Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Research Article(ISSN: 2643-6760) 
Mipo - A Biological Method for Fixation of Complex Fractures of Tibia Volume 1 - Issue 1
Preeti Singh1, Fardeen Bhimani2 and Rohan Bhimani3*
- 1Department of Orthopaedics, Osmania General Hospital, Hyderabad, India
- 2Department of Orthopaedics, Bharati Hospital, Pune, India
- 3Department of Orthopaedics, Hinduja Healthcare Surgicals, Mumbai, India
Received: April 16, 2018; Published: April 26, 2018
Corresponding author: Rohan Bhimani, Department of Orthopaedics, Hinduja Healthcare Surgicals, 11th Road, Khar (West), Mumbai-400052, India
DOI: 10.32474/SCSOAJ.2018.01.000103
Abstract
Introduction: Management of proximal and distal tibial fractures is challenging because of the complexity of injury, limited muscle coverage and poor vacularity. Surgical management of tibial fractures includes multiple options: external fixation, IM nailing, ORIF and minimally invasive plate osteosynthesis (MIPO). Open reduction and internal fixation with a plate may end in wide dissection and tissue devascularization. Fixation of tibial fractures with MIPO allows protection of soft tissue and blood supply. This is a report of a series of prospectively studied closed proximal and distal tibial fractures treated with MIPO.
Materials and Methods: A total of 20 patients with closed proximal or distal tibial or fractures were enrolled in the study between 2016 and 2017 and completed follow-up. Demographic characteristics, mechanism of injury, time required for union, range of motion and complications were recorded. Eleven patients had proximal tibial fractures and nine had distal tibial fractures. Patients were followed up to 2 and 6 weeks and then at intervals of 4 to 6 weeks until 12 months.
MResults: Mean age of the patients was 39.5 years (range 18-65 years). Thirteen cases were the consequence of high-energy trauma and seven were the result of low-energy trauma. The clinical and radiological outcome were excellent in 13 patients, good in 6 patients and fair in 1 patient. The average time for fracture union was 16.4 weeks, ranging from 16 to 20 weeks. None of our patients developed any complications.
Conclusion: MIPO is a reliable method of management for tibial fractures; it provides a high union rate and good functional outcome with minimal soft tissue problems.
Keywords: Tibial fractures, MIPO, Soft tissue, Locking plate, Osteointegration, Functional outcome, Clinical outcome
Abbreviations: MIPO: Minimally Invasive Plate Osteosynthesis, LCP: Locking Compression Plate
Introduction
Proximal tibial fractures are serious injuries and pose a treatment challenge. They usually result from high energy injuries, damage is usually extensive and open fractures, compartment syndromes, and vessel injuries are frequently related [1-4]. On the other hand, distal tibial fractures are typically the result of combined compressive and shear forces, and may end in instability of the metaphysis, with or without articular depression, and injury to the soft tissue [5]. The aim of fracture treatment is to obtain early fracture union in the most acceptable anatomical position with early and maximum functional return of activity. Conservative management of closed comminuted fractures with cast are associated with complications like prolonged immobilization, deformity, shortening, angulations, joint stiffness etc. Precise reduction by open reduction and internal fixation with conventional plate, frequently lead to complications like non-union, delayed union, infection, implant failure and need for bone grafting [6]. In addition, it also results in significant soft tissue stripping [3,7] The Minimally Invasive Plate Osteosynthesis (MIPO) is a technique which enables indirect reduction and stable fixation with minimal biological footprint and preserving vascular supply at the fracture site [3,8]. The aim of this prospective study was to evaluate clinical results and complications of MIPO in complex tibial fractures.
Materials and Methods
Case 1
Between 2016 and 2017, 20 patients with acute, closed proximal and distal tibial fractures were selected. Among them 11 had proximal tibial fractures and 9 had distal tibial fractures. The exclusion criteria included open fractures, tibial shaft fractures in which intramedullary nailing was done, fractures with neurovascular injury, and pathological fractures. There were 15 males and 5 females who consented to be a part of this study. Fractures were analysed preoperatively using radiographs and CT scans if there was any articular involvement (Figure 1). We prospectively gathered their data. Demographic characteristics, mechanism of injury, time required for union, range of motion and complications were recorded The Locking compression plate which are anatomically pre-contoured were used. Preoperative calculations were done on radiographs to ascertain the size of the plate, accurate size of locking, cortical and cancellous screws after subtraction of the magnification factor. Patients were operated on as soon as they were medically fit. Surgeries were performed under Spinal Anaesthesia. Patients were positioned supine on a radiolucent table. The involved leg was draped and a pneumatic tourniquet applied.
Figure 1: X-Ray showing the fracture of tibia and fibula at junction of proximal two-third and distal one-third.

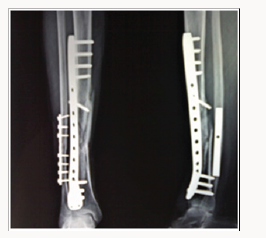
An incision of 2 to 3 cm over the proximal aspect of the tibia on the medial or lateral sides was made, according to the fracture site. For distal tibial fractures, a straight incision was made at the level of the medial malleolus or antero-laterally with preservation of the vessels and nerves depending on the fracture site. Fractures were reduced indirectly by a reduction forceps under fluoroscopic guidance and by ligamentotaxis using an external fixator. A sub muscular plane was made with a long hemostat and chisel without causing additional periosteal damage. The locking plate was applied sub muscularly to fix the fracture. The plate was fixed with screws, which were inserted percutaneously through the primary surgical incisions. Reduction and position of the plate was checked under a C-arm (Figure 2). Postoperatively, the limbs were protected using an above knee splint for 2 days. Active and passive range of motion exercises were permitted to avoid knee stiffness and to strengthen the quadriceps. Suture removal was done after 2 weeks and non-weight-bearing walking was allowed for 6 weeks. Partial weight bearing was allowed depending on fracture healing and patient compliance. At week 12, full weight bearing was permitted as tolerated. At each follow up patients was assessed for pain at the fracture site, tenderness, range of movement at knee and ankle, operative scar and radiological union at 6,10,14,18 and 22 weeks. Clinical and radiological assessments based on the criteria laid down by S.J.LAM9 were recorded using a proforma. The criteria are as follows:
a) Excellent: Range of movement of adjacent joints 80-100 % of normal. No pain in performing daily activities.
b) Good: Range of movement of adjacent joints 60-80% normal. Pain not enough to cause any modification of patient daily routine.
c) Fair: Range of movement of adjacent joints 30-60% normal. Pain enough to cause restriction patients daily activities.
d) Poor: Range of movement of adjacent joints less than 30% of normal. Pain enough to cause severe disability or non union.
Result
A total of 20 enrolled patients completed follow-up for one year and were included in the study; there were 15 males and 5 females. Mean age of the patients was 39.5 years (range 18-65 years). Thirteen cases were the consequence of high-energy trauma and seven were the result of low-energy trauma. Proximal tibial fracture was in eleven cases and distal tibial fractures in nine cases. Majority of the patients were operated within 3 days of injury. On S.J.LAM criteria, 13 patients showed excellent results, 6 patients had good results and 1 patient had fair result. The average time for fracture union was 16.4 weeks, ranging from 16 to 20 weeks (Figure 3). None of our patients developed any complications.
Discussion
MIPO allows indirect fracture reduction and percutaneous sub muscular implant placement [3]. The minimal-invasive method agrees in theory to combine the principles of a stable construct to a closed reduction with conservation of the haematoma [10]. Contrast to conventional plates, the locking compression plate (LCP) is anatomically pre-contoured; it does not depend on on friction and provides superior stability. Thus, it reduces the risk of loss of reduction through locking screws secured in the plate. The key aspect that led.com to use locking plates to treat fractures of the tibial shaft was the difficulty we would have faced in controlling the reduction of the proximal or distal fractures with intramedullary nailing. Indirect reduction and subcutaneously applied plates protects soft tissue and periosteal blood supply; hence, MIPO should provide undisturbed union and a low complication rate. In spite of the advantage of well-preserved blood supply, MIPO does not help in reduction. The fragments may not be anatomically reduced and interfragmentary compression may be inadequate, which consequences in delayed union. Barei DP et al. [11] demonstrated that after open reduction and internal fixation, 20% of the cases developed superficial or deep infections in spite of acceptable functional outcome. In this study, all patients had radiological union without any complications. In the present study, early surgical intervention was performed. Majority of patients were operated within 3 days because delay in intervention makes fracture reduction challenging. The time to consolidation reported in our study was to some extent less, when matched to the data known from the literature concerning plating osteosynthesis [4,5]. The average time for fracture union in our series was 16.4 weeks. MIPO decreases postoperative pain and aids early rehabilitation, which improves articular cartilage nutrition and healing. It is cosmetically more acceptable owing to less scar formation [3]. Uniqueness of this study was early mobilization, high mean time to fracture union, which was 16.4 weeks, no complications and majority of the patients having excellent outcome. The current study has some limitations. This is a non-randomized study with no control group. In addition, the sample size was small and the mean follow up was for 12 months. In conclusion, MIPO is a reliable method of treatment for distal tibial fractures; it provides a high union rate and good functional outcome with minimal soft tissue complications.
References
- Kim JW, Oh CW, Jung WJ (2012) Minimally Invasive Plate Osteosynthesis for Open Fractures of the Proximal Tibia. Clinics in Orthopedic Surgery 4(4): 313-320.
- Sament R, Mayanger JC, Tripathy SK (2012) Closed reduction and percutaneous screw fixation for tibial plateau fractures. Journal of Orthopaedic Surgery 20(1): 37-41.
- Raza H, Hashmi P, Abbas K (2012) Minimally invasive plate osteosynthesis for tibial plateau fractures. Journal of Orthopaedic Surgery 20(1): 42-47.
- Biggi F, Di Fabio S, D’Antimo C (2010) Tibial plateau fractures: Internal fixation with locking plates and the MIPO technique. Injury Int J Care Injured 41(11): 1178-1182.
- Dinko Vidovic D, Matejcic A, Ivica M (2015) Minimally-invasive plate osteosynthesis in distal tibial fractures: Results and complications. Injury Int J Care Injured 46(6): 96-99.
- Wang TJ, Ju WN and Qi BC (2017) Novel management of distal tibial and fibular fractures with Acumed fibular nail and minimally invasive plating osteosynthesis technique A case report. Medicine 96(12): e6482
- Ozkaya U and Parmaksizoglu AS (2015) Dual locked plating of unstable bicondylar tibial plateau fractures. Injury Int J Care Injured 46(2): S9- S13.
- Kim HJ, Park KC, Kim JW (2017) Successful outcome with minimally invasive plate osteosynthesis for periprosthetic tibial fracture after total knee arthroplasty. Orthopaedics and Traumatology: Surgery & Research 103(2): 263-268.
- Lam SJ (1964) The place of delayed internal fixation in the treatment of fractures of the long bones. J Bone Joint Surg 46(3): 393-397.
- Adam P, Bonnomet F and Ehlinger M (2012) Advantage and limitations of a minimally-invasive approach and early weight bearing in the treatment of tibial shaft fractures with locking plates. Orthopaedics and Traumatology: Surgery & Research 98(5): 564-569.
- Barei DP, Nork SE, Mills WJ (2004) Complications associated with internal fixation of high-energy bicondylar tibial plateau fractures utilizing a two-incision technique. J Orthop Trauma 18(10): 649-657.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...