
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6679
Case Report(ISSN: 2637-6679) 
Sildenafil, Tramadol, and Hashish; the Single or Triple Triggering Cause of Acute Myocardial Infarction with Possible Coronary Spasm; Complex Dilemma and Dramatic Response Volume 6 - Issue 2
Yasser Mohammed Hassanain Elsayed*
- Critical Care Unit, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt
Received: April 28, 2021 Published: May 11, 2021
Corresponding author: Yasser Mohammed Hassanain Elsayed, Critical Care Unit, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt
DOI: 10.32474/RRHOAJ.2021.06.000236
Abstract
Rationale: Acute myocardial infarction is unusual in young persons. Drug adverse effects may be very critical and deadly. Sildenafil is an approved first oral phosphodiesterase type-5 inhibitor pill by the Food and Drug Administration in the treatment the erectile dysfunction. Angina, coronary vasospasm, myocardial infarctions are recorded serious cardiac presentations with sildenafil. Acute myocardial infarction had happened post-oral tramadol in a heavy smoker. Smoking cannabis is known to be a rare acutely trigger myocardial infarction Coronary artery spasm implicated in the pathogenesis of infarction.
Patient concerns: A 45-year-old, male patient presented to the emergency department with acute ST-segment elevation myocardial infarction post-ingested combination of oral sildenafil tablet, oral tramadol tablet, and smoking of two hashish cigarettes at a party.
Diagnosis: Acute ST-segment elevation myocardial infarction post-ingested combination of oral sildenafil tablet, oral tramadol tablet, and smoking of two hashish cigarettes
Interventions: Electrocardiography, streptokinase infusion, cardiac enzymes, and later echocardiography.
Outcomes: clinical and electrocardiographic dramatic response to streptokinase infusion.
Lessons: Understanding pharmacokinetics, pharmacodynamics, drug interactions, and toxicology is essential for the clinician in any specialty. Coronary artery spasm has often implicated suggested mechanisms in inducing acute myocardial infarction. The three substance combinations induced myocardial infarction by either potentiating or synergism. A dramatic response for thrombolytic therapy despite the presence of both right ventricular with inferior ST-segment elevation myocardial infarction carries a good prognosis.
KeywordsSildenafil; Tramadol; Hashish; Acute Myocardial Infarction; Coronary Artery Spasm; Ischemic Heart Disease
Abbreviations:CAS: Coronary Artery Spasm; cGMP: cyclic Guanosine Monophosphate; ECG: Electrocardiogram; ICU: Intensive Care Unit; IHD: Ischemic Heart Disease; MI: Myocardial Infarctions; NO: Nitric Oxide; O2: Oxygen; PDE-5 inhibitor: Phosphodiesterase Type-5 Inhibitor; RV MI: Right Ventricular Myocardial Infarction; SMC: Smooth Muscle Cell; STEMI: St-Elevation Myocardial Infarction; THC: Tetrahydrocannabinol.
Introduction
Sildenafil citrate is one of the most frequently abused prescribed pharmaceuticals at hand nowadays[1,2] especially, among teenage males[3]. The pharmacological mechanism that encouraging the erection of the penis encompasses the emission of nitric oxide (NO) in the corpus cavernosum during sexual excitation. NO then catalyze guanylate cyclase enzyme, which results in increased levels of cyclic guanosine monophosphate (cGMP), producing smooth muscle cell (SMC) relaxation in the corpus cavernosum and allowing blood flow. Sildenafil is a strong and selective inhibitor of cGMP-specific PDE-5 in the corpus cavernosum, where PDE-5 is responsible for the degradation of cGMP[4]. The sildenafil total body clearance is 41 L/h with a consequent terminal phase half-life of 3-5 h. After either oral or IV administration, sildenafil is excreted as metabolites mainly in the feces (about 80 % of given oral dose) and to a marginal extent in the urine (about 13 % of given oral dose)[4]. Commonly, the recommended sildenafil dose for sexual intercourse is 50 mg with a maximum recommended dose of 100 mg or decreased to 25mg [5]. The single famous absolute contraindication for sildenafil is the simultaneous use of nitrates[6]. Sildenafil is better avoided in active ischemic heart disease (IHD), cardiogenic shock, and hypertensive patients on multiple antihypertensive regimens[2]. The most frequent sildenafil side effects are a headache, flushing of the face, and gastric upset5. Less frequent side effects are color visual changes [5]. Myocardial infarction (MI), stroke, arrhythmias, and death are rarely reported in men taking sildenafil [5]. Tramadol is an opioid analgesic and synthetic analog of codeine. Tramadol is a mu-opioid receptor agonist acting at the central level. The analgesic effect and affinity of mu-opioid receptors for tramadol are 10-fold less than codeine[7]. Tramadol is a synthetic analgesic for both moderate and severe pain in primary situations[8]. The initial dose is 25 mg and the maximum dose of 100 mg a day; the adult dose should not exceed 400 mg a day[8]. The other possible tramadol side effects include severe dizziness, swelling of the face and extremities, hallucinations, suicide attempt, somnolence, gastric upset, vomiting, diarrhea, sweating, itching, agitation, xerostomia, tremor, anorexia, and insomnia[8]. Gormel and his colleges (2015) reported one case of tramadol induced Kounis syndrome with subsequent acute lateral MI [9]. It is hypothesized that vasospastic angina could be induced-MI[9]. Cannabis is the most commonly used Worldwide abuse substance[10]. Its use is largely concentrated among young people (15- to 34-year-olds)[10]. It is derived from the plant Cannabis sativa[11]. Herb (marijuana), resin (hashish), and oil (hash oil) are the three principal kinds of cannabis products [12]. The most potent form of cannabis is cannabis oil, derived from the concentrated resin extract[12]. It may contain more than 60 percent of THC content[12]. Different classes of chemicals, including nitrogenous compounds, amino acids, hydrocarbons, sugar, terpenes, and simple fatty acids, together contribute to the unique pharmacological and toxicological properties of cannabis10. Delta-9-tetrahydrocannabinol (Δ-9-THC) and Cannabidiol (CBD), the two essential products of the cannabis Sativa plant, have distinct symptomatic effects[10]. According to the United Nations Office on Drugs and Crime (UNODC), the amount of THC present in a cannabis sample is commonly used as a measure of cannabis potency[12]. Smoking cannabis is known to be a rare acutely trigger MI[12,13]. Cannabis is dose-dependent in inducing MI[10]. One large study of 1,913 adults conducted in the USA found a significant association between MI and cannabis use regarding a dose-response effect[13]. Postulated theories for this include complex interactions between increased oxygen demand (due to increased heart rate and blood pressure), decreased oxygen (O2) supply (due to an increase in carboxyhemoglobin), and coronary vasospasm11. A coronary artery spasm (CAS) is a transient constriction of the muscular wall of one of the arteries resulting in diminution or entirely blockage of blood flow[14]. The precise mechanisms of CAS are still obscure but mostly multifactorial15. Most patients who presented with CAS don’t have common risk factors for heart disease. Tobacco usage, exposure to extreme cold, emotional stress, and substance abuse are famous triggers[14]. Psychological factors play an important role in IHD, but their role in CAS is not clear[15]. Past anxiety and depression are more prevalent in patients with CAS versus those with IHD. The link between emotional stressors with mental health factors with CAS, sympathetic nervous system (SNS) stimulation, inflammatory conditions, oxidative stress, endothelial dysfunction (ED), and SMC[15]. Either ST-segment depression or ST-segment elevation on ECG is a possible association with CAS [16]. Coronary angiography is essential for the diagnosis of CAS[17]. Nitrates, calcium channel blockers, and statins are commonly used drugs in CAS[14].
Case Presentations
A 45-year-old married Egyptian male worker patient presented to the emergency department with acute severe agonizing chest pain. Chest pain was ischemic. The patient gave a recent history of taken oral sildenafil tablet (25 mg), oral tramadol tablet (25 mg), and two hashish cigarettesin a party since about 2 hours of the initial ECG tracing. The patient denied any history of cardiovascular disease or other relevant diseases. Upon examination, the patient appeared distressed, sweaty, and anxious. His vital signs were as follows: blood pressure of 140/80 mmHg, pulse rate of 96/minute; regular, temp. of 36.2°C, respiratory rate of 16/min, and initial pulse oximetry of 98 %. No relevant local cardio-respiratory signs. Initial ECG tracing on presentation mild ST-segment elevations with small q-waves in inferior leads (II, III, and aVF) and reciprocal STsegment depressions in aVL and V2 leads of VR; 90 bpm (Figure 1). The patient was admitted to ICU as an acute myocardial infarction. He was initially managed with O2 inhalation using nasal cannula at the rate of 5 L/min. Pethidine HCL (100 mg) was given for chest pain in intermittent doses as needed. Serial ECG tracings were taken. ECG Tracing was done on ICU admission; within 13 hours of the above ECG tracing and just before given streptokinase showing ST-segment elevations with pathological Q-waves in inferior leads (II, III, and aVF), new ST-segment elevations in V1 and V3, and reciprocal ST-segment depressions in I, aVL, and V2 leads of VR; 96 bpm (Figure 2A). ECG Tracing is a right side ECG tracing was done on ICU admission; within 13.30 hours of the initial ECG tracing and just before given streptokinase showing ST-segment elevations with pathological Q-waves in both right ventricular (RV) leads (V3R and V4R) of VR; 95 bpm (Figure 2B). Aspirin; 4 oral tablets (75 mg), clopidogrel; 4 oral tablets (75 mg), streptokinase IVI (1.5 million units over 60 minutes), bisoprolol; oral tablet (5 mg), and captopril; half oral tablet (25 mg; was added after 48 hours of presentation) were given. ECG Tracing was done within 7.30 hours of ICU admission showing resolution of above ST-segment elevations and reciprocal ST-segment depressions of VR; 89 bpm. There are pathological Q-waves in inferior leads (II, III, and aVF), new T-wave inversions in III and aVF leads (Figure 2C). ECG Tracing is a right side ECG tracing was done within 24 hours of the initial ECG tracing showing resolution of above ST-segment elevations but there are pathological Q-waves (green arrows) in both right ventricular (RV) leads (V3R and V4R) of VR; 86 bpm (Figure 2D). The patient became completely symptomatically free after streptokinase infusion. ECG Tracing was done within 24 hours of the initial ECG tracing; within 13 hours of given streptokinase showing resolution of above STsegment elevations and reciprocal ST-segment depressions of VR; 92 bpm. There are still pathological Q-waves in inferior leads (II, III, and aVF) and T-wave inversions in III and aVF leads (Figure 2E). The initial emergency troponin I test was positive (76 ng/l). RBS was 214 mg/dl on admission. Later echocardiography showed inferior hypokinesia with EF 63 %. No other workup abnormality. The patient was continued on captopril tablet (25 mg twice daily), aspirin tablet (75 mg, once daily), clopidogrel tablet (75 mg, once daily), nitroglycerin retard capsule (2.5 mg twice daily started within 48 of presentation), and atorvastatin (40 mg once daily) until discharged on the 5th day.
Figure 1: ECG tracing was done on initial presentation of chest pain showing mild ST-segment elevations (red arrows) with small q-waves (blue arrows) in inferior leads (II, III, and aVF) and reciprocal ST-segment depressions in aVL and V2 leads (lime arrows) of VR; 90 bpm.
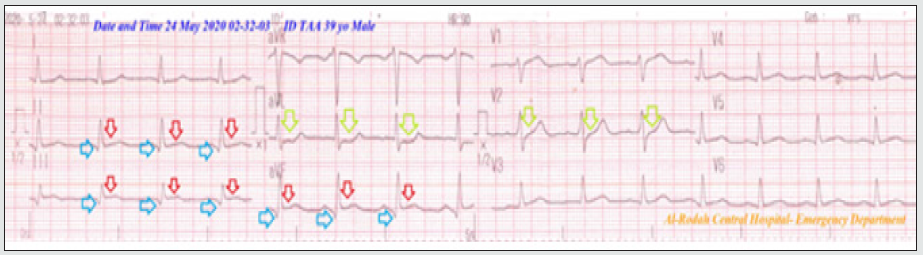
Figure 2A: Serial ECG tracings in ICU. Tracing was done on ICU admission; within 13 hours of the above ECG tracing and just before given streptokinase showing ST-segment elevations (red arrows) with pathological Q-waves (blue arrows) in inferior leads (II, III,and aVF), new ST-segment elevations in V1 and V3 (purple arrows), and reciprocal ST-segment depressions in I, aVL and V2 leads (lime arrows) of VR; 96 bpm.

Figure 2B: Tracing is a right side ECG tracing was done on ICU admission; within 13.30 hours of the initial ECG tracing and just before given streptokinase showing ST-segment elevations (orange arrows) with pathological Q-waves (green arrows) in both right ventricular (RV) leads (V3R and V4R) of VR; 95 bpm.
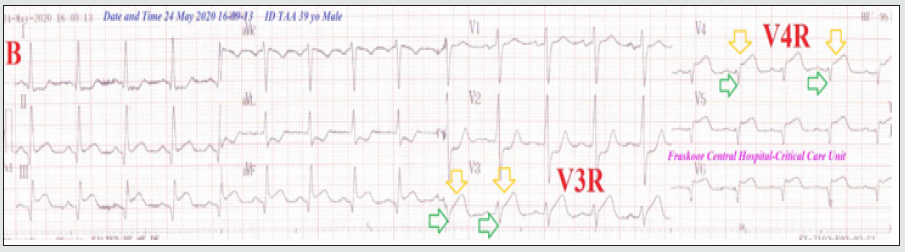
Figure 2C: Tracing was done within 7.30 hours of ICU admission showing resolution of above ST-segment elevations and reciprocal ST-segment depressions of VR; 89 bpm. There are pathological Q-waves (blue arrows) in inferior leads (II, III,and aVF), new T-wave inversions in III and aVF leads (green arrows).
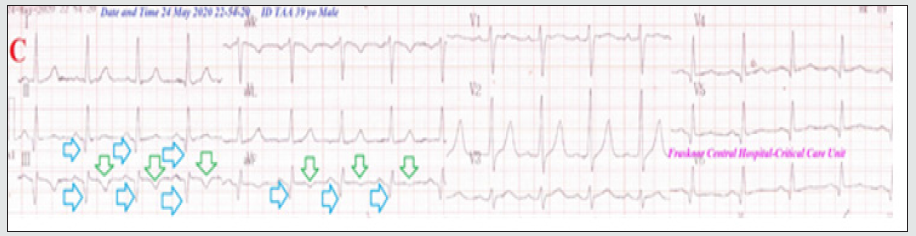
Figure 2D: Tracing a right side ECG tracing was done within 24 hours of the initial ECG tracing showing resolution of above ST-segment elevations but there are pathological Q-waves (green arrows) in both right ventricular (RV) leads (V3R and V4R) of VR; 86 bpm.
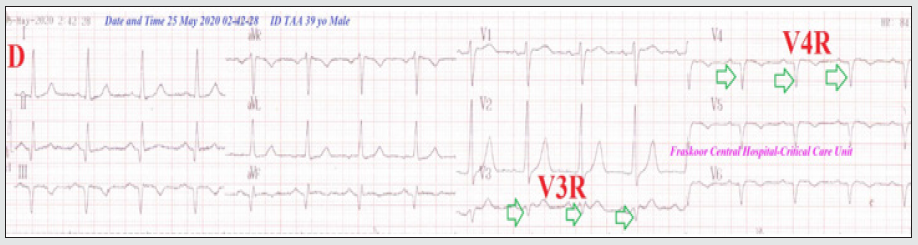
Figure 2E: Tracing was done within 24 hours of the initial ECG tracing; within 13 hours of given streptokinase showing resolution of above ST-segment elevations and reciprocal ST-segment depressions of VR; 92 bpm. There are still pathological Q-waves (blue arrows) in inferior leads (II, III, and aVF) and T-wave inversions in III and aVF leads (green arrows).

Discussion
Overview: A 45-year-old, male patient presented to the emergency department with acute inferior and right ventricular (RV) ST-segment elevation myocardial infarction (STEMI) postingested combination of oral sildenafil tablet, oral tramadol tablet, and smoking of two hashish cigarettes at a party.?
The primary objective: for my case study was clearing the existence of acute inferior and right ventricular STEMI postoral sildenafil tablet, oral tramadol tablet, and smoking hashish cigarettes in a young patient.
Study question here: Can the combination of sildenafil, tramadol, and hashish-induced myocardial infarction? and How the clinician will manage this case?.
The secondary objective: for the case study how to manage acute inferior and right ventricular STEMI post-oral sildenafil tablet, oral tramadol tablet, and smoking hashish cigarettes in a young patient?
The presence of acute RVMI with inferior STEMI carries more risk for complications and the need for fluids.
Despite the taken doses of both sildenafil and tramadol were within the recommended but all of the sildenafil, tramadol, and hashish have probability to cause acute myocardial infarction.
Potentiating or synergism for the three substances is a possible interpretation.
The author thinks that coronary artery spasm is implicated in the pathogenesis.
ST-segment elevation in V1 and V3 leads in the initial ECG on the ICU admission (Figure 2A) and resolute with treatment with no pathological Q-waves indicate the presence of associated coronary artery spasm.
The absence of shock and bradycardia despite the co-existence of RVMI with inferior STEMI may interpret by antagonizing actions for all three substances.
Adding vasodilators like nitrates and captopril were avoided in the first 48 hours to avoid possible happening severe hypotension, shock, and death that can be happening with sildenafil and RVMI with inferior STEMI.
There are absent bradycardia, absence heart block, and absent hypotension.
There is a good response for thrombolytic therapy.
The only limitation of the current study was the unavailability of coronary angiography.
I can’t compare the current case with similar conditions. There are no similar or known cases with the same management for near comparison.
Conclusion
Understanding pharmacokinetics, pharmacodynamics, drug interactions, and toxicology is essential for the clinician in any specialty. Coronary artery spasm has often implicated suggested mechanisms in inducing acute myocardial infarction. The three substance combinations induced myocardial infarction by either potentiating or synergism. A dramatic response for thrombolytic therapy despite the presence of both right ventricular with inferior ST-segment elevation myocardial infarction carries a good prognosis.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment:
I wish to thank the nurses team of the critical care unit who make extra-ECG copies for helping me.
References
- (2004) Fizer Inc. Viagra Web site. New York, NY.
- Alpert JS (2005) Viagra: The risks of recreational use. Am J Med118(6): 569-570.
- Albaugh JA and Kellogg Spadt S (2003) Man’s search for ultimate sex: Viagra abuse. Urol Nurs 23(1): 75-76.
- (2016) Sandoz Limited. Sildenafil Sandoz 100mg Tablets.
- (2010) FDA. VIAGRA® (sildenafil citrate) Tablets. Pfizer Icr 210:1-30.
- Shinlapawittayatorn, K Chattipakorn S, and Chattipakorn N (2005) Effect of sildenafil citrate on the cardiovascular system. Braz J Med Biol Res 38(9):1303-1311.
- Randy A. Sansone, and Lori A. Sansone (2009) Tramadol; Seizures, Serotonin Syndrome, and Coadministered Antidepressants. Psychiatry (Edgmont) 6(4): 17–21.
- (2014) Chris Iliades. What Is Tramadol (Ultram)?. Everydayhealth.
- Suat Gormel, ,Tolga Ege, Mustafa Koklu, Murat Celik, Uygar Cagdas Yuksel (2015) Acute Lateral Myocardial Infarction Secondary to Tramadol-Induced Kounis Syndrome. Journal of Cardiothoracic and Vascular Anesthesia 29(6): 1599–1602.
- Laurent Karila, Perrine Roux , Benjamin Rolland , Amine Benyamina , Michel Reynaud , et al. (2014) Acute and Long-Term Effects of Cannabis Use: A Review. Current Pharmaceutical Design 20 (25): 4112-4118.
- Mudalige Don Vajira Malin Gunawardena, Senaka Rajapakse, Jagath Herath, Naomali Amarasena. Myocardial infarction following cannabis induced coronary vasospasm. case report. BMJ Case Rep p.1-2.
- United Nations Office on Drugs and Crime (UNODC). Why Does Cannabis Potency Matter?
- (2009) why-does-cannabis-potency-matter?
- Albert Stuart Reece (2009) Chronic toxicology of cannabis. Clinical Toricology 47: 517-524.
- Mankad R (2019) Coronary artery spasm: Cause for concern?
- Mehta PK, Thobani A, Vaccarino V (2019) Coronary Artery Spasm, Coronary Reactivity, and Their Psychological Context. Psychosom Med 81(3): 233-236.
- Liu PC, Cheng CW, Hung MJ (2010) Variant Angina with Angiographically Normal or Near-normal Coronary Arteries: A 10-year Experience. J lntern Med Taiwan 21: 79-89.
- Zaya M, Mehta PK, Merz CN (2014) Provocative testing for coronary reactivity and spasm. J Am Coll Cardiol 63(2):103-109.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...

.png)


