
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6679
Short Communication(ISSN: 2637-6679) 
Transit Sound Levels from the Delivery Room to the Neonatal Unit Volume 7 - Issue 4
Raja Nandyal1, Michele Coleman2 and Susan Bedwell DNP3
- 1Professor of Pediatrics, Neonatology Section, Oklahoma University Health Sciences Center, US
- 2Department of Primary Care pediatrics, Edmond, Oklahoma University Health Sciences Center, US
- 3Director of Quality Improvement, OU Section of Neonatal-Perinatal Medicine, Oklahoma University Health Sciences Center, US
Received: March 12, 2022; Published: March 25, 2022
Corresponding author: Raja Nandyal, MD, Professor of Pediatrics, Neonatology Section, Oklahoma University Health Sciences Center, US
DOI: 10.32474/RRHOAJ.2022.07.000267
Abstract
In 1997, the American Academy of Pediatrics (AAP) recommended that the sound levels be limited to less than 45 dB in a Neonatal Intensive Care Unit (NICU). Follow-up studies of growing premature infants show high incidence of neurodevelopmental problems, including hearing loss. This is an observational study to assess the sound levels that a neonate can be potentially exposed to during the transport in a closed incubator from the delivery room to NICU. Sound levels were measured using a dosimeter. A continuous recording of sound decibels was made with the time stamped, at nine predetermined specific points during the transit. In addition to preparatory runs, sound levels for ten separate consecutive runs were measured to account for the variations in the extraneous environmental noise. All ten runs had decibels above 45 decibels. The lowest average dB level recorded during the run was 56.2 and the highest average was at 88.7. The highest levels occurred when the incubator was moved into and out of the elevator (81.5 dB and 83.5 dB respectively). Our study suggests that a neonate has the potential to experience higher than recommended sound levels during the transit from the delivery room to the Neonatal ICU. Newly acquired data can help to further modify the transport incubator, by adopting various technological advances noted in other industries, and in different environments.
Introduction
In 1997, the American Academy of Pediatrics (AAP) [1] recommended that the sound levels be limited to less than 45 dB in a Neonatal Intensive Care Unit (NICU) on A-weighted scale (dBA). Several preventive and therapeutic modalities that evolved during the last few decades have resulted in a dramatic improvement, in the survival rate of premature infants [2,3]. Follow-up studies of these growing premature infants show high incidence of neurodevelopmental problems, including hearing loss [4,5]. Noise in the NICU has the potential to contribute to hearing impairments, sleep disturbance, somatic effects, and developmental problems in preterm infants. NICU environment, including unprotected exposure to excessive sound is considered as a potential cause for the hearing loss5. The adverse effects of exposure to sound levels during the neonatal transport from a referring hospital to a perinatal center by ground or by air were previously studied [6,7]. We are not aware of any study that assessed the sound levels that a neonate can be potentially exposed to during the transit in a transport incubator, from the delivery room to NICU. This is an observational study, to assess the sound levels that a neonate can be potentially exposed to during the transport in a closed incubator from the delivery room to NICU.
Methods
Sound levels in an actual transport incubator (Airborne 185A+, Life Support Systems) which is always used for the transport of highrisk neonates from the delivery room to the NICU at our perinatal center, were measured. We used a dosimeter (Reed C-322 Sound Level Meter and Data Logger, 30 to 130 dB range, 0.1 dB graduation, +/- 1.5 dB Accuracy). It was placed within the incubator with the doors closed during the transit, from the delivery room on the 4th floor to a semiprivate room in a Level IV Neonatal ICU, located on 7th floor. No neonate was placed in the incubator. During the incubator runs, the study team tried to imitate the usual pace that is used when a neonate is being transported from the delivery room to NICU. A continuous recording of sound decibels was made with the time stamped, at nine predetermined specific points during the transit. Those were the start, initial closing of the transport incubator door, bump in the hallway, door to the elevators, moving equipment on top of incubator, entering the elevator, exiting the elevator, NICU entrance door, and the stop at the NICU. In addition to preparatory runs, sound levels for ten separate consecutive runs were measured to account for the variations in the extraneous environmental noise. The study was done on a Sunday, because of the team’s availability and the team did not want to interfere with the busy schedule of the weekdays.
Results
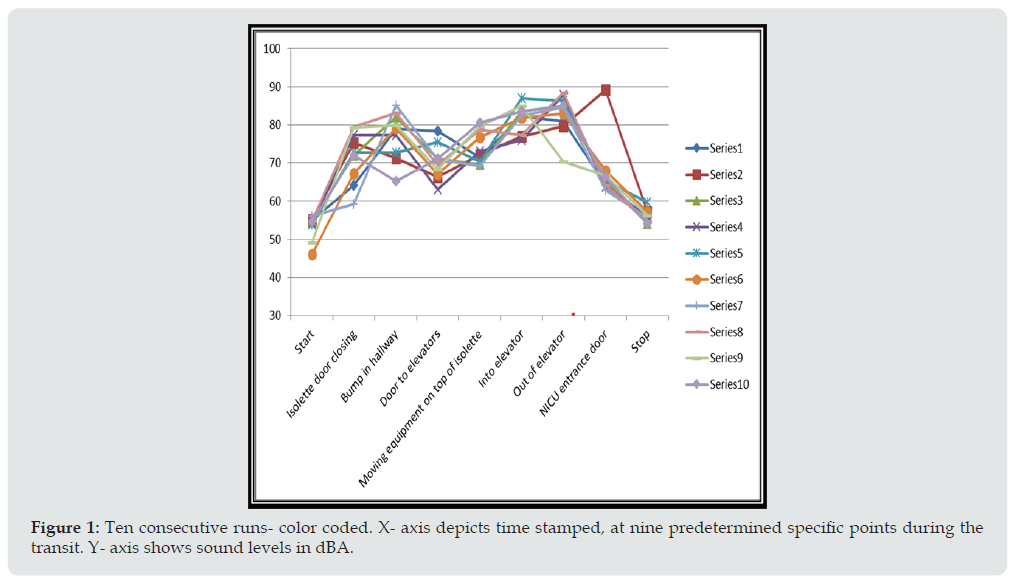
As reflected in the graph (Figure 1), all ten runs had decibels above 45 decibels. Transport time from the delivery room to NICU averaged 2.5 minutes. The lowest average dB level recorded during the run was 56.2 and the highest average was at 88.7. The highest levels occurred when the incubator was moved into and out of the elevator (81.5 dB and 83.5 dB respectively).
Figure 1: Ten consecutive runs- color coded. X- axis depicts time stamped, at nine predetermined specific points during the transit. Y- axis shows sound levels in dBA.
Discussion
National Center for Environmental Health [8] established a fact, that exposure to loud sound has the potential to cause hearing loss. And there is ample evidence to say that when a preterm infant, a compromised neonate, or even a normal term newborn, when exposed to excessive sound levels, it may result in adverse outcome [5,9,10]. Often, intensive care environments, especially of NICUs, are filled with extraneous noise coming from medical staff rounds, presentations, and other healthcare professional discussions. Other sources include sound generated by NICU equipment, monitor alarms, ventilators, beepers, cell phones, and even closure of the doors, to which preterm infants are potentially vulnerable [5,11,12]. The crying of an infant can be a significant source of noise, as loud sounds tend to be amplified within the incubator [11,12]. Darcy et al. [13] found that the ‘hourly mean sound levels in each NICU ranged from 53.9 dB to 60.6 dB, with no statistically significant difference between noise levels recorded on day shift versus night shift, and no statistically significant difference among sites. Their data contradicted nurses’ perception that the day shift generates more noise due to various day time activities, than that of the night shift. Our study showed that the highest sound levels occurred when the incubator was moved into and out of the elevator (81.5 dB and 83.5 dB respectively). Those levels were very close to 85 dBA. Sound levels of 80 to 89 dB were noted in heavy traffic, window air conditioner, noisy restaurant, and with power lawn mower. And it was reported that sound levels above 85 dB are harmful [14]. Recent comparative study [15] of 3 modes of neonatal incubators, concluded that ‘a preterm infant in an incubator is exposed to noise levels clearly exceeding international recommendations. This assessment included observation in all 3 neonatal incubators. Committee to Establish Recommended Standards for Newborn ICU Design [16], published their guidelines in 2013, which helped several hospitals in the design of modern NICUs. Still, several published studies showed that frequently, neonates are exposed to higher sound levels than those recommended by the AAP1. One such study done by Aita [17], showed that in the former open ward NICU, mean sound levels ranged from 54 to 61 dBA, and were consistently (100%) above the recommended hourly level of 45 dBA, whereas mean levels in their newer NICU ranged from 47 to 51 dBA and exceeded 45 dBA no more than 75% of the time. Recently, Restin et al. [18] commented that the fan inside the incubator, generates noise in the frequency range of 1.3–1.5 kHz with a weighted sound pressure level (SPL) of 40.5 dB(A). Even though the incubator narrows the transmitted frequency spectrum of sound entering the incubator to lower frequencies, it does not significantly reduce the transient noises, such as alarms or the opening and closing of cabinet doors.
Conclusion
Our study suggests that a neonate has the potential to experience higher than recommended sound levels during the transit from the delivery room to the Neonatal ICU. Obviously, there was no neonatal experience in this study, as it was primarily conducted as a pilot study. The information we collected can be used to test the existing sound barriers with larger ‘n’ and duplicate the study without human participation. Newly acquired data can help to further modify the transport incubator, by adopting various successful technological advances noted in other industries, and in different environments. The results can be analysed and then select the best modification which is optimal for the neonatal transport. In addition to decreasing noise level, the researcher needs to consider other aspects of the transport, the accessibility to the neonate during the transport for procedures (positive pressure ventilation, administration of medication), electronic monitoring, visibility, temperature control, easy transferability etc. Ideally, neuro developmental follow up studies will add to the value of such studies.
References
- American Academy of Pediatrics, Committee on Environmental Health (1997) Noise: a hazard for the fetus and newborn. Pediatrics 100: 724-727.
- Kaempf J, Morris M, Steffen E, Wang L and Dunn M (2021) Continued improvement in morbidity reduction in extremely premature infants. Arch Dis Child Fetal Neonatal Ed 106: 265-270.
- Sood, BG and Brodsky DD (2019) Current Advances in Neonatal Care. Current Advances in Neonatal Care. Pediatric Clinics 66(2): 17-18.
- Taylor GL, Joseph RM, Kuban KCK, Douglass LM and Laux, J, et al. (2021) Changes in Neurodevelopmental Outcomes from Age 2 to 10 Years for Children Born Extremely Preterm. Pediatrics 147(5):
- Wachman, EL and Lahav A (2011) The effects of noise on preterm infants in the NICU. Arch Dis Child Fetal Neonatal Ed 96: F305-F309.
- Vickie Bailey V, Szyld E, Cagle K, Kurtz D and Chaaban H (2019) Modern Neonatal Transport: Sound and Vibration Levels and Their Impact on Physiological Stability - Am J Perinatol 36(04): 352-359.
- Bouchut JC, Lancker EV, Chritin, Gueugniaud PY (2011) Physical Stressors during Neonatal Transport: Helicopter Compared with Ground Ambulance. Air Medical Journal. 30(3): 134-139.
- Eichwald, J and Yulia Carroll Y (2018) Loud Noise: Too Loud, Too Long! J Environ Health 80(8): 34-35.
- Bremmer P, Byers JF, Kiehl, E (2003) Noise and the premature infant: physiological effects and practice implications. J Obstet Gynecol Neonatal Nurs 32(4): 447-454.
- Philbin MK (2000) The full-term and premature newborn: the influence of auditory experience on the behavior of preterm newborns. J Perinatol 20: 77−87.
- Bellieni C, Buonocore G, Pinto I, Stacchini N and Cordelli DM (2003) Use of sound-absorbing panel to reduce noisy incubator reverberating effects. Biol Neonate 84(4): 293-296.
- Altuncu E, Akman I and Kulekci S (2009) Noise levels in neonatal intensive care unit and use of sound absorbing panel in the isolette. Int J Pediatr Otorhinolaryngol 73: 951-953.
- Darcy AE, Hancock LE and Ware EJ (2008) A descriptive study of noise in the neonatal intensive care unit: ambient levels and perceptions of Adv Neonatal Care. 8(3): 165-175.
- Michigan Medicine (2020) Harmful Noise Levels.
- Zacaríasa, FF, Jiméneza JLB, PJ Bustillo Velázquez Gaztelua, PJB, Molinaa, RH and López, SL (2018) Noise level in neonatal incubators: A comparative study of three models. Otorhinolaryngology 107: 150-154.
- White RD, Smith JA and Shepley MM (2013) Recommended standards for newborn ICU design, eighth edition. J Perinatol 33: S2-16.
- Aita M, Robins S, Charbonneau L, Pascal Doray Demers P and Feeley N (2021) Comparing light and noise levels before and after a NICU change of design. J Perinatology 41: 2235-2243.
- Restin T, Gaspar M, Bassler D, Kurtcuoglu V, Scholkmann Fand Haslbeck FB (2021) Newborn Incubators Do Not Protect from High Noise Levels in the Neonatal Intensive Care Unit and Are Relevant Noise Sources by Themselves. Children 8(8): 704.

.png)


