Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4692
Research Article(ISSN: 2637-4692) 
Micro X-Ray Spectral Analysis and in Vivo Studies of Complex-Modified Titanium Implants Volume 5 - Issue 2
UE Eshkulov1, S Yu, Ivanov1,2, AI Shaikh Liev2, AB Dymnikov1 and EA Gosteva3,4*
- 1The Peoples’ Friendship University of Russia, 6 Miklukho-Maklaya St, Moscow, Russia
- 2First Moscow State Medical University named after I.M. Sechenov of the Ministry of Health care of Russia, Sechenov University, Russia
- 3Academy of Engineering, RUDN University, Russia
- 4National University of Science and Technology MISiS, 4 Leninsky Prospekt, Russia
Received: February 3, 2022 Published: February 11, 2022
Corresponding author: EA Gosteva, National University of Science and Technology MISiS, 4 Leninsky Prospekt, Russia
DOI: 10.32474/MADOHC.2022.05.000209
Annotation
Currently, dental implantology continues to develop actively. There are more than a hundred manufacturers of dental implants
(DI) and methods of processing their surfaces on the market. The traditional methods of modifying the DI surface include shot
blasting with fractions (TiO2, Al2O3, SiO2, hydroxyapatite) followed by acid etching; anodizing method; laser treatment; spraying
metals or salts on the surface of the DI. As a result, the surfaces of dental implants acquire macro- and micro-roughness, porosity
to increase the area of contact with the bone tissue [1] . The cleanliness of the surface of a dental implant that has undergone
preliminary processing and cleaning methods determines the quality of osseointegration and its stability during the functioning
of the implant. However, a number of studies indicate that the contained metal impurities in titanium alloys, over time, are able
to migrate into the surrounding tissues, leading to an interruption of osseointegration, bone resorption and, subsequently, to the
loss of the implant. In addition, there is an opinion about a possible systemic negative effect of metal ions on the microorganism
(Aluminum - Al, Vanadium - V, Iron - Fe) coming out of the titanium alloy. A number of authors have demonstrated the possibility of
emission of nanosized metal particles from the surface of dental implants and metal meshes into the aqueous medium, identified
them, and studied the response to basophils in the venous blood of patients [2-4].
The purpose of our study was to assess the effect of the developed method of complex modification of the surface of the DI,
including sequential mechanical treatment and irradiation with PIB (powerful ion beams) of dental implants made of Grade
1 alloy. The proposed method made it possible to increase the physicomechanical properties of the titanium surface and, as a
consequence, the bio inertness of the implant itself. A histomorphometric study of intraosseous dental implants treated with PIB
in an experimental model of miniature pigs revealed high osseointegrative properties, comparable to other methods of surface
treatment of the DI.
Keywords: Micro X-Ray Spectral Analysis; Irradiation with Powerful Ion Beams; Dental Implant; Osseointegration; Microroughness
Introduction
Ceramic implants (PURE Ceramic Implant, Institute Straumann AG, Basel, Switzerland) with a regular diameter of 4.1 mm have recently been placed. Ceramic implants offer benefits to patients with metal allergies, or in patients who may require metal-free restorations [2]. The possibilities of surgical implantation protocols are expanding, in particular due to the improvement of the macroand micro relief of dental implants (DI). DI manufacturers pay great attention to surface modification of titanium alloys. The optimal conditions for osseointegration of dental implants are developed surface micro relief (roughness), porosity and sterility (cleanliness of the DI surface) [5]. To date, the authors have proposed a classification of the surface of dental implants depending on the degree of roughness: smooth up to 0.5 microns, minimally rough 0.5- 1 microns and moderately rough 1.0-2.0 microns, rough from 2 and above [6]. The successful course of the process of osseointegration of dental implants is largely determined by the physicochemical and structural state of the surface layers. Therefore, the issues of developing new methods for processing dental implants that can increase the surface cleanliness isolate the internal structure of the implant, preventing the migration of metal impurities into the surrounding tissue and increasing the physical and mechanical parameters of dental titanium implants remains relevant. The modification method proposed by us is promising from the point of view of cleaning the DI surface from chemical elements after preliminary treatment, prevents the migration of metal impurities into the surrounding tissues. The procedure for powerful ion beams (PIB) processing of titanium samples is described in this research [7]. Purpose of the study - conduct preclinical studies of the surface of the DI, modified by various processing methods on an experimental model.
Materials and methods
To modify the surface of the DI was used a high-current pulsed accelerator “Temp-4M”. This device has a certain beam composition, current density kA cm-2, fluencies per pulse up to several hundred J cm-2 and the nanosecond duration of the current is 10-8 - 10-6 s. The DI surface was processed in several pulses for the optimal rough, porous surface. Beams of light ions (carbon, hydrogen) proved to be effective, capable of providing modification at depths exceeding 10-20 times beams of heavy ions with lower fluencies. The number of pulses was chosen equal to 10. The study of the local chemical composition of the DI was carried out by micro X-ray spectral microanalysis (MRSA) in accordance with GOST 22309-2015 and the study of the structure was determinate on scanning electron microscope “Zeiss EVO MA 10” (Carl Zeiss, Great Britain) equipped with energy-dispersive spectrometer “X-Max”.
In Vivo Research
The experimental research was carried out on the basis of the Vivarium FMBA RUSSIA, (Svetlye Gory city). Six healthy and mature male mini-pigs of the Svetlogorsk breed were employed for the animal investigation. In this study, all the implantation surgeries fulfilled the requirements of the Animal Care and Experiment Committee. All operations were performed under anesthesia with Rometar and Zoletil 100, as well as local infiltration anesthesia with Ultracain DS 4%. Four and three implant holes were made in the left and right lower jaw for implanting. After 4 months of the osseointegration of the DI, a bone fragment was taken, which was subsequently transferred for histo-morphometric examination. After 6 months, the test samples were installed in the area of the extracted teeth, according to the protocol of dental implantation. For the study, 3 groups of DI were prepared from the VT1-0 alloy with a diameter of 4 mm and a length of 10 mm: 1 st group – 12 DI with a smooth surface; 2 st group - 12 implants after double acid etching; 3 st group – 12 implants after complex treatment with PIB. A total of 6 minipigs were involved in the study. Each animal received 2 implants of the same type: one for the upper and one for the lower jaw. Thus, there were 6 animals in each group. At the end of the experiment, an alveolar bone fragment with an implant was resected to the animals under anesthesia. Euthanasia was not performed. The distal sections of the upper jaw and lower jaw were selected as the area of surgical intervention due to the optimal density of bone tissue in these areas, comparable to the variant of the structure of the human jawbone tissue, density D2 – D3.
Histological Examination
Pig jaw fragments with implants were placed in 10% neutral formalin and fixed for 24 hours. Then they were transferred to absolute isopropanol, which was replaced three times. Then, the impregnation was carried out with the Technovit 4200 solution with its successive change three times. Polymerization was carried out according to the manufacturer’s instructions in a Technomat apparatus under conditions of increased pressure (2 Bar) for 10 minutes. Finished blocks were cut to remove excess plastic and blanks were formed for the subsequent section. The section of the blocks was carried out on an Isomet 4000 apparatus (Buechler, USA). As a result, sections with a thickness of 100 μm were obtained, which were glued to glass with acrylate glue and polished on polishing wheels with a sequential change in grain size from 200 to 1200. Finished thin sections (histopreparations) were stained according to the technique of heavenly trichromitoluidine blue [8].
Morphometric Research
To assess osseointegration used recommended methodology histomorphometry [9]. Determined the relative area of contact between bone and implant (BIC), fibrous tissue and implant (FIC), bone marrow and implant (MaIC). The relative area was expressed as a percentage of the sum of all areas. Osseo integration was assessed as good with BIC values> 75%, satisfactory BIC> 51%, and unsatisfactory BIC <51%. Statistical data processing was performed using the Statistica version 12 software (TIBCO Software, Palo Alto, California, United States). To check the normality of the samples, the Shapiro-Wilk test was calculated. For pairwise comparison of groups, a nonparametric version of the Newman-Keuls test was chosen.
Results and Discussion
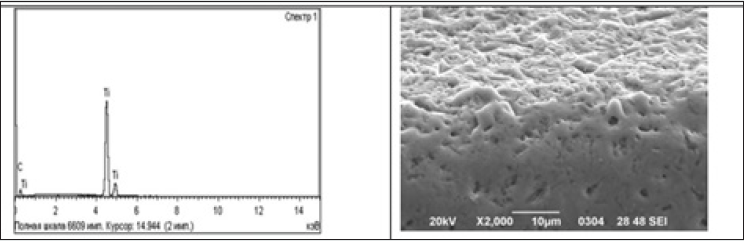
As a result of determining the chemical composition of the surface zone of an implant made of VT1-0 alloy by micro X-ray spectral analysis (MRSA), it was established that the main element present in the alloy is Ti (Figure 1), which corresponds to the chemical composition of this alloy according to GOST 1.90013. Selected sites the presence of silicon (Si) of various stoichiometry was found. The size of individual inclusions reaches 150-200 microns. The use of surfactants or etching in various acidic environments, as a rule, does not lead to complete cleaning of the surface from silicon particles. Since the presence of silicon, which is a toxic element, is unacceptable on the surface of any endoprostheses, it becomes quite obvious that it is impossible to use dental implants immediately after sandblasting. As a result of determining the chemical composition of the surface zone of the implant made of VT1-0 alloy by micro X-ray spectral analysis (MRSA), it was established after PIB treatment that the main element present in the alloy is Ti (Figure 1), there are no silicon (Si) particles.
Figure 1: MRSA and fractographic images at various magnifications of the experimental titanium implant Grade 1 (after preliminary treatments and powerful ion beams)
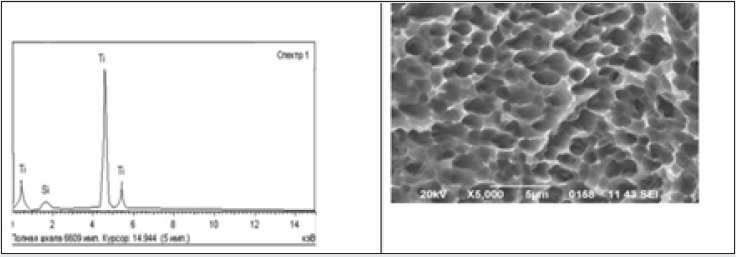
As can be seen from the presented photographs obtained by scanning electron microscopy, the general view of the implant surface (Figure 2) indicates the inhomogeneity of the treatment - the size of individual “depressions” on the surface is 80-100 μm. The result obtained meets all the requirements of GOST and the rough surface of the DI. MRSA confirm positive treatment impact: significant the presence of aluminum (Al) and oxygen (O), as well as traces of iron (Fe), which were detected before processing and could appear as a result of blowing, were completely removed. The surface morphology of DI VT1-0 is a clear pronounced structural anisotropy - the grains are elongated in the vertical direction (Figure 1). Pitted relief of “grooves” etching in the volume of the investigated surface is uniform - both inside one grain and over the entire surface as a whole. The size of the etching pits does not exceed 5 microns. The creation of such morphology of the relief, which ensures the uniformity of etching over the entire surface, should have a positive effect on the process of osseointegration.
Results Invivo Research
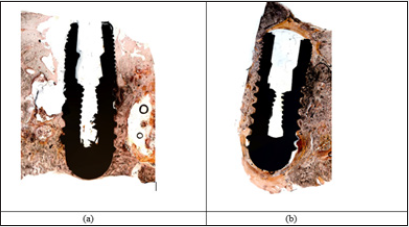
All installed implants were osteintegrated. Histological examination of the bone blocks of the lower jaw with dental implants installed in them revealed that the bone block is represented by an array of bone substance, without clear differentiation into the cortical and spongy layers. The cortical layer with the periosteum with well-defined Folkman canals with a narrow lumen, in which vessels of various diameters and degrees of maturity were found. The periosteum is represented by dense fibrous connective tissue with fibroblast-like cells located between the fibers of the connective tissue. The highest concentration of fibroblast-like cells is in its functional layer. The spongy substance is represented by sharply thickened bone trabeculae with narrow Haversian canals. There are vessels of various diameters inside the canals. The bone mass contains screw intraosseous dental implants. Most implants are slightly submerged below the surface of the alveolar ridge. The implants are surrounded by lamellar bone tissue, which adheres tightly to the metal. It contains vessels of various sizes in narrow Haversian channels. In some places, the bone tissue is replaced by the reticular stroma of the bone marrow, the connective tissue of which is attached to the metal, sometimes not tightly. In the slit space between the connective tissue, homogeneous fine-fiber structures without structural organization (Figures 3 A & B). Thus, histological examination of dental implants revealed good osseointegration with bone tissue. Bone tissue is formed over its entire surface. For a detailed study of osseointegration is morphometric measurements [6,7].
Figure 3: а) Implant Group (processed by PIB), Staining celestial Trichrome X50; b) Implant II Groups acid etching, Statining heavenly richrome X50.
Morphological Research
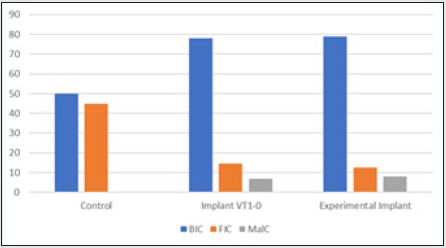
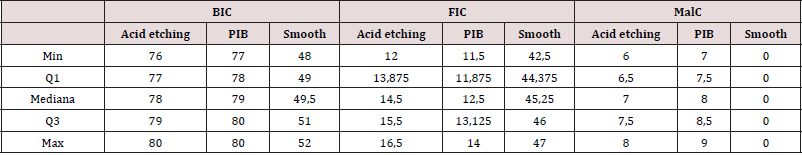
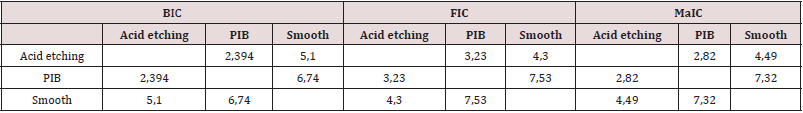
Morphometric examination of bone tissue samples with the studied implants revealed that the implants treated with PIB and acid etching, in terms of BIC (bone to implant contact - bone and implant contact) have comparable osseointegration with very high rates: BICII = 78%, BICIII = 79% (Figure 4). The results of statistical processing of the data showed that the data do not obey a normal distribution. To detect differences in osseointegration of implants with different surfaces for each of the three groups (BIC, FIC, MaIC), a Kruskal-Walli’s analysis was performed. The values of the Kruskal-Walli’s criterion were 25.17, 28.71, and 28.69, respectively, at 9.21 critical χ2 at a confidence level of p <0.05, which indicates statistically significant differences in osseointegration of implants with different types of surfaces. Descriptive statistics for the data obtained are presented in Table 1. For pairwise comparison of groups, a nonparametric version of the Newman-Keuls test was chosen (Table 2). 2,242 is the critical value of this criterion for 3 groups at a confidence level of 0.05; if the number is more than 2,242, then the differences are statistically significant with a probability of 95%, if less, then they are not significant. According to him, there are statistically significant differences between osseointegration of implants after treatment with PIB and implants with a smooth surface in terms of BIC, FIC and MaIC (p <0.05), there are statistically significant differences between osseointegration of implants with an acid-etched surface and a smooth surface in terms of BIC. FIC and MaIC (p <0.05). However, there are no statistically significant differences in BIC and MaIC values between implants after treatment with PIB and implants with an acid-etched surface, but there are differences in FIC (p <0.05) [10].
Table 2: Q values of the nonparametric version of the Newman-Keuls test for pairwise comparison (differences are significant at Q> 2,242 (p <0.05).
Results And Discussion
Our data indicate that the technology of processing implants with powerful ion beams with carbon atoms in a mode allows cleaning the titanium surface from impurities located on it, in particular, hydrogen, aluminum and iron, which is clearly evidenced by the MRSA data. The PIB processing mode used in this work was chosen as the optimal one; preliminary studies of various PIB modes were carried out by us in [2]. It should be noted that after treatmenting with PIB, the surface area of the implant increases due to the acquisition of developed microroughness. However, in this work, we were unable to identify differences in osseointegration between implants of II (PIB) and III (acid etching) groups. To identify differences in osseointegration of these types of implants, additional in vivo studies that are longer in time and with a functional load on the implants. This approach will reveal the effect of migration of impurities from a titanium alloy through its surface over time. In addition, the processing of PIB implants is technologically safer than acid etching.
Conclusions
Surface treatment of dental implants made of VT1-0 alloy with powerful ion beams based on carbon atoms is a promising, hightech, and safe modification method that allows achieving 100% purity of the titanium surface. Primary osseointegration of dental implants after PIB treatment corresponds to generally accepted indicators.
References
- Gosteva EA, Dymnikov AB, Starkov VV, Sedlovets DM, Valikhov MP, et al. (2021) Interaction of Various Variants of the Nanostructured Surface of Titanium with MSCs Isolated from Adipose Tissue. Biomimetics 6(4): 61.
- Lang NP, Jepsen S (2009) Implant surfaces and design. Consensus report of working group 4. Clin Oral Implants 20(4): 228-231.
- Li Q, Wang Z (2020) Involvement of FAK/P38 Signaling Pathways in Mediating the Enhanced Osteogenesis Induced by Nano-Graphene Oxide Modification on Titanium Implant Surface. Int J Nanomedicine 15: 4659-4676.
- Yeo IL (2019) Modifications of Dental Implant Surfaces at the Micro- and Nano-Level for Enhanced Osseointegration. Materials (Basel) 13(1): 89.
- Labis VV, Bazikyan EA, Kozlov IG, Sizova SV, Khaidukov SV (2016) Nanoscale particles are participants in osseointegration. Bulletin of the Orenburg Scientific Center of the Ural Branch of the Russian Academy of Sciences 1: 1-18.
- Bormann KH, Gellrich NC, Kniha H, Schild S, Weingart D, Gahlert MA (2018) prospective clinical study to evaluate the performance of Zirconium dioxide dental implants in single-tooth edentulous area: 3-year follow-up 18(1): 181.
- Tarbokov VA, Pavlov SK, Remnev GE, Nochovnaya NA, Eshkulov UE (2018) Metallurg No 11: 80-84.
- Volkov AV, Shustrov SA, Korsanenkov KS, Nabieva EKh (2016) New painting method undecalcified bone tissue. Clinical and experimental morphology 4 (20): 55-58.
- Volkov AV, Smbatyan BS, Nazaryan DN, Muraev AA (2018) A new morphometric nomenclature for assessing osseointegration of intraosseous implants. Modern technologies in medicine. 10(3): 7-13.
- Bormann KH, Gellrich NC, Kniha H, Schild S, Weingart D, et al. (2018) Prospective clinical study to evaluate the performance of Zirconium dioxide dental implants in single-tooth edentulous area: 3-year follow-up. 18: 181.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...