Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Research Article(ISSN: 2643-6760) 
Periareolar Excision of Fibroadenoma Mamma: A Perfect Cosmetic Solution for Benign Breast Tumors in Young Females Volume 5 - Issue 1
Pankaj Srivastava1*, Shalini Srivastava2* and Ram Jeet Maurya3*
- 1Surgery, Om Surgical Center & Maternity Home, Varanasi, India
- 2Gynecology, Om Surgical Center & Maternity Home, Varanasi, India
- 3Anesthesiology, Om Surgical Center & Maternity Home, Varanasi, India
Received:May 04, 2020; Published: May 19, 2020
Corresponding author: Pankaj Srivastava, Laparoscopic, Thoracic, Thoracoscopic & VATS Surgeon, Om Surgical Center & Maternity Home, SA 17/3, P-4, Sri Krishna Nagar, Paharia, Ghazipur Road, Varanasi, UP, INDIA. PIN-221007
ORCID ID: https://orcid.org/0000-0002-7321-614X
DOI: 10.32474/SCSOAJ.2020.05.000203
Abstract
Fibroadenoma is a common benign breast tumor of young unmarried girls. Surgical excision is the treatment of choice. In literature, many surgical approaches have been suggested to deal with this condition and evaluated in terms of patient’s satisfaction, esthetic presentation and cosmetic outcome. We herein report a series of thirteen patients who have undergone surgical procedure for the fibroadenoma breast. We applied periareolar incision to excise the fibroadenoma and got satisfactory results in terms of speedy recovery, fine hidden scar mark, no intra/post-operative complication and high level of patient’s satisfaction without compromising the primary goal of the surgical procedure i.e. complete excision of the tumor. We strongly recommend that periareolar incision should be applied to excise benign breast tumors especially fibroadenomas with only caveat of large tumors, very thin breast tissues and peripherally situated tumors.
Keywords: Benign breast tumor; fibroadenoma; periareolar incision; cosmesis; cosmetic; esthetic; Periareolar approach; Areola; nipple-areola; breast lump; Areola; incision; breast; excision; surgical techniques; Multiple fibroadenoma; breast surgery
Abbrevations: FNAC: Fine Needle Aspiration Cytology; BIRADS: Breast Imaging Reporting and Data System; NPO : nil per os (Nothing by mouth); OT : Operation Theater; IV: intravenous; ET tube: Endotracheal Tube; BIRADS: Breast Imaging-Reporting and Data System
Introduction
The majority of benign breast tumors are because of fibrocystic
disease, which denotes small fluid-filled cysts and moderate
epithelial cell and fibrous tissue hyperplasia. It can occur in
women of any age, but the peak incidence is during the second
and third decades of life [1] and up to 25% of patients present
with multiple fibroadenomas [2]. The incidence of fibroadenoma
decreases with increasing age and very less in postmenopausal
females. Fibroadenoma arises from both stromal and epithelial
connective tissue cells which contain receptors for both estrogen
and progesterone. That is why they tend to proliferate during
pregnancy because of excessive production of estrogen.
As age increases, the risk of malignant changes in fibroadenoma
rises [3]. This warrants excision of all such breast tumors.
Fibroadenoma with hyperplasia and cellular atypia indicates a
higher risk for breast cancer development [4]. Since fibroadenoma
is the disease of young females where surgical excision is the
treatment of choice, the surgeon often faces dilemma in the mode
of surgical intervention because he has to make proper balance in
successful excision with preservation of function and acceptable
esthetic-cosmetic outcome. Multiple incision techniques are
mentioned in literature like periareolar, periareolar overlying,
circumareolar etc. we have chosen periareolar skin incision for the
access and removal of the fibroadenoma.
Surgical Technique
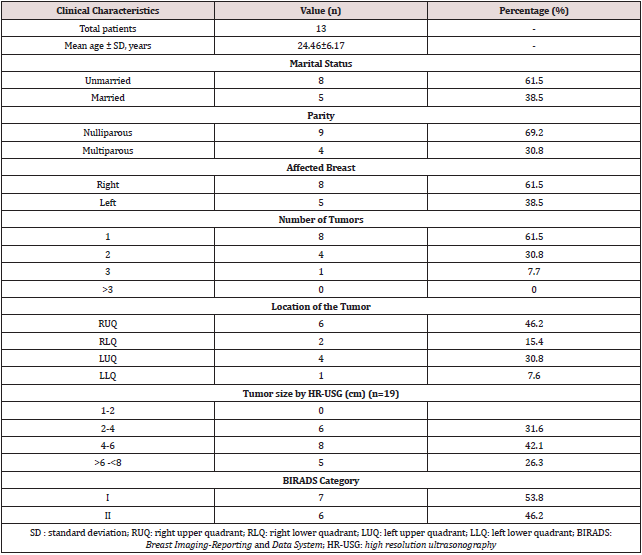
Total 13 patients were operated for fibroadenoma breast by periareolar incision method from 201 to 2019 in Om Surgical Center & Maternity Home. Informed consent was obtained from all the patients. Diagnosis of fibroadenoma was confirmed by FNAC. All patients were evaluated properly on various demographic parameters (Table 1). Sonomammography of the breast was performed and all patients revealed either BIRADS I or BIRADS II category. Hematology, biochemistry and serology tests were performed as per hospital surgical norms. PAC was done one day prior to the operation. Patient was put NPO 12 hours prior to the surgery. For surgical prophylaxis IV 1.5gm Cefoperazone- Sulbactum was given slowly 30-45 minutes preoperatively after skin sensitivity test. In OT, procedure was done under general anesthesia and patients were put in supine position. Pre-anesthetic medication was given as IV glycopyrrolate 0.2mg, midazolam 2.0mg, and butorphanol 1.0mg. After 3-4 minutes of preoxygenation, induction of general anesthesia with IV 100mg propofol and 100mg succinylcholine was given and patient was intubated with cuffed ET tube of 7.0mm inner diameter. GA was maintained with N20+O2 mixture and Vecuronium plus isoflurane combination.
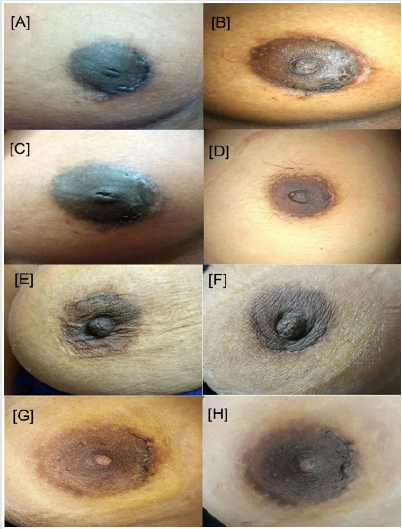
Patient was painted and drapped in supine position with wellexposed operated side breast. Breast mass was then palpated thoroughly and marked with skin pen (Figure 1). The periareolar incision of that side was then marked and size of the incision was assessed with that of mass so that during dissection and extraction of the tissue; margins of the incision line must be preserved and should not get ragged (Figure 2). Otherwise subcuticular suturing will not be as effectively approximate the wound margins as it should have. The periareolar incision should not be more than 50% of the perimeter of the areola. The subcutaneous tissue and fat planes were dissected by monopolar electrocautery by pulling the edges of the incision upward with skin hooks taking care that skin margins should not get cauterized. Dissection was continued in the deeper plane downward toward the mass. The position of the mass was determined again by palpation. After sidewise mobilization of the mass, the parenchyma over the mass was divided to expose and enucleate the lump (Figure 3). We usually apply bipolar electrocautery at this place to avoid unnecessary hemorrhage due to small feeding vessels. Hemostasis was meticulously maintained. The dead space was not obliterated, and drain was not required in any of the cases. The skin incision was closed with subcuticular running nonabsorbable prolene 3-0/4-0 suture on cutting needle (Figure 4) and sometimes with absorbable monocryl 4-0/5-0 suture where stitch removal is not required (Figure 5). Patient was then extubated after giving IV myopyrolate 5ml supported with oxygen by mask. Ball bandage was applied over the wound for compression immediately and retained for 5-7 days. Patient was shifted to the recovery ward after getting full consciousness. Breast support was given to each patient with appropriate size brassiere. The wound was inspected on the 8th postoperative day when the patients came for stitch removal (Figure 6). The patients were followed up on two weekly visits for a minimum of 3 months. Clinical photographs were taken on routine follow-up visits (Figure 7). Histopathologic examination revealed benign breast ducts with surrounding stromal proliferation; epithelial proliferation in pericanalicular and intracanalicular patterns; areas of duct adenosis; dilatation; areas of fibrosis and no stromal overgrowth, atypia or significant mitoses (Figure 8).
Figure 2: The periareolar incision just at the edge of the areola and skin (see the incision applied is short than the marking).

Figure 3: Entire fibroadenoma taken out of the periareolar incision after dissection (see the intact capsule).

Clinical Presentation
Total thirteen patients were taken for the study that underwent operation for the fibroadenoma of the breast using periareolar incision. The age of the patient ranged from 18 to 36 years with mean of around 25 years. Most of the patients were unmarried whereas five were married and having 1 to 3 children. Right breast was more often affected than the left in which upper quadrant of the breast was predominantly involved. We encountered single tumor in majority of cases; four cases had two and one had three tumors. In cases with multiple fibroadenomas, all were present in the same quadrant. Tumor was the presenting feature in all the cases. Pain was present in more than half of the cases. We did not find any other associated complain like nipple discharge etc. All the patients were having BIRADS I or II category lesions. None of the patient had any history of previous breast ailment or any surgery. Follow up time ranged from minimum of 3 months to even 10 years. Detailed clinical presentation have been summarized in Table 1.
Discussion
The traditional method of benign breast tumor resection used widely, is a radial or arc incision along the langer’s lines on the skin above the pathological changes of the breast, in order to minimize damage to the mammary ducts [5], whereas ugly postoperative scar significantly affects the appearance of the breast with this approach (Figure 9, red encircled]. If there are multiple lesions, there will be more scars left after removal of the tumors and the bilateral breasts will be asymmetrical. This can cause the patient much psychological pressure and affect their quality of life. Many incision techniques have been used to give better cosmetic outcome to the breast after operation. Fibroadenoma excision through periareolar incision or through an overlying incision [6,7]. Circumareolar Incision and dissection through subdermal tunnel has also been tried successfully for excision of multiple breast fibroadenoma [8]. Multiple fibroadenoma of the breast can safely be removed by the Ribeiro technique modified by Rezai [9].
Figure 9: Big and unsightly post-operative scar after radial incision approach for excision of fibroadenoma almost after 10 years of operation.

Dufourmentel in 1928 first time used this incision for operation
on breast [7]. Later on, the periareolar incision was widely used in
gynecomastia [10,11] and in breast augmentation [12,13] for a long
time because of having cosmetic benefit. Shrotria considered the
periareolar incision as the gateway to the breast [14].
Post-operative scarring in periareolar incision is almost
negligible close to no scar mark after 2-3 months period (Figure
7). In one study, authors have reported only 3 patients with scar
diathesis out of 153 operated patients [6]. Certain studies reported
that there are no difference in duration of surgery and the amount
of bleeding when comparing periareolar and traditional radial/arc
incisions [6]. In our patients we also found very good results in terms
of short operation time, very less or negligible bleeding, preserved
nipple-areola sensations, and most importantly cosmesis.
In literature, certain studies described several disadvantages
of periareolar incision (Table 2), such as longer operation time,
larger volume of intraoperative blood loss, prolonged exposure,
more damage to breast tissue specially in creating subcutaneous
tunnel, nipple ischemia, scar diathesis, disruption of lactation, and
hypertrophic scars & keloids in Caribbean women [6,7,15,16].
Fortunately we had had not experienced any of the above in our all
patients except negligible skin loss at wound margin in one patient
(Figure 7B).
The nipple-areola complex is always innervated by the lateral
and anterior cutaneous branches of the 3rd, 4th, and 5th intercostal
nerves. These cutaneous branches traverse superficially within
the subcutaneous fat and reached the nipple from the lateral side,
terminating at the medial border of the areola. Surgeons must keep
in mind that the nerves innervating the nipple and areola are best
protected if skin incisions at the lateral border of areola are avoided
[17]. It has been reported that a periareolar incision is not suitable
for the tumor of >5 cm in diameter or when the distance between
the tumor and the areola is >34cm, as there is chances of potential
damage to the lactiferous ducts [7]. However, Kong et al used
periareolar incision even when the distance between the tumor
and the areola was 7.5cm and ensured good patient outcomes [6].
Our series also supported that tumor at periphery of the breast may
also be successfully approached through the periareolar incision.
We did operate on tumors up to 7.0 cm with favorable results
without any complications.
In order to avoid damaging lactiferous ducts, one has to
make plane of dissection very carefully between thick layer of
subcutaneous fat and breast tissue. If breast is not bulky, dissection
should be directed directly to the tumor by deepening the plane of
dissection without disrupting surrounding soft breast tissue so as
to minimize tissue damage and successful excision of fibroadenoma.
Surgeon may use both blunt and sharp dissection to achieve the
target. In our practice we usually do maximum blunt dissection
by the finger and use bipolar electrocautery whenever deemed
necessary. The another disadvantage of the periareolar incision
is the flattening or collapse of the nipple-areola complex reason
being thin fatty layer, excessive dissection and resection of the
subcutaneous breast tissues underneath the nipple-areola complex,
large mass occupying almost whole breast and tumor located just
beneath the areola. To avoid this unwanted outcome, surgeon must
evaluate the case properly regarding the surgical approach and
once decided for the periareolar incision then do minimal sharp
dissection and ensuring minimal use of electrocautery under the
nipple-areola complex.
Despite all as most of the fibroadenomas occur in young
unmarried females in whom scar marks on their breast not only
impose blot to their beauty but also create psychological insult.
Therefore, cosmetically acceptable scar or camouflaged scar is
of paramount importance to them with removal of the disease
i.e. fibroadenoma. The periareolar incision scar motivates them
to accept the operative procedure readily and fulfill further their
desire.
Conclusion
The treatment plan of benign breast lesions including fibroadenoma should be chosen according to the location and size of the tumor because the primary aim should be the complete excision of the disease i.e. fibroadenoma with best possibility of keeping the cosmetic appearance of the breast intact. The cosmetic results of excision of fibroadenoma by a periareolar incision are very promising in young patients with palpable tumor. The added advantages of speedy recovery, small incision and hidden scar mark make the periareolar incision as main surgical technique for the excision of the fibroadenoma having caveat of multiple fibroadenomas, large tumor and tumors situated deep in peripheral breast tissue. However, periareolar incision warrants higher technical requirements from the surgeons because careful search of proper plane of dissection, meticulous hemostasis, adequate soft tissue handling and minimal disruption of normal surrounding breast tissue are the keys to successful outcome.
Acknowledgements
None
Conflict of Interest
No conflict of interest declared by the authors
References
- Arno Kuijper, Ellen CM, Mommers Elsken vander Wall, Paul J van Diest (2001) Histopathology of Fibroadenoma of the Breast. Am J Clin Pathol 115: 736-742.
- Lovasic F, Petkovic M, Belac Lovasic I, Mustac E, Uravic M, et al. (2011) The “round block” surgical technique in the management of multicentric fibroadenomas. Coll Antropol 35: 235-240.
- Egger H, Muller S (1977) Fibroadenoma of the breast. Dtsch Med Wochenschr 102(42): 1495-1500.
- El-Wakeel H, Umpleby HC (2003) Systematic review of fibroadenoma as a risk factor for breast cancer. Breast 12(5): 302-307.
- Weledji EP, Tambe J (2018) Breast Cancer detection and Screening. Med Clin Rev 4(2): 8.
- Xiangnan kong, Xi chen, Liyu jiang, Tingting ma, Baosan han, et al. (2016) Periareolar incision for the management of benign breast tumors. Oncology Letters 12: 3259-3263.
- Liu XF, Zhang JX, Zhou Q, Chen F, Shao ZM, et al. (2011) A clinical study on the resection of breast Fibroadenoma using two types of incision. Scandinavian Journal of Surgery 100: 147-152.
- Agodirin SO, Rahman GA, Olatoke SA, Akande HJ (2017) Circumareolar Incision-subdermal Tunneling Dissection for Excision of Multiple Breast Fibroadenomata. Niger J Surg 23(1): 63-66.
- Camara O, Egbe A, Koc I, Herrmann J, Gajda M, et al. (2009) Surgical Management of Multiple Bilateral Fibroadenoma of the Breast: The Ribeiro Technique Modified by Rezai. Anticancer Research 29: 2823-2826.
- Saad MN, Kay S (1984) The circumareolar incision: a useful incision for gynaecomastia. Ann R Coll Surg Engl 66(2):121-122.
- Pitanguy I (1966) Transareolar incision for gynecomastia. Plast Reconstr Surg 38(5): 414-419.
- Becker H (1999) The intra-areolar incision for breast augmentation. Ann Plast Surg 42(1): 103-106.
- Jones FR, Tauras AP (1973) A periareolar incision for augmentation mammaplasty. Plast Reconstr Surg 51(6): 641-644.
- Shrotria S (2001) The peri-areolar incision--gateway to the breast! Eur J Surg Oncol 27(6): 601-603.
- Eman E, Loay MG, Taha AB, Ahmed E (2018) “Infra-Mammary Incision versus Peri-Areolar Incision in Management of Large Benign Breast Lesions; a Novel Approach”. Chronicle of Medicine and Surgery 2(6): 281-290.
- Naraynsingh V, Maharaj D, Rampaul R (2002) “Swiss-roll operation for giantfibroadenomas”. The Breast Journal 8(1): 45-46.
- Schlenz I, Kuzbari R, Gruber H (2000) The sensitivity of the nipple-areola complex: an anatomic study. Plast Reconstr Surg 105(3): 905-909.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...