Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1403
Research Article(ISSN: 2644-1403) 
Radiofrequency Ablation for the Treatment of Chronic Lumbar Facets Arthropathy; Bipolar Radiofrequency at Two Points Versus Monopolar Radiofrequency at One Point - A Randomized Control Trial Volume 1 - Issue 4
Wael M Abdelkhalek1, Mohamed M Hashim2, Adel M Shaaban3 and Dhafir A Alkhudairi4*
- 1Senior registrar of Anaesthesia & Pain management, King Hamad University Hospital, Bahrain
- 2Lecturer of Anaesthesia, ICU and Pain management, faculty of medicine, Cairo university, Egypt
- 3Specialist Anaesthesia and Pain management, Middle East Hospital, Bahrain
- 4Head, Department of Anaesthesia, consultant of anaesthesia and Pain management, King Hamad University Hospital, Kingdom of Bahrain
Received: May 30, 2019; Published: June 07, 2019
Corresponding author: Dhafir A Alkhudairi, Department of Anaesthesia, King Hamad University Hospital, Kingdom of Bahrain
DOI: 10.32474/GJAPM.2019.01.000118
Abstract
Background: Radiofrequency (RF) ablation has reported variable results in the treatment of facet joint pain; therefore, more robust evidence for RF ablation for the management of facet joint pain is needed to establish the optimum. This study compares the effectiveness of two different techniques of applying RF ablation, monopolar vs bipolar, to the medial branch of the dorsal nerve.
Methods: After diagnostic facet joint injection with lidocaine 2%, patients who demonstrated an improvement in Visual Analogue Scale (VAS) score of more than 50%, were divided into two groups with a total 50 subjects (25patients in each group). Group 1 would receive monopolar RF at one point, group 2 would receive bipolar RF at 2 points. The patients in each group were evaluated in 2 weeks, 1 month, 3 months and 6 months’ intervals, using the VAS score. Overall patient satisfaction was evaluated by the patient satisfaction score.
Results: There was no significant difference in VAS score between the groups (‘between subject test’ p = 0.224). The median initial pain score was 8 [8-10] and was comparable between group one and group two (9 [8-10] and 8 [8-10], respectively; p = 0.338). The patient satisfaction score was comparable between group one, and two (6 [5-7] and 7 [5-8], respectively; p = 0.170).
Conclusions: The use of bipolar technique in comparison to Monopolar technique for RF neurotomy of the medial branch of the dorsal nerve did not add more benefits to the patients in decreasing pain scores at different timings.
Keywords: Back Pain; Facet Joint Arthropathy; Medial Branch Radiofrequency; Radio Frequency Ablation; Treatment; Zygapophyseal Joint
Introduction
Therapeutic interventions for lumbar facet joint arthropathy are performed to provide long-term pain relief, after the facet joint has been identified as the generator for the low back pain. The therapeutic interventions generally used for the treatment of low back pain, of facet joint origin, include intra-articular facet joint injections, lumbar facet joint nerve blocks and RF neurotomy [1- 3]. RF ablation is widely used in the treatment of chronic pain for its efficacy and low incidence of side effects and complications [4]. RF ablation is a procedure, which incorporates heat to interrupt pain signals travelling through spinal nerves and is considered as a promising treatment option for chronic low back pain [5]. The results of RF ablation as a treatment for the lumbar facets arthropathy are still lacking a strong evidence which might be due to the variable and extensive nerve supply of the facet joints [6]. The need to find a more effective and long-lasting technique in the management of the pain originating from lumbar facet joints is required. Modification of the RF ablation techniques which are currently used may have good results in the treatment of low back pain caused by facet joint pathologies.
Materials and Methods
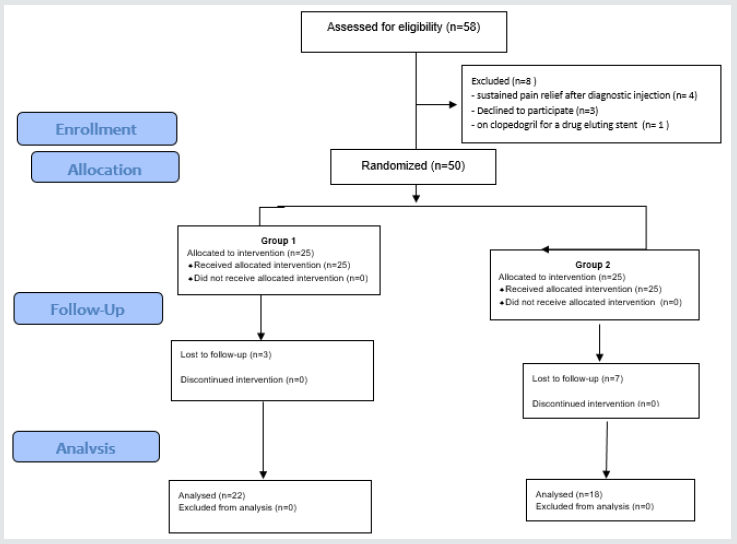
The study was conducted in King Hamad University Hospital (KHUH)–Muharraq–Bahrain. The Study was approved by the ethics committee of KHUH and a written consent was obtained from all patients participating in the study. The study is registered in ClinicalTrials.gov: ACTRN12615000426583. This study is a pilot study, as there is no identifiable literature directly comparing the efficacy of the two RF ablation techniques in the treatment of lumbar facet related pain. The duration of the study was six months for each patient. All patients with low back pain, aged 18 years and above, who had a pain score from moderate to severe (VAS more than 4) for a period which exceeds six months, with positive tenderness over facet joints, were included. Additional inclusion criteria were: pain that is resistant to the conventional treatment such as: medications, exercise and physiotherapy, degree of improvement in pain score exceeding 50% after diagnostic injection of local anaesthetic, except patients who had constant pain relief. Patients were excluded if they refused to proceed with the RF technique, or did not want to share in the study, presence of coagulopathy or were on therapeutic dose of anti-coagulants (aspirin is excluded), presence of red flags (fracture, tumor, focal neurologic signs, etc.), or infection at the site of injection. All the included patients in the study were examined in the pain clinic, experienced pain specialists performed all interventions. The patients received injections of ml of lidocaine 2% in the facet joints, using fluoroscopy. Patients with a decrease in the VAS score by ≥50 % were reviewed after 2 weeks. Additionally, patients who had constant improvement, and patients who had a pain score decreased < 50%, were excluded from the study. All the patients that participated in the study were randomized according to a ‘’closed envelope technique’’. Twentyfive patients were in each group.
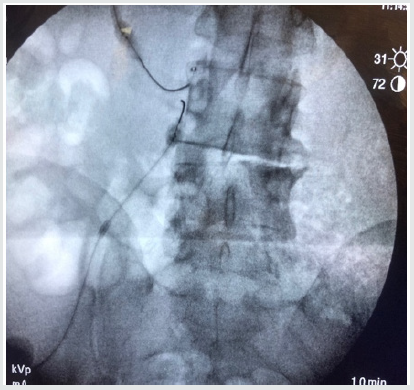
A. Group 1: Treatment with monopolar RF ablation at one point, Needle was inserted perpendicular at the upper part of the base of the transverse process at the corresponding vertebrae. After sensory and motor stimulation, 1ml of lidocaine 2% was administered through the RF needle before commencing monopolar RF ablation at 80oc for 90 sec (Figure 1).
B. Group 2: Treatment with bipolar RF at two points, 1st needle was inserted at the upper part of the base of the transverse process and the other needle was inserted below the 1st needle at the lower part of the base of the transverse process (10mm apart). After sensory and motor stimulation, 1ml of lidocaine 2 % was administered through the RF needle before starting bipolar lesion RF at 80oc for 90 sec (Figures 2 & 3). All procedures were performed under fluoroscopic guidance, with the use of Cosman RF generator G4TM, 20 gauge straight sharp cannula, 10cm shaft, 10mm tip and 10cm electrodes (Cosman autoclavable CSK-TC10(All patients received Paracetamol 1g orally every 6 hours and diclofenac 50mg orally, every 8 hours, if needed, for 4 days following the procedure. After the radiofrequency procedure, all patients had regular followup at the pain clinic, and their VAS score was assessed at 2 weeks, one month, 3 months and 6 months’ interval. The follow-up was at the pain clinic and was conducted by a specialized nurse, who was unaware of the treatment modality. The patient satisfaction for the pain relief was evaluated after 6 months by a Likert Satisfaction Scale [7].
C. 1: Very unsatisfied, 2: Unsatisfied, 3: Neutral, 4: Satisfied and 5: Very satisfied.
Statistical Analysis
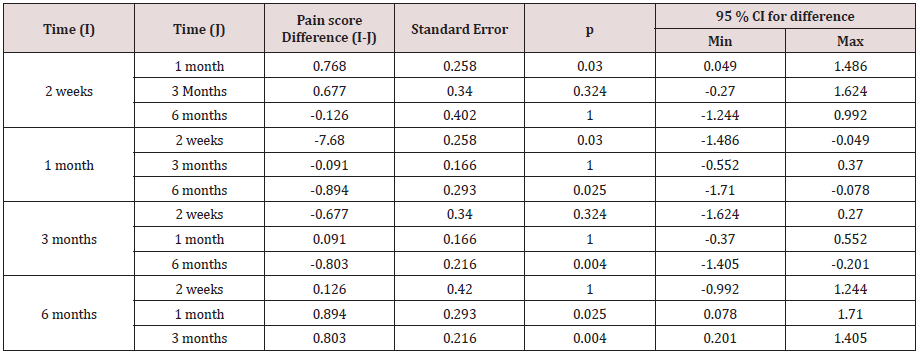
Statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) (version 20). Qualitative variables were expressed as percentages, and compared using χ2 test, or exact fisher test as appropriate. The normal distribution of all the quantitative variables was assessed by the Shapiro-Wilk test and Kolmogorov-Smirnov test. Quantitative data were expressed as mean ± standard-deviation (SD) or median [Quartiles] as appropriate. Two groups were compared (group 1 and group 2). The initial pain score, and the patient’s satisfaction score after completing the full course of treatment were compared by using Student’s test, or Mann-Whitney test as appropriate. Repeated analysis of variance was performed to compare the pain score over time between the two groups (after 2 weeks, one month, three months and six months). Therefore, within-subject variables were assessed according to 4 levels, whereas between-subject variables were assessed on two levels. The sphericity was assessed by Mauchly’s test. Greenhouse Geisser adjustments were considered for analysis that did not meet Mauchly’s test of sphericity. A posthoc analysis was then performed using the Bonferroni test. A twosided p value < 0.05 was considered as statistically significant.
Results
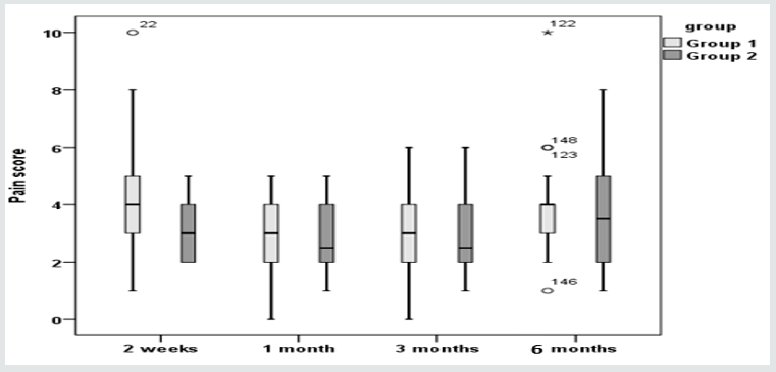
Fifty patients were included in the study (Figure 3). The age, weight and sex of the patients were compared between group 1 and group 2 (Table 1). The median initial pain score was 8[8-10] and was comparable between group 1 and group 2 (respectively 9[8-10] and 8 [8-10]; p=0.338). The sphericity was checked with Mauchly’s test after Greenhouse-Geisser correction (p=0.599). The pain score values recorded at 2 weeks, 1 month, 3 months and 6 months in both groups are summarized in Figure 4. Repeated analysis of variance showed that there was a significant difference within subjects over time (p=0.012). The post-hoc analysis showed that the pain score after 1 month was significantly lower than the pain score recorded after 2 weeks (p=0.030). However, the pain score after 6 months was significantly higher than the scores recorded at 1 month and 3 months (p value respectively 0.025 and 0.004) (Table 2). Moreover, repeated analysis of variance did not show significant differences between group 1 and group 2 (‘’between subject test’’=0.224). Similarly, the patient satisfaction score was comparable between group 1 and group 2 (6 [5-7] and 7 [5-8], respectively; p = 0.170).
NB: Sex-ratio in both groups is 1:1Footnotes: CI: Confidence interval
Discussion
Low back pain may arise from diversity of origins, including, but not limited to lumbar facet arthropathy, intervertebral lumbar discs and sacroiliac joint arthropathy. Facet joint arthropathy usually originates from segmental disc degeneration and frequent biomechanical stresses, which lead to inflammation around the synovial joints, including soft tissues and bone [5,8,9]. The dorsal ramus divides within the transverse ligament, to the medial and lateral branches. The medial branch of the dorsal ramus runs in a canal (fibro-osseous canal), which is bounded by the accessory process, the mammillary process, and the mammillo-accessory ligament. This canal is used as a target for neurotomy of the medial branch. The accessory process is difficult to visualize in x-ray films, the junction between the lateral surface of the superior articular process and the base of the transverse process is targeted for neurotomy [10]. Each medial branch from L1 to L4 supplies the zygapophyseal joint at the corresponding level, and the zygapophyseal joint at one level below, except the medial branch of L5 which supplies the zygapophyseal joint between the sacrum and L5 vertebra [11]. The standard treatment of the zygapophyseal joint is intra-articular injection of corticosteroids, or RF ablation of the medial branch, which supplies the joint. RF ablation is a commonly used technique for the treatment of chronic facet arthropathy, especially when other conservative treatments fail to produce adequate improvement [12-14]. Binder et al. [15] found in a study, that medial branch neurotomy for the treatment of chronic facet arthropathy is a promising treatment, but until now, there is a lack of evidence that supports this technique, mostly due to insufficiently powered randomized controlled trials. Physiological effects and physics of radiofrequency current have been discussed broadly, which lead to production of different electrodes with variations at the tips and parameters of the stimulation, aiming to improve the results when using the RF technique [16,17]. It was recommended by Van et al. [18] in 2012, that there is no need to repeat the diagnostic block due to the low incidence of the side effects of the RF neurotomy. This study found that RF neurotomy of the medial branch of the dorsal nerve has been reported as an efficient procedure with clear evidence which was supported by many controlled trials. A-meta-analysis of RCTs conducted by Lee et al. [19] involving 454 patients, revealed that 231 patients had RF denervation and 223 patient controls, had sham or epidural blocks. The RF group had significantly lower back pain improvement than the control group after 1 year of follow up, and patients who showed an improvement to diagnostic block, had always significantly lower back pain improvement, compared to the control group. A metaanalysis conducted in 2014 by Leggett et al. [5] found that RF ablation of sacroiliac joint and facet joint was effective in five of the six studies evaluated, in decreasing the pain significantly at short term follow up (>1 year). Another meta-analysis was conducted in 2014 by Poetscher et al. [20] which included 9 studies, they concluded that RF neurotomy of the facet joint had a greater effect than intra-articular corticosteroid injection and showed that RF neurotomy has from moderate to low quality of evidence. The moderate or low-quality evidence might result from a rich periarticular innervation of the degenerated facet joints, and diffuse distribution of fine nerve endings, including sensory and autonomic fibres supplying the medial joint capsules. Modification of the RF technique may have a good response; however, more studies may be required to develop a more effective treatment for the facet related pain [6,11]. The degenerated facet joints trigger rich peri-articular innervations, associated with swelling of the synovial capsules of the facet joints as described. RF ablation of the facet joint capsule had been discussed, with possibility of improvement with using the bipolar RF techniques. The bipolar technique will potentially burn and coagulate more surface area compared to the monopolar technique, leading to more denervation of the facet joint capsule and therefore greater improvement [6,16]. It has been found that using the RF electrodes in parallel, and near each other using a bipolar technique may have the potential to cause a larger burn area, and coagulation between the electrodes. Furthermore, investigators had shown that the bipolar lesions increased in size and became spherical after increasing the length of the active tip of the electrodes [17,21,22]. Prior to this, no studies have been conducted to compare the efficacy of monopolar and bipolar technique for RF neurotomy of the medial branch of the dorsal nerve. This study was considered as a pilot study, aiming to improve the pain scores after the use of RF technique, depending on the idea of the increase of the area of coagulation, after using the bipolar technique [17,22]. Limitations faced during this study were the small sample size of the patients. The small area which was targeted for applying the electrodes for RF neurotomy, and the regular follow-up for patients at the pain clinic (accurate timings) were considered as difficulties. As with any interventional procedures, there may be potential complications related to RF neurotomy. Although it is usually rare, but can occur, and may include soreness around the treated area, numbness of skin overlying the treated area, worsened pain which may be attributed to muscle spasm in the area treated, permanent nerve pain and infection. The most common side effect of the procedure is the transient discomfort and soreness which are usually not severe [18-20]. Although we did not face any major side effects in the managed groups, we assessed the overall patient satisfaction as a reflection to this potential common side effects. This study shows low pain scores in both groups after 1 month of the procedure. Higher pain scores were observed in both groups after 6 months from RF ablation, with no considerable difference in pain scores between groups at all times, Patient satisfaction is higher in group 2 More studies with larger number of patients are required to give us more accurate results.
Conclusion
The use of bipolar technique for RF neurotomy of the medial branch of the dorsal nerve did not add more benefits to the patients in decreasing pain scores at different timings, compared to monopolar technique.
References
- Nedelka T, Nedelka J, Schlenker J, Hankins C, Mazanec R (2014) Mechanotransduction effect of shock waves in the treatment of lumbar facet joint pain: Comparative effectiveness evaluation of shock wave therapy, steroid injections and radiofrequency medial branch neurotomy. Neuro Endocrinol Lett 35: 393-397.
- Manchikanti L, Boswell MV, Singh V, Benyamin RM, Fellows B, et al. (2009) Comprehensive evidence-based guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician 12: 699-802.
- Sokolof JM, Nampiaparampil DE, Chimes GP (2012) Use of medial branch blocks before radiofrequency ablation for lumbar facet joints. PM R 4: 521-526.
- Veizi E, Hayek S (2014) Interventional therapies for chronic low back pain. Neuromodulation 17: 31-45.
- Leggett LE, Soril LJ, Lorenzetti DL, Noseworthy T, Steadman R, et al. (2014) Radiofrequency ablation for chronic low back pain: a systematic review of randomized controlled trials. Pain Res Manag 19: 146-153.
- Linqiu Zhou, Carson D, Schneck, Zhenhai Shao (2012) The anatomy of dorsal ramus nerves and its implication in lower back pain. Neuroscience & Medicine 3: 192-201.
- Likert Rensis (1932) A Technique for the Measurement of Attitudes. Archives of Psychology 140: 1-55.
- Varlotta G, Lefkowitz T, Schweitzer M, Errico T, Spivak J, et al. (2011) The lumbar facet joint: a review of current knowledge; part 1: anatomy, biomechanics, and grading. Skeletal Radiol 40: 13-23.
- Jaumand NV, Welch WC, Winkelstein BA (2011) Spinal facet joint biomechanics and mechanotransduction in normal, injury and degenerative conditions. J Biomech Eng 133: 071010.
- Shuang F, Hou S, Zhu J, Yan L, Ying Z, et al. (2015) Clinical anatomy and measurement of the medial branch of the spinal dorsal ramus. Medicine (Baltimore) 94: 2367.
- Bogduk N, Long DM (1979) The anatomy of the so-called articular nerves and their relationship to facet denervation in the treatment of low-back pain. Neurosurg 51: 172-177.
- Cohen SP, Raja SN (2007) Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet) joint pain. Anesthesiology 106: 591-614.
- Kennedy D, Mattie R, HamiltonA, Conrad B, Smuck M (2016) Detection of intravascular injection during lumbar medial branch blocks: A comparison of aspiration, live fluoroscopy, and digital subtraction technology. Pain Med 17: 1031-1036.
- Iannuccilli J, Prince E, Soares G (2013) Interventional spine procedures for management of chronic low back pain-a primer. Semin Intervent Radiol 30: 307-317.
- Binder DS, Nampiaparampil DE (2009) The provocative lumbar facet joint. Curr Rev Musculoskeletal Med 2: 15-24.
- Robert E J, Ovidiu P, Michelle G (2017) Bipolar Radiofrequency Facet Ablation of the Lumbar Facet Capsule: An Adjunct to Conventional Radiofrequency Ablation for Pain Management. Cureus 9: 1635.
- Cosman ER Jr, Cosman ER Sr (2005) Electric and thermal field effects in tissue around radiofrequency electrodes. Pain Med 6: 405-424.
- Van Zundert J, Vanelderen P, Kessels A, Van Kleef M (2012) Radiofrequency treatment of facet-related pain: evidence and controversies. Curr Pain Headache Rep 16: 19-25.
- Lee CH, Chung CK, Kim CH (2017) The efficacy of conventional radiofrequency denervation in patients with chronic low back pain originating from the facet joints: a meta-analysis of randomized controlled trials. Spine J 9: 291-298.
- Poetscher AW, Gentil AF, Lenza M, Ferretti M (2014) Radiofrequency denervation for facet joint low back pain: a systematic review. Spine 39: 842-849.
- Bruners P, Lipka J, Günther RW, Schmitz-Rode T, Mahnken AH (2008) Bipolar radiofrequency ablation: is the shape of the coagulation volume different in comparison to monopolar RF-ablation using variable active tip lengths? Minim Invasive Ther Allied Technol 17: 267-274
- Choi E, Shin K, Nam S, Cheong I (2008) A study about size and shape of bipolar radiofrequency lesions. Korean J Anesthesiol 54: 197-200.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...