digital Dentistry of Ministry of Health and Beijing Key Laboratory of Digital Stomatology, China
DOI: 10.32474/MADOHC.2021.04.000199
Abstract
Objective: This paper introduces a method to make a transfer tray for indirect bracket bonding by using the Three-Dimensional (3D) software packages. Using the advanced technology of Computer-Aided Design (CAD) and Rapid Prototyping (RP) technology to reduce chair time and improve the bonding precision in orthodontics.
Method: The procedure included data acquisition of cast model and CBCT data. With the data, the tooth was segmented one by one, and the segmented data was saved as Stereolithography (STL) files. The tooth data and the cast data could be seen in a same 3D digital software and with the data the bracket position was decided by doctors. The transfer tray was designed in a reverse engineering software and printed by a 3D printing device.
Result: The method was used to make an individualized transfer tray in orthodontics.
Conclusion: With 3D scanning, CAD and RP technology, an efficient method of transfer tray production was established, which could meet clinical needs in indirect bonding of orthodontic and achieve a high efficiency and accuracy
Keywords: Transfer tray; CAD; Bracket; Indirect bonding; RP
Introduction
Indirect bonding in orthodontic is a method of bracket placement in which the brackets are placed simultaneously on the patient’s teeth. Good design and precise operation could lead to better treatment results and shorter treatment times. In recent years there has been an increase interests in the research of indirect bonding procedure. The ideal bracket placement will correct tooth positions in 3 planes during treatment [1,2]. [3] have enumerated 4 elements that demand attention when positioning brackets (1) bracket base adaptation to the contour of tooth surface (2) the rotational position of each bracket from the occlusal direction (3) the vertical position of each bracket (4) the desired slot angulations of each bracket by evaluating the position of the roots [3]. Hodge et al stated that there was no significant difference between the mean errors or risks produced by the indirect or direct bonding method for bracket placement [4,5]. Several other studies shown that indirect bonding is a more accurate and efficient technique for bracket placement [6,7]. Many factors might affect the clinician’s precision in bracket position, such as experience, sharpness of sight and manual dexterity. Using transfer trays can reduce the impact of human operation. Transfer trays are individually designed on a computer and produced with a rapid prototyping procedure [8]. So, the technology of improving bracket placement accuracy still should be explored. Computer-Aided Design (CAD), Computer- Aided Manufacturing (CAM) and Rapid Prototyping (RP) are hightech procedures used in stomatology [8-11]. Various utilities and methods have been developed for indirect bonding and precise bracket placement [12,13]. Recent imaging techniques have allowed complete visualization of different tissues in 3 dimensions. CBCT imaging could provide detailed images of the bone and be performed to evaluate diseases of the jaw, dentition, bony structures of the face, nasal cavity, nerve canals and sinuses. Based on the CBCT data, the anatomical information of mandibular canal, root and crown were reconstructed [14]. With three-dimensional scanner, all the surface information of the dental cast models can be got. Doctors could make more accurate treatment for maintaining crown and root in their new position [15]. To help the clinician save time and achieve more accurate bracket placement, in this study, two commercial software packages, Geomagic Studio 2012 (3D Systems, USA) and Amira 5.4 (VSG, Visualization Sciences Group, Germany) were used to complete the CAD process for a transfer tray of indirect bonding.
Materials and Methods
Tools
a. Software: Amira 5.4 (VSG, Visualization Sciences Group, Germany), 3Shape 3D Viewer (3Shape Company, Denmark), Geomagic Studio 2012 (3D Systems Company, America).
b. Hardware: CBCT (DCT Pro, Vatech & EWOO Group, South Korea), Activity102 3D Scanner (Smart Optics Company, Germany).
Data Processing
Data acquisition
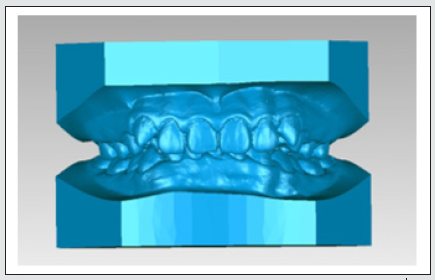
One male patient was selected as the experimental subject. The maxillary CBCT scans were performed on the i-CAT Imaging system. The scanning conditions were constant with 360 rotation. Images were obtained using the following protocol: field of view, 200×190mm2; 90Kvp; 144mA; scan time, 24s; voxel size, 0.4mm. Scanning conditions were constant with 360 rotation. All data were saved in the DICOM 3.0 format. All the data of the models were saved as Stereolithography (stl) files. The plaster model was scanned by Activity102 3D Scanner and the scanned data was saved as ‘Model_Maxillary.stl’ and ‘Model_ Mandibular.stl’ Figure 1.
Teeth Segmentation
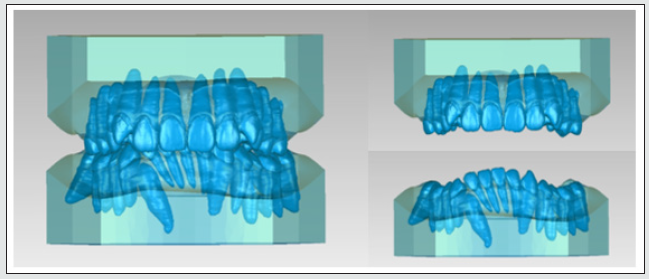
Amira 5.4 software was used to segment the CBCT data, and the tooth was segmented one by one manually. Then the data was saved as ‘Teeth_ Maxillary.stl’ and ‘Teeth_ Mandibular.stl’.
Registration
The registration was linear transformation which include rotation and translation. With the software of Geomagic Studio 2012, using the ‘Manual Registration’ settings, fixed the model data and aligned the teeth and models data, so the stl data of teeth and the models were in a same coordinate system Figure 2.
Orthodontic bracket placement in the software
Orthodontists strive for accurate bracket positioning and hope it can achieve a superior occlusion easier. Doctors assessed the bracket positioning early in treatment by clinical and radiographic evaluations. After the teeth segmentation, doctors could see the crown and root at the same time. With all the information, all the brackets were put in the correct position for clinical height and angulation by doctors in the software of Geomagic Studio 2012.
CAD of transfer tray
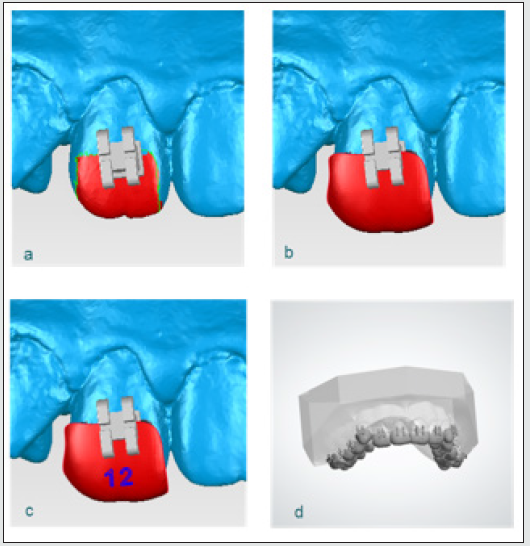
All the designed data was stored in the reverse engineering software of Geomagic Studio 2012, using an interactive selection tools command, the area of occlusal surface of the teeth was extracted and trimmed Figure 3a. The trimmed surface was then offset along the normal direction by 1.2mm, forming an interior surface of the transfer tray. To create the solid 3D model of the transfer tray body, a 1.2-mm shell of the interior surface of the tray was drawn out. Within the Boolean command, the transfer tray body was subtracting by bracket, so a new object was created. Figure 3b All this process was made manually one by one tooth or more than one tooth. Each transfer tray was tagged with tooth information. Figure 3c So all the transfer tray was made. The designed transfer tray data was then saved in the STL file format Figure 3d.
Figure 3: The CAD process of transfer tray in Geomagic 2012, a. is the extracted tooth surface, b. is the transfer tray body which was subtract by bracket c. is the transfer tray was tagged with tooth information d. is all the designed transfer tray data of maxillary.
3D printing
The CAD transfer tray data was imported into a computer system connected to the 3D printer (Objet30 Pro, Stratasys, Israel), and the transfer tray was printed layer upon layer at 16μm/layer using Vero Clear filament Figure 4.
Results
The method could be used to make an individualized transfer tray in orthodontics within the digital method. From imaging to CAD and manufacture technologies, the transfer tray can be made feasibly. Figure 5 The entire design process took approximately 2 min for each tooth transfer tray.
Discussion and Conclusion
This paper proposes a reverse engineering method for the design of transfer tray and based on the scanned models and bracket models. The data for the transfer tray design are based on the results of the scanned plaster model and the design process could base on one or more teeth which decided by doctors, so the transfer tray and the teeth will fit well, and it is convenient for doctors to remove it after bonding. The advantages of this design flow are that doctors can position the bracket based on tooth root data and crown data, which could avoid the hidden danger that teeth roots move to outside the cortex during the treatment. The results show that the design has higher bonding efficiency and precision. In future, the individual designs can meet clinical application requirements better with this method.
Acknowledgement
This study was supported by funding from the Ministry of Education of China Online Fund (grant no. 2017YB192).
References
- Nir Shpack, Silvia Geron, Ioannis Floris, Moshe Davidovitch, Tamar Brosh, et al. (2007) Bracket placement in lingual vs labial systems and direct vs indirect bonding. Angle Orthod 77(3): 509-517.
- Ahmadreza Sardarian, Shahla Momeni Danaei, Shoaleh Shahidi, Sahar Ghodsi Boushehri, Allahyar Geramy (2014) The effect of vertical bracket positioning on torque and the resultant stress in the periodontal ligament-a finite element study. Prog Orthod 15(1): 50.
- Carlson SK, E Johnson (2001) Bracket positioning and resets: Five steps to align crowns and roots consistently. Am J Orthod Dentofacial Orthop 119(1): 76-80.
- TM Hodge, AA Dhopatkar, WP Rock, DJ Spary (2004) A randomized clinical trial comparing the accuracy of direct versus indirect bracket placement. J Orthod 31(2): 132-137.
- Bovali E, S Kiliaridis, MA Cornelis (2014) Indirect vs direct bonding of mandibular fixed retainers in orthodontic patients: A single-center randomized controlled trial comparing placement time and failure over a 6-month period. American Journal of Orthodontics and Dentofacial Orthopedics 146(6): 701-708.
- Koo BC, CH Chung, RL Vanarsdall (1999) Comparison of the accuracy of bracket placement between direct and indirect bonding techniques. American journal of orthodontics and dentofacial orthopedics: Official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics 116(3): 346-351.
- Garino F, GB Garino (2005) Computer-aided interactive indirect bonding. Progress in Orthodontics 6(2): 214-223.
- Fabio Ciuffolo, Ettore Epifania, Gionni Duranti, Valentina De Luca, Daniele Raviglia, et al., (2006) Rapid prototyping: A new method of preparing trays for indirect bonding. American Journal of Orthodontics and Dentofacial Orthopedics 129(1): 75-77.
- Fusong Yuan, Yong Wang, Yaopeng Zhang, Yuchun Sun, Dangxiao Wang, et al. (2016) An automatic tooth preparation technique: A preliminary study. Scientific Reports 6: 25281.
- Stansbury JW, MJ Idacavage (2016) 3D printing with polymers: Challenges among expanding options and opportunities. Dental Materials 32(1): 54-64.
- Kumar A, H Ghafoor (2015) Rapid prototyping: A future in orthodontics. p: 1-7.
- Nichols DA, G Gardner, AD Carballeyra (2013) Reproducibility of bracket positioning in the indirect bonding technique. American journal of orthodontics and dentofacial orthopedics: Official publication of the American Association of Orthodontists, its constituent societies. American Board of Orthodontics 144(5): 770-776.
- Ahmed M El-Timamy, Fouad A El-Sharaby, Faten H Eid, Yehya A Mostafa (2016) Three-dimensional imaging for indirect-direct bonding. American Journal of Orthodontics and Dentofacial Orthopedics 149(6): 928-931.
- Kovisto T, M Ahmad, WR Bowles (2011) Proximity of the mandibular canal to the tooth apex. J Endod 37(3): 311-315.
- Cheng Cheng, Xiaosheng Cheng, Ning Dai, Yi Liu, Qilei Fan, et al., (2015) Personalized Orthodontic Accurate Tooth Arrangement System with Complete Teeth Model. Journal of Medical Systems 39(9): 84.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...