
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5760
Case report(ISSN: 2690-5760) 
A COVID-19 Bilateral Peripheral Pneumonia in a Cirrhotic Patient; at Home Diverse Management; A Case Report Volume 2 - Issue 4
Yasser Mohammed Hassanain Elsayed*
- Critical Care Unit, Fraskour Central Hospital, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt
Received: November 10, 2020 Published: December 14, 2020
Corresponding author: Yasser Mohammed Hassanain Elsayed, Critical Care Unit, Fraskour Central Hospital, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt
DOI: 10.32474/JCCM.2020.02.000144
Abstract
Rationale: Coronavirus disease is an important serious pandemic worldwide infection. Anticoagulants and antiplatelet medication are essential drugs in the management of COVID-19 infection. Bleeding tendency is an anxious adverse effect for these drugs in hepatic patients. Patient concerns: An elderly male COVID-19 cirrhotic patient presented to physician outpatient clinic with bilateral peripheral pneumonia. Diagnosis: COVID-19 pneumonia in cirrhotic patient. Interventions: Electrocardiography, chest CT scan, and oxygenation. Outcomes: Gradual dramatic clinical, electrocardiographic, and radiological improvement had happened. Lessons: It denotes the role of the low dose of anticoagulants, the low dose of antiplatelets, steroids, and antimicrobial therapy in the management of COVID-19 pneumonia with liver cirrhosis. Using the lowest doses of anticoagulants, and antiplatelet was the choice to avoid bleeding tendency. The mild elevations in liver enzymes indication of mild hepatic injury. The fluctuations in the synthetic function of the liver including; S. albumen, total bilirubin, prothrombin time, and INR was within normal.
Keywords:COVID-19; Coronavirus; Peripheral pneumonia; Cirrhosis; At home diverse management
Abbreviations: CBC: Complete Blood Count; COVID-19: Coronavirus Disease 2019; ECG: Electrocardiography; IV: Intravenous; IVB: Intravenous Bolus; O2: Oxygen; POC: Physician Outpatient Clinic; SGOT: Serum Glutamic-Oxaloacetic Transaminase; SGPT: Serum Glutamic-Pyruvic Transaminase; VR: Ventricular Rate
Introduction
Coronaviruses family were at first discovered in the 1930s when
an acute chest infection of domestic chickens was appeared to be a
result of the infectious bronchitis virus (IBV) [1]. In December 2019,
series of case studies of acute respiratory illness, now named as a
new descent of coronavirus–infected pneumonia (NCIP) or atypical
viral pneumonia initially notified in Wuhan, Hubei Province, China
[2-4]. It was described as a coronavirus disease-2019 (COVID-19)
[2].
High levels of the virus in histopathological features that
have been found in the liver are signal for hepatic organotropism
of SARS-CoV-2 [5]. People with comorbidities (e.g. liver disease)
are at higher risk for severe COVID-19 illness [6,7]. Elevated liver
transaminases and abnormal liver function tests are one of the
most common laboratory abnormalities in COVID-19 patients
[8]. Essentially, the liver function tests (LFTs) includes alanine
transaminase (ALT or SGPT) and aspartate transaminase (AST or
SGOT), alkaline phosphatase (ALP), gamma-glutamyl transferase
(GGT), serum bilirubin, prothrombin time (PT), the international
normalized ratio (INR) and albumin are key in clinical management
[9]. These tests can be the main guide for hepatic injury and their
differential diagnosis (DD) [9]. Aminotransferases are markers of
hepatocellular (HC) injury [9]. Albumin is synthesized in the liver.
With any liver disease, there is a fall in serum albumin, indicating
reduced synthesis [9]. Prothrombin time (PT) estimates the
conversion rate of prothrombin to thrombin. Except for factor
VIII, all other coagulation factors are synthesized by the liver.
Prothrombin time needs coagulation factors II, V, VII, and X. They
are synthetic in the liver. They are pivotal in coagulation [9].
Hyperbilirubinemia is an increase in serum bilirubin levels above
the normal laboratory range which is mostly due to bilirubin
disorders. Hyperbilirubinemia can be classified as unconjugated or
conjugated. Unconjugated hyperbilirubinemia usually results from
increased production, impaired hepatic uptake, and decreased conjugation of bilirubin [10,11]. Alkaline phosphatase is mostly
increased in both cholestatic liver disease and bone disorder or
osteoblastic activity [9].
Case Presentation
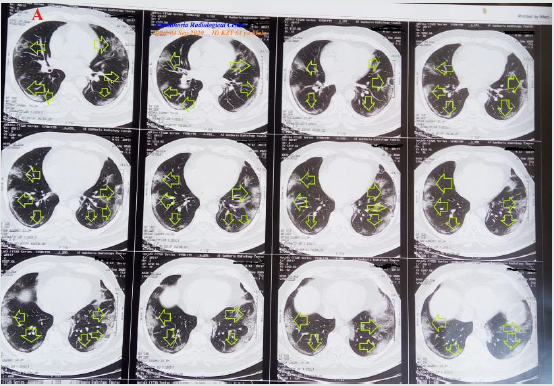
A 61-year-old married, farmer, Egyptian male patient presented to the Physician Outpatient Clinic (POC) with acute tachypnea, fever, and cough. Fatigue, anorexia, and dizziness were initial associated symptoms. He gave a history of fever for 3 days hours. The patient has an old history of liver cirrhosis. He also gave a recent history of contact with confirmed COVID-19 patient in the past 14 days. Upon general physical examination; generally, the patient was tachypneic, irritable, with a regular tachycardia of VR 110 bpm, blood pressure of 90/70 mmHg, respiratory rate of 34 bpm, the temperature of 40.2°C, and pulse oximeter of oxygen (O2) saturation of 91 %. No more relevant clinical data were noted during the clinical examination. He had managed at home as COVID-19 pneumonia in a cirrhotic patient. Initially, the patient was treated with O2 inhalation by O2 cylinder (100%, by nasal cannula, 5L/ min). Ringer solution (500 ml over 30 minutes) was immediately given. The patient was maintain treated with SC enoxaparin 20 mg twice daily), aspirin tablet (75 mg, once daily), clopidogrel tablet (75 mg, once daily), cefotaxime; (1000 mg IV every 8hours), azithromycin (500 mg PO single daily dose on the day one, followed by 250 mg PO daily on for 5 days), oseltamivir (75 mg PO twice daily only for 5 days), hydrocortisone sod succinate (100 mg IV every 8 hours), and paracetamol (500 mg IV every 8 hours as needed). The patient was monitored for temperature and blood pressure. The initial ECG on presentation showing sinus tachycardia with VR of 110 (Figure 1A). The initial complete blood count (CBC); Hb was 13.7 g/dl, RBCs; 5.18*103/mm3, WBCs; 6.1*103/mm3 (Neutrophils; 76.9 %, Lymphocytes: 17.8%, Monocytes; 5.3), Platelets; 96*103/ mm3. Measured random blood sugar was; 111 mg/dl. S. Ferritin was high; 291 ng/ml. D-dimer was normal (370 ng/ml). The initial CRP was high; 75.6 g/dl. SGPT was high; 63U/L, SGOT was high; 94 U/L, alkaline phosphatase (ALP);76 U/l, S. albumen;4.7 g/dl, total bilirubin; 0.3 mg/dl, Prothrombin time;13 sec., and INR; 1.2. Serum creatinine; 0.9 mg/dl and blood urea;34 mg/dl. In the on the fifth day of management; CBC; Hb was 11 g/dl, RBCs; 4.21*103/mm3, WBCs; 4.4*103/mm3 (Neutrophils; 49.7 %, Lymphocytes: 26.2%, Monocytes; 24.1%), Platelets; 126*103/mm3. CRP was; 8.12 g/dl. SGPT; 38 U/L, SGOT; 66 U/L, alkaline phosphatase (ALP);99 U/l, S. albumen;4.2 g/dl, total bilirubin; 0.7 mg/dl, Prothrombin time;12 sec., and INR; 1.3. Serum creatinine; 0.87 mg/dl, and blood urea; 36 mg/dl. In the on the tenth day of management; CBC; Hb was 12.2 g/dl, RBCs; 4.57*103/mm3,WBCs; 6.1*103/mm3 (Neutrophils; 58.6 %, Lymphocytes: 26.8 %, Monocytes; 14.6%,), Platelets; 119*103/ mm3. S. Ferritin was high; 152 ng/ml. D-dimer was normal (380 ng/ml). CRP was; 1.02g/dl. SGPT; 32 U/L, SGOT; 50.4 U/L, alkaline phosphatase (ALP);106 U/l, S. albumen;4.3 g/dl, total bilirubin; 0.1 mg/dl, Prothrombin time;13 sec., and INR; 1.1. S. creatinine was; 0.71 mg/dl and blood urea; 29 mg/dl. The first radiological films were done on the day of presentation: Plain Chest imaging showing peripheral bilateral ground-glass pulmonary consolidations (Figure 2). Chest CT scan showing peripheral bilateral lungs ground-glass consolidations (Figure 3A). The last radiological film was done on the second day of admission; a Chest CT scan was done within 14 presentations showing nearly dramatic improvement of the above ground-glass pulmonary consolidations (Figure 3B). Echocardiography was normal. COVID-19 pneumonia in a cirrhotic patient was the most probable diagnosis. ECG tracing was taken within 20 days of treatment showing normal sinus rhythm with VR of 85 (Figure 1B). Within 14 days of the above management, the patient finally showed complete clinical, radiological, and laboratory improvement.
Figure 1: Serial ECG tracings; A. tracing was the initial ECG on presentation showing sinus tachycardia with VR of 110. B. tracing was taken within 20 days of treatment showing normal sinus rhythm with VR of 85.

Figure 2:First film: 2A1. Plain Chest imaging on the day of the presentation showing peripheral bilateral ground-glass pulmonary consolidations (lime arrows).
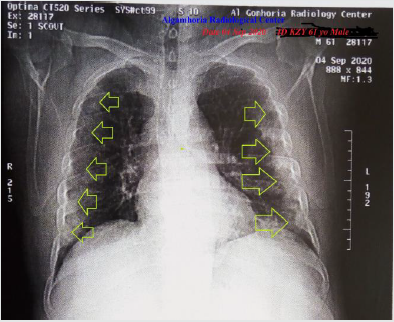
Figure 3: A. chest CT scan was done on presentation showing peripheral bilateral ground-glass pulmonary consolidations (lime arrows) B. chest CT scan was done within 14 presentation showing nearly dramatic improvement of the above groundglass consolidations.
Discussion
Overview
a) An elderly male COVID-19 cirrhotic patient presented
to a physician outpatient clinic with bilateral peripheral
pneumonia.
b) The objective primary for my case study was the presence of
bilateral peripheral pneumonia in a COVID-19 cirrhotic patient
in an outpatient clinic.
c) The secondary objective for my case study was the question of;
How did you manage the case?
d) There was a history of direct contact to confirmed the
COVID-19 case.
e) The presence of direct contact to confirmed the COVID-19 case,
bilateral peripheral ground-glass extensive consolidation, and
lymphocytopenia on top of fever, tachypnea, and dry cough
will be supporting the COVID-19 diagnosis.
f) The tachypnea, sinus tachycardia, hypoxia, consolidation,
and elevated d-dimer are highly suggestive of associated
pulmonary embolism.
g) Hyperthermia with hypotension on the case presentation
may be interpreted by the presence of septic shock (due to
pneumonia).
h) The conversion sinus tachycardia normal sinus rhythm in ECG
after clinical improvement was marked.
i) The blood pressure normalization urgently after fluid IV
infusion with the maintenance of the effects of anti-infective
drugs, anticoagulants, and antiplatelet had avoided the need
for vasopressors e.g. norepinephrine IV infusion.
j) Using the lowest doses of anticoagulants and antiplatelet was
the preference to avoid bleeding tendency.
k) The mild elevations in liver enzymes indication of mild hepatic
injury.
l) The fluctuations in the synthetic function of the liver including;
S. albumen, total bilirubin, prothrombin time, and INR was
within normal.
m) It signifying the role of anti-infective drugs, anticoagulants,
and antiplatelet role in COVID-19.
n) The presence of sinus tachycardia indicate either; fever shock
or pulmonary embolism.
o) Blood pressure, respiratory rate, and O2 saturation are a
strong guide for clinical follow-up in COVID-19 patients.
p) A gradual decreasing the level of elevated CRP, lymphocytic
count, liver enzymes, and CT chest may be used as another
good laboratory guide for follow up in COVID-19 patients.
q) The serial change of radiological changes from normal chest
CT to abnormal to normal at the end will strengthen the used
medications in this effective management. Also, it gives a good
radiological impact for follow up.
r) I can’t compare the current case with similar conditions. There
are no similar or known cases with the same management for
near comparison.
Limitations of the study
There are no known limitations to the study
Conclusion and Recommendations
a) The using the lowest doses of anticoagulants and antiplatelet
in hepatic impairment are an essential choice to avoid the
bleeding tendency.
b) The fluctuations in the synthetic function of the liver including;
S. albumen, total bilirubin, prothrombin time, and INR is
insignificant.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
I wish to thanks my wife to save time and improving the conditions for helping me.
References
- Estola T (1970) Coronaviruses, a New Group of Animal RNA Viruses. Avian Diseases 14 (2): 330–336.
- Mitra M (2020) Antigen and antibody for Coronavirus RNA Vaccination Development. Op Acc J Bio Sci & Res 1(1).
- Rajan R, Jarallah MAI, Dashti R (2020) Cardiovascular complications of novel Wuhan Coronavirus (COVID-19) – A 2020 update. J Cardiol Curr Res 13(1): 28.
- Wang D, Hu B, Hu C, et al (2020) Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA 323(11): 1061–1069.
- Puelles VG, Lütgehetmann M, Lindenmeyer MT, Sperhake JP, Wong MN, Allweiss L, et al (2020) Multiorgan and Renal Tropism of SARS-CoV-2. N Engl J Med 383(6): 590-592.
- Centers for Disease Control and Prevention (2020) People at Increased Risk And Other People Who Need to Take Extra Precautions.
- CDC COVID-19 Response Team (2020) Preliminary Estimates of the Prevalence of Selected Underlying Health Conditions Among Patients with Coronavirus Disease 2019 - United States, February. MMWR Morb Mortal Wkly Rep 69(13): 382-386.
- Cai Q, Huang D, Yu H, Zhu Z, Xia Z, Su Y, et al (2020) COVID-19: Abnormal liver function tests. J Hepatol 73(3): 566-574.
- Lala V, Goyal A, Bansal P, Minter DA (2020) Liver Function Tests.
- Fargo MV, Grogan SP, Saguil A (2017) Evaluation of Jaundice in Adults. Am Fam Physician 95(3): 164-168.
- Roche SP, Kobos R (2004) Jaundice in the adult patient. Am Fam Physician. 69(2): 299-304.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




