Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1403
Research Article(ISSN: 2644-1403) 
The Effect of Adding Magnesium to Bupivacaine as an Adjuvant in Continuous Pectoralis Nerve II (PECs) Block in Simple Mastectomy Volume 2 - Issue 5
Eman M Kamal Abo Seif, Walid Y Kamel and Amr M Hilal Abdou*
- Department of Anesthesia, Ain Shams University, Egypt
Received: February 10, 2020; Published: February 20, 2020
Corresponding author: Amr M Hilal Abdou, Department of anesthesia and intensive care. Ain Shams University, Egypt
DOI: 10.32474/GJAPM.2020.02.000148
Abstract
Background and Aim: Breast surgeries are associated with post-operative pain and restricted shoulder mobility, so the aim of this study is to assess the analgesic efficiency and safety of Continuous Pectorals II (PECs) block by adding magnesium to bupivacaine as an adjuvant versus bupivacaine as a sole agent in cases of simple mastectomy.
Patients and Methods: This randomized double blinded study designed to compare the analgesics efficacy and safety of continuous PECs II using bupivacaine versus continuous PEC II using bupivacaine plus magnesium in patients undergoing simple mastectomy and postoperative period. We enrolled 40 adult females ASA I-II patients’ candidates for simple mastectomy without axillary clearance. All patients were randomly distributed into two groups. Control group: prior to surgical incision patients had ultrasound guided PEC II continuous block with 10ml plain bupivacaine 0.25% plus followed by infusion of 8ml normal saline per hour. Magnesium group: patients were given 10ml plain bupivacaine 0.25% plus 0.5 gm (5ml) magnesium sulfate followed by infusion of 0.25% plain bupivacaine 7ml/h. plus 10 mg (1 ml) magnesium sulfate infusion per hr.
Results: For assessment of the postoperative pain scores by the VAS; our results showed significant reduction in the magnesium group (P<0.001) in comparison with control group. Intraoperative vital data in the form of heart rate (HR) and mean arterial blood pressure (MAP) showed highly significant decrease of the heart rate in the magnesium group (P≤0.001) after 30 minutes from the block till 2 hours after the block compared to the control group, in addition to significant decrease in MAP (P = 0.036) after the block by 30 minutes. Postoperative vitals showed significant decrease of HR (P=0.016) in magnesium group 4 hours after surgery till the following day, highly significant decrease in RR (P <0.001).
Conclusion: This clinical study proven that mixing of magnesium sulphate to bupivacaine during PECs II block provided a solid safe prolonged motor and sensory block, besides the reduction of postoperative additional rescue pain medications and pain scores.
Introduction
Acute postoperative pain and shoulder immobility is a usual
complication following breast surgeries. Many technique are used
to reduce the postoperative pain, thoracic paravertebral block
(TPVB) is the most widely used technique to provide postoperative
analgesia but it does not block medial and lateral pectoral nerves
effectively with risk of spinal cord trauma, pneumothorax and
sympathetic block [1]. Blocking the pectoral nerve (PEC I) provides
intraoperative and postoperative pain control during breast surgery.
The Pec I block is a superficial block that has been used effectively.
The PECs II block is more effective and used widely now because
it blocks also the long thoracic and the thoraco-dorsal nerves in
addition to the lateral branches of the intercostals nerves that
present at the level of the mid axillary line innervating mammary
gland and T2 to T6 overlying skin [2]. To achieve adequate PECs
II block Local anesthetic should be infiltrated under the Pectoralis
minor muscle between the Clavi-pectoral fascia and the superficial
border of the serratus muscle thus covering the pectoral region with
the pectoral nerves and the intercostals branches [3].The block is
done in supine position and the arm either abducted 90 degrees
or by the patient’s side. Injecting the anterior axillary line at the
level of the fourth rib 3-6 cm in depth with the transducer of the ultrasound machine at the mid clavicular level and angled inferolaterally
after identifying the axillary artery, vein and the second rib
[4]. The transducer then is moved lateral until the Pectoralis minor
and serratus anterior are identified, the local anesthetic is injected
between the two muscles. For continuous PECs II bock, a catheter is
inserted in the fascial plane and positioned to ensure intraoperative
and postoperative pain control [5].
Bupivacaine is an amide local anesthetic with a slow onset,
long duration of action and high potency. Bupivacaine has a
toxicity profile among the worst of the amide local anesthetic, the
maximum recommended single bolus dose of bupivacaine is 2.5
mg/Kg, it is metabolized in the liver by human cytochrome P450
(CYP) and the metabolites are non-toxic by the CYP3A4 in an
oxidative metabolism fashion. Bupivacaine exert its action through
impairing sodium influx across the neuronal membrane by blocking
the sodium channels. Magnesium is the second most common
intracellular cation after potassium. It acts as co-factor in more than
300 enzymatic reactions and also involved in several processes as
neurotransmitter release, cardiac excitability, neuronal activity and
control or vasomotor tone [6]. The total normal serum Mg+2 levels
is in the range of 1.8 to 3ml/dl. The sole route of elimination of
Mg2+ is by renal clearance. Magnesium has a depressant action on
the central nervous system and has been used as an anticonvulsant
[7]. The mechanism of action is related to competition with calcium
in the processes of transmitter release which leads to pre-synaptic
inhibition of acetylcholine release at the neuromuscular function.
It also exerts its analgesic action through blocking N-methyl-D
aspirate (NMDA) receptors [8]. Mg2+ potentiates the action of local
anesthetics (LA) in the peripheral nerves by elevating the firing
threshold in both myelinated and unmyelinated axons increasing
the transmembrane potential causing hyperpolarization [9]
addition of magnesium to bupivacaine can result in an enhancement
of nerve blocking.
Methodology
Following approval from our faculty ethical committee and obtained written informed consent from the patients, we enrolled 40 adult females ASA I-II scheduled for simple mastectomy in this randomized double blinded study. All patients were randomly assigned to one of two groups. Patients known to be allergic to local anesthetics, or diagnosed with coagulopathy or on anticoagulant therapy, or having skin infection at the injection site are excluded from this study. Control group: prior to surgical incision patients had ultrasound guided continuous PECs II block and injected with 10 ml plain bupivacaine 0.25% plus 8 ml normal saline per hr. Magnesium group; Patients had ultrasound guided continuous PECs II block and injected 10 ml plain bupivacaine 0.25% plus 0.5 gm (5 ml) magnesium sulphate, followed by infusion of 0.25% plain bupivacaine 7 ml/hr. plus 10 mg (1 ml) magnesium sulphate infusion per hour.
Anesthetic Management
History and preoperative assessment were done for all patients of the two groups. Full preoperative profile with coagulation investigations was done. Patient education on evaluation of the intensity of pain via the visual analog scale (VAS), scored from 0-10 (where 0=no pain and 10=worst pain). All patients had the same premedication such as Midazolam 0.1 mg/kg. Standard monitors were applied for all patients. Conventional general anesthesia with Propofol and fentanyl 1- mcg/kg and atracurium 0.5 mg /kg were standardized for all patients.
PECs II Block Technique
While patient is in supine position either with abducted arm 90 degrees or beside the patient. Injection done at fourth rib’s level anterior axillary line, under ultrasound guidance (Sonosite M-Turbo, USA) The depth was adjusted to 3-6 cm with the transducer at the midclavicular level and angled infero-laterally the transducer was then moved laterally to identify the Pectoralis minor and serratus anterior. The local anesthetic was injected between the last two muscles, followed by insertion of a B Braun catheter kit Periflix (B. Braun Melsungen AG, Germany) with an 18 gauge needle in the fascial plane was done to insure continuous PECs II block for the operative and postoperative pain control. Intraoperative analgesic control was maintained by Fentanyl 1 mcg/kg if there was heart rate or blood pressure elevation more than 20% of the baseline, concerning the postoperative analgesia VAS was assessed first if more than 5; Morphine bolus 0.1mg/kg was given.
Collected Data
Heart rate and mean blood pressure were assessed before induction of anesthesia then 15 minutes after the block then every 15 minutes till the end of surgery, respiratory rate values were recorded for the first 24 hours postoperatively every 2 hours, all the previous variables were added to the VAS score, time of first analgesic dose and total morphine dosage given for the first 24hr after surgery.
Statistical Analysis
For each patient, results were calculated from baseline values and were considered for comparison between the groups. All results are described as mean ±SE. comparison were made using the student’s t-test, the Mann-Whitney U-test or Chi square test. The threshold for statistical significance was taken as P<0.05. Randomization was done using a computer-generated sequence. Concealment was achieved using opaque envelopes.
Results
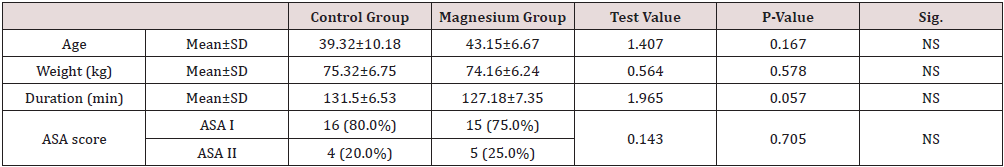
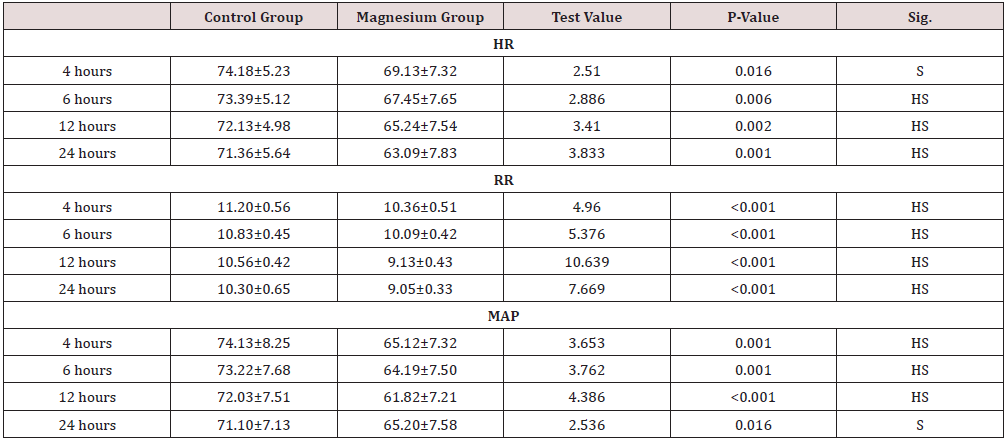
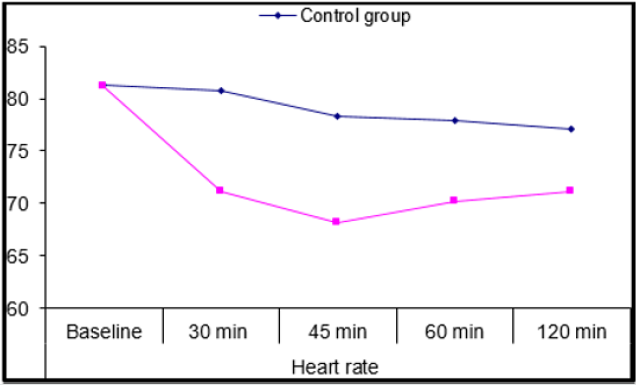
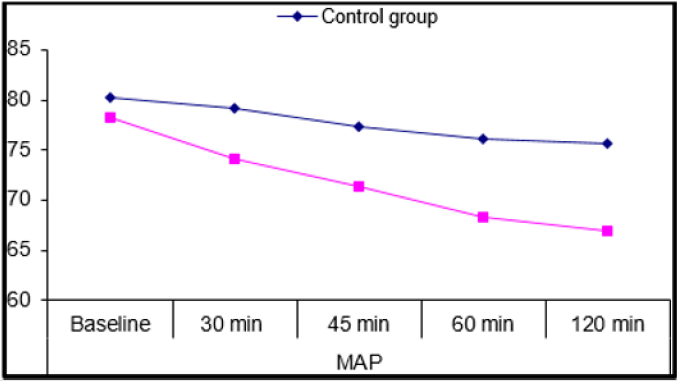
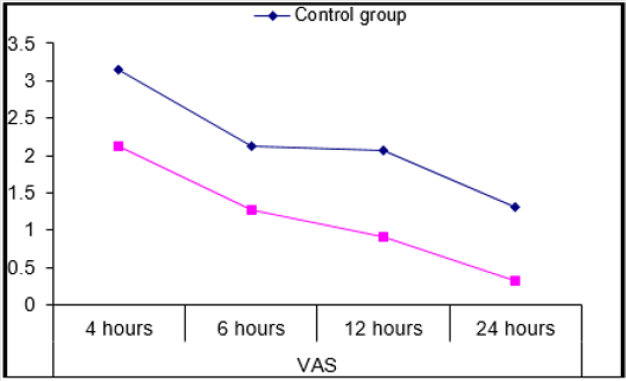
Forty adult females 31 of them were ASA I, 9 of them were ASA II were recruited for simple mastectomy then randomly divided into control group and magnesium group of average duration (Mean±SD) of surgery 131.5±6.53 and 127.1±7.35, The demographic data Table 1 as regards age, weight, Duration of surgery and ASA score showed no significant difference (P=0.167, 0.578, 0.057, and 0.705) respectively. 2(10%) cases in the control group required intraoperative fentanyl doses and no (0.0%) cases took any fentanyl in the magnesium group. Intraoperative vital data in the form of heart rate (HR) and mean arterial blood pressure (MAP) (Figures 1&2) showed highly significant decrease of the heart rate in the magnesium group (P≤0.001) after 30 minutes from the block till 2 hours after the block compared to the control group, in addition to significant decrease in MAP (P = 0.036) also 30 minutes after the block. Postoperative vitals Table 2 showed significant decrease of HR (P=0.016) in magnesium group 4 hours after surgery till the following day, highly significant decrease in RR (P <0.001) with no detected complications such as ICU admission or Oxygen therapy, SPO2 measurements were normal in any group for the first day following surgery. With respect to the postoperative MAP there was highly significant (P=0.001) decrease towards the magnesium group. For assessment of the postoperative pain scores by the VAS; our results (Figure 3) showed highly significant decrease in the magnesium group (P <0.001) when compared to the control group.
Discussion
Many types of regional methods such as intercostal nerve blocks, epidural block and paravertebral nerve block have been used for controlling postoperative pain following breast surgeries [10]. Pectoral nerve block is a technique first done by Blanco in 2011; after one year he modified the block into a second version (Modified peck block=PECs II) aiming to block the axilla and the intercostals nerve [11]. This study compared the analgesics effectiveness and safety of continuous PECs II using bupivacaine versus continuous PECs II using bupivacaine plus magnesium in patients had breast lumpectomy both for pain control during and after the surgery. The results showed that there was a good control for intra and postoperative data regarding hemodynamics (mean arterial blood pressure and pulse rate), the results also showed a decrease in intraoperative consumption of fentanyl. Postoperative score of pain was more in the control group comparing to the magnesium group, and none of the patients requested for rescue analgesia in the postoperative day. In contrast to the results of this study, Hung et al. [12] studied the magnesium sulfate effect on amide LA in sciatic nerve block and concluded that magnesium (Mg) shortens the sciatic nerve block duration so it does not seem to be useful as adjuvant in peripheral nerve block. However, Bondok and her colleagues [13] studied the effect of injection of magnesium in the knee in arthroscopy procedure, and proved that this technique resulted in a significant reduction in the postoperative VAS in the first 24hrs in addition to significant decrease in the dose of postoperative analgesics. Furthermore, Kashedi et al. [14] compared the effect of analgesia of Mg plus Lidocaine, paracetamol plus Lidocaine and placebo plus Lidocaine on block characteristic for intravenous regional anesthesia (IVRA) in patients undergoing upper extremity orthopedic surgery: it was found that time from drug injection to sensory block onset was the shortest in the magnesium plus Lidocaine group. The duration of the motor block was prolonged in the Lidocaine plus Mg group.
Conclusion
This clinical study proven that mixing of magnesium sulphate to bupivacaine during PECs II block provided a solid safe prolonged motor and sensory block, besides the reduction of postoperative additional rescue pain medications and pain scores.
Conflict of interest
Nothing to disclose.
Author’s Contribution
We Dr E.K.A/A.M.A/W.Y.K hereby declare that the article has not been published or submitted to or accepted for publication in any form in any other journal. I vouch that the authorship of this manuscript will not be contested by anyone whose names are not listed. On acceptance the article will become the copyright of Journal. All Authors has read and approved this manuscript.
References
- Lin N, Yu B, Hung C (2016) Paravertebral Block Plus Thoracic Wall Block Versus Paravertebral Block Alone for Analgesia of Modified Radical Mastectomy: A Retrospective Cohort Study. PLoS One11(11): e0166227.
- Kulhari S, Bharti N, Bala I, Arora S, Singh G (2016) Efficacy of Pectoral Nerve Block Versus Thoracic Paravertebral Block for Postoperative Analgesia After Radical Mastectomy: A Randomized Controlled Trial. BJA 117(3): 382-386.
- Womack J, Varma M (2014)SeratusPlane Block for Shoulder Surgery. Anaesthesia 69(4):395-396.
- fujiwara A, Komasawa n, Minami T (2014) Pectoral Nerves (pecs) and Intercostals Nerve Block for Cardiac Resynchronization Therapy Device Implantation. Springerplus3: 409.
- Blanco R, Fajardo M, Maldonado T (2012) Ultrasound Description of Pecs Ii (Modified Pecs I): Noval Approach to Breast Surgery. Rev EspAnestesiolReanim 59(9): 470-475.
- Ramamurthi R, Krane J Elliot (2007) Local Anesthetic Pharmacology in Pediatric Anesthesia. Techniques in Regional Anesthesia and Pain Management 11(4): 229-234.
- Dube L, Granry J (2003) The Therapeutic Use of Magnesium in Anesthesiology, Intensive Care and Emergency Medicine: A Review. Can J Anesth Can D Anesthésie50(7): 732-746.
- Blaine J, Chonchol M, Levi M (2015) Renal control Of Calcium Phosphate and Magnesium Homeostasis. Clin J Am Soc Nephrol 10(7): 1257-1272.
- de Baaij J, Hoenderop J, Bindels R (2012) Regulation of Magnesium Balance: Lessons Learned from Human Genetic Disease. Clin Kidney J 5: i15-i24.
- Song W, Chang Y (2012) Magnesium Sulfate for AcuteAsthma in Adults: A Systematic Literature Review. Asia Pac Allergy 2(1): 76-85.
- Lynch E, Welch K, Caraduena J (1995)Thoracic Epidural Anesthesia Improves Outcome After Breast Surgery. Ann Surg 222: 663-669.
- Hung Y, Chen C, Lirk P, Wang CF, Cheng JK et al. (2007) Magnesium Sulphate Diminishes the Effects of Amide Local Anesthetics in Rat Sciatic Nerve Block. REG Anesth Pain Med 32: 288-295.
- Bondok R, Abd El-Hady A (2006) Intra-Articular Magnesium Is Effective for Postoperative Analgesia in Arthroscopic Knee Surgery. Br j anesth 97(3): 389-392.
- Kashefi P,Montazeri K (2008)Adding Magnesium Sulphate to Lidocaine of Intravenous Regional Anesthesia. JrnlResAnesht Pain Med 33(5): 97.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...