Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6679
Case Report(ISSN: 2637-6679) 
Relation of QRS Vector and Transverse Ring in Left Bundle Branch Block: Case Report Volume 6 - Issue 2
Hassa Iftikhar1*, Ya Li2 and Akanganyira Kasenene3
- 1Department of Cardiology, Tongji Hospital, Tongji Medical College of Huazhong University of Science and Technology (HUST). Wuhan, Hubei, PR China
- 2Department of Cardiology, Zhongnan Hospital of Wuhan University, Wuhan University, Wuhan, Hubei, PR China
- 3Department of Imaging and Nuclear Medicine, Zhejiang University, Hangzhou, PR China
Received: May 5, 2021 Published: May 20, 2021
Corresponding author: Hassa Iftikhar, Department of Cardiology, Tongji Hospital, Tongji Medical College of Huazhong University of Science and Technology (HUST). Wuhan, Hubei, PR China
DOI: 10.32474/RRHOAJ.2021.06.000237
Abstract
Background: Electrophysiological studies always remained essential to differentiate the type of pre-excitation syndrome in arrhythmia. We explore mahaim fibers’ role instead of a bundle of his in the accessory pathway to diagnose left bundle branch block. Case presentation: A asymptomatic 51-year-old man was present in the outpatient department with a history of myocardial infarction over several years. The classical pre-excitation syndrome remains classical without delta waves. Trans-esophageal atrial pacing was induced using electrocardiogram and intracardiac electrogram (IEGM) to study further morphological changes of QRS in all directions.
Diagnosis: The evaluated accessory pathway before and after ablation at anterolateral bypass potentially synchronous the transitional R wave at the electrical axis, recording the positive and negative sign readings. The morphology pattern closer to the left bypass’s origin at the frontalis concludes the left bundle branch block, which was misdiagnosed earlier with the right bundle branch block.
Conclusion: This is the first case report which elaborated the importance of retrograde study in uni-directional stimulus that significantly identified the maximum QRS terminal vector changes in rhythm disorder.
KeywordsPre-Excitation; QRS Terminal Vector; Mahaim Fiber; Left Bundle Branch Block; Ablation.
Abbreviations:ECG: Electrocardiogram; SVT: Supraventricular tachycardia; AP: Accessory pathway; PS2 : Phase segment; AH interval: Atrial his interval; AV node: Atrioventricular node; NV node: Nodo-ventricular node; STEMI: ST-elevation myocardial infarction; NSTEMI: Non-ST elevation myocardial infarction; RBBB: Right bundle branch block; LBBB: Left bundle branch block
Introduction
Pre-excitation is a typical condition in which earlier ventricular activation is determined. [1] The history of heart failure and cardiomyopathy remains prevalent to unknown risk of ventricular pre-excitation. The asymptomatic case in pre-excitation considered younger males showing the precipitating event of atrial fibrillation. The accessory pathway’s anatomic structure predisposes to site the right and left atrioventricular ring connection linking together at the junctional route of the left ventricular septum. [2,3]In most cases, the population of females and children are affected commonly in mahaim fiber. The clinical presentation varies from congenital disorder originated at the left anomaly and pulmonary venous in coronary artery disease. The aberrancy of repeated tachycardia makes no significant difference in gender, etiology, and medical history to explain the ventricular systole atomicity in the atrioventricular node. Moreover, we believe that mahaim fibers’ physiology playing a pathogenic role in the myocardium evaluates the latent type of pre-excitation that may affect the QRS terminal vector at different time phases. We comprehensively investigate the septal junctions of mahaim fiber and diagnose the bundle branch block via the atrioventricular node. The sinus PR and narrowed QRS at S2 pacing measure the time differences and velocity potential on surface ECG to evaluate the ventricular-pre-excitation degree explaining the retrograde levels. Based on the Huazhong University of Science and Technology board of Tongji Hospital, the institutional regulation reviewed no importance of ethical approval.
Case Presentation
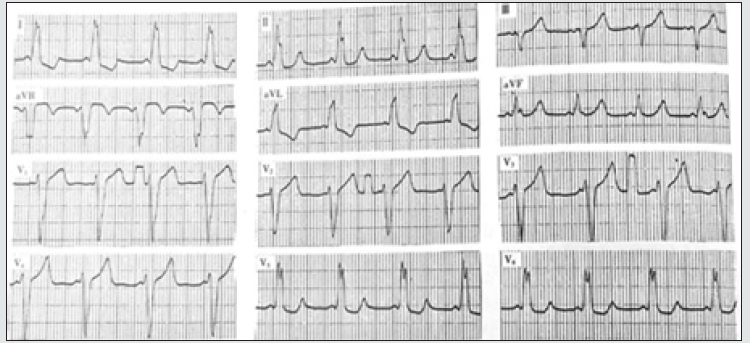
A 51-year-old male was presented with a history of Inferior Myocardial Infarction prior-8years documented with arrhythmia. He reports unbearable chest tightness several times a day, with night sweats disturbing his sleep. He presented hemodynamically stable at the outpatient clinic but was complaining of mild dizziness and palpitation. He uses beta-blockers for several years based on the doctor’s prescription but refused any syncopal history. The 12-lead ECG showed episodes of tachycardia deliberately with a reduced pulse rate. He was diagnosed with the ventricular preexcitation syndrome in the absence of SVT. To study the rhythm disorder in multiple blocked branches, an electrophysiology study was conducted to understand the morphological changes between the initial and terminal vector before and after ablation at the heart rate of 130 times/min. Before ablation, it shows PJ interval 0.24s and QRS 0.12 accompanied by ST-T changes showing no visibility of delta waves as shown in Figure 1. The QRS terminal vector relation is affected in the lead II, III, AVF, and V1+V2 lead.
During the physical examination, the auscultation and imaging findings were normal. And on determining the sinus and refractory period of the electrode in the right atrium, the heart rate of 110bpm started splitting and slowly diminished. The medication of aspirin was discontinued before the ablation procedure. The conventional 12 lead ECG technique at normal tracing positioned in the right atrium, left atrium, and right ventricle recorded the synchronized concentric atrial pacing to measure the refractory period evaluating the risk factor ventricular tachycardia and ventricular fibrillation, respectively. The lateral position of the right ventricle in the apex anatomically configures the functioning of mahaim fibers (Nodoventricle) rising from its origin of AV node collectively form 3 points transverse ring as shown in Figure 2, similar to tricuspid ring starting from the above right atrium to right bundle branch conduction fiber directly peak the ventricular muscle ending at the anterior branch. The efferent I and II limbs are located on the right side, respective to afferent III and IV limbs. It represents the uni-directional way of the circuit from the atrium to ventricle reaching the septum, which may reverse the blood flow back to the atrium dilating the left ventricle. The symmetrical changes are easily concealed and misdiagnosed by myocardial damage and ventricular hypertrophy. It identifies the mahaim fibers (NV) from the atrioventricular (AV) node and the bundle of his classifying the significance of the left bundle branch block.
Figure 2: Schematic presentation showing the relation between QRS vector and transverse volume ring in left bundle branch block.
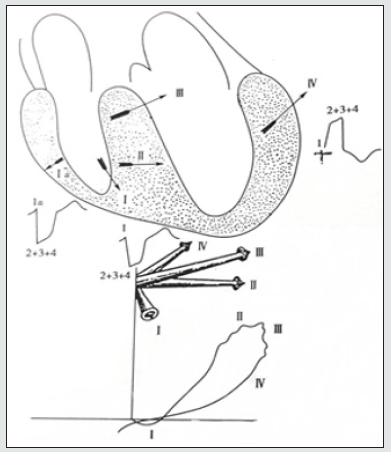
Mechanically, it passes down faster than the usual route forming eight waves. The normal way of ventricles continuously ends down with the eight waves depolarization. The bypass and the normal routes descend together to form ventricular fusion apart from the core chamber’s end. The formed myocarditis during ventricular fusion activates the impulse around itself both through the AV and AP conduction. Moreover, on having the improved nodal property, it precedes mahaim fibers’ activation instead of the bundle of his at 3 PJ interval suggesting atrioventricular (AV) block. The recorded potential in myocarditis is generated in V1+V2+V3. The differences in velocity between the atrioventricular (AV) node and AP pathway determine the latent type and 1st-degree pre-excitation in the manifestation of ECG reflecting pre-excitation. Notably, in the classical presentation of pre-excitation based on PR interval at normal heart rate, the isolated NV fiber prematurely senses P wave delaying the PS2 activation that exclusively leads to the incomplete block at right side either through AV node or left anterior AP conduction system. [4] The amplitude with the direction of the vector appears differently with the segment of 20ms and polarity of ≥2mm; it affects the initial QRS vector and affects the QRS maximum and QRS terminal vector [5].
The recording of multiple leads V1+V2+V3+V4 dynamically influences the R-R lead accuracy, showing no apparent pre-atrial contraction indicating (-) sign due to its closer origin to bypass. However, the ablation within the AV bypass increases the limb pre-exciting waves and couple the transitional R waves on the electrical axis to represent the frontalis QRS wave with the changes of 40ms equal to the potential of pre-excitation. Initially, the 40ms vector denoting (+) sign on equipotential of 8 waves lead deviate downward expressing (-) to record the combined QRS wave with pre-excited leads. The maximal QRS vector lies between 40°-80° with the magnitude of increased >2mv at the left posterior quadrant. To understand the intuitive effect on spatial vector in ablation theoretically, it is essential to measure the 1. AP localization 2. The dominance of bypass 3. QRS analysis to conclude the diagnosis
a) The accessory pathway localization lies at the atrioventricular node’s lateral ring, which shows the thickness of the accessory fascicle posterior to the leaflet of the mitral valve. The accessory pathway’s characteristic expects that the left septal junction can cause morphological changes by leading to delta waves on doubling the pathways at fibrous annulus tissues. Apart from the ventricles, the depolarization produces 400m/s velocity conduction, making 0 impulses rapidly, which ends the delta waves via a normal pathway at Purkinje fiber [6].
b) On measuring the bypass route starting from the coronary sinus, it shows more obvious (-) inverted waves at I and AVL leads compared to the deeper Q waves presented at bypass distantly are located away from the coronary sinus. The pacing is slightly greater in AH interval, prolonging pacing at the atrioventricular node (AV) to conclude the left bundle branch block. Usually, the (-) wave with the depth of (-) AVL lead occurs greater and earlier than that of lead I. This confirms Q waves’ visibility at I and AVL 8 wave leads localized at the left frontal wall bypass. Therefore, the left bypass’s dominance is noted with the depth of AVL lead between the left anterior and left posterior considering the larger (-) I lead making the changes of rS shape in V1 due to its smaller degree of pre-excitation.
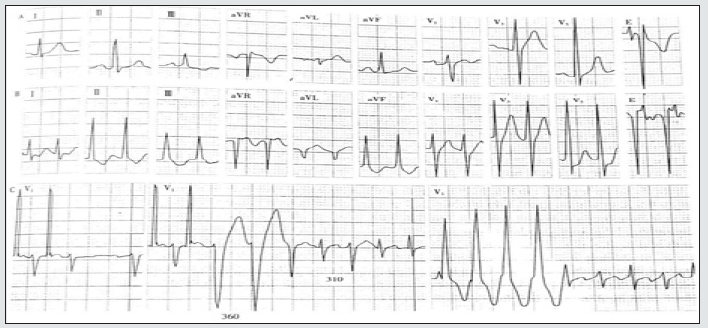
Figure 3: Occult ventricular prediction
A. Sinus rhythm, PR interval, and QRS cluster were normal
B. Directional atrioventricular re-entrant tachycardia
C. Esophageal atrial pacing fails to show bypass conduction. It induces atrioventricular reentricular tachycardia (Middle figure): the first two QRS of tachycardia presented left bundle branch block type, with RR period of 360ms, followed by QRS narrowing and R interphase 310ms indicating left latent bypass. Diagram of the mechanism of tachycardia in the center of the figure.
D. Atrial ventricular tachycardia presents wide and narrow QRS; if the time limit of wide QRS is longer, narrow QRS >35ms will be extended, indicating bypass and bundle branch bypass located on the same side, it is identified by the hidden left bypass. ECG- Sinus rhythm, atrioventricular re-entrant tachycardia with ipsilateral bundle branch block.
c) Additionally, the rS pattern in V5 and V6 displaces the QRS complex to septal activation in the existence of a heart block. But the absence of an ECG marker in ventricular activation predicts better left ventricular functions. Non-invasively, the dyssynchrony detects left bundle branch block induced by ablation show the latent activation and its variance to mahaim fiber truly identify mid and terminal end conduction delaying the (+) indication at QRS loop respectively.
d) During QRS analysis, the shape is elongated and narrowed posteriorly, ranging from 90°-40°. The delayed conduction move clockwise direction exceeds 2mV anteriorly in the magnitude of maximum QRS vector, indicating lateral infarction. The length of NV and shorter effective period of PR depolarizes symmetrically to initiate the lateral positioning at the reduced atrial septum. Simultaneously, the activation of the ventricle laterally at the left side produces an R wave with the amplitude of raised R/S ratio in lead V6 (R1 + S6) and (R6 + S1), indicating left bundle branch block as seen in figure 3.
After ending the ablation procedure, the patient was admitted to the hospital for ten days to monitor his regular heart rate and carry further testing. All lab values were found normal. The sustained tachycardia reverted to sinus rhythm by the adenosine use. He responded well to other pharmacological medication added to his diet, including Digoxin, Propranolol, and Quinidine. He confirmed no symptoms occurred after the treatment therapy.
Discussion
At present, the study of mahaim type-pre-excitation majorly brings the transmission changes at different regions showing no proper functioning and easily drop-down at the end on the transmural pathway to form the manifestation of left bundle branch block. [7] It explains bundle branch characteristics in a uni-directional way exhibit the branch block aberrancy at the accessory pathway without participating in re-entrant ventricular tachycardia. The mahaim fibers localization approach emerged from an atrioventricular node threshold that explains the study from anterograde at the right side to retrograde at the left side demonstrate the bypass tract and QRS analysis in all direction activation processes. The introduction of the standardized negative leads on EKG reading with the concept of equivalent to the criteria of STEMI in the myocardium region measure the closer leads of V2-V4, respectively. The effect of the silent myocardial infarction lesions exposed at the lateral and inferior walls inversely showing the ranges of -45°- to -90° degree angle residing at the 30̊-degree angle. The origination of the ST vector evident through the contagious ST-elevation segment extended to the maximum of II (-), III (-), and avF (-) leads to moving towards the opposite direction in the correlation of avR sub-endothelial pattern of NSTEMI. Traditionally, the inversion of nodal rhythm in inferior leads possesses automaticity of deviation from (-) sign to (+) sign representing mahaim fibers’ property. The controversy of mahaim fibers in arrhythmia, apart from the bundle of his limitedly connect septum, broadens the fibers structurally at the atrioventricular node (AV). Moreover, the dilemma of pre-excitation in the morphology of left ventricular targets relatively delays the right ventricular activation on blocking the series at the left side, resulting to cause fusion of the QRS variables—the associated anomalies including Ebstein anomaly, Klippel-Feil syndrome, rheumatic heart disease, and sick sinus syndrome. The symptom of palpitation asymptomatically at normal tracing depolarizes tachycardia resuscitation on causing flutter through the septal accessory pathway.
a) Type A’s characteristic with a free wall septal perforation of the right ventricle occasionally determines the right bundle branch block (RBBB) configuration. The appearance of lead V1 and V2 in the RBBB pattern maximizes the QRS vector’s orientation inferiorly and posteriorly at 0° -90° axis separating from V3 to begin the complication from the right ventricle to left ventricular pacing predicting (+) value of 95% - 99% [8].
b) The characteristic of Type B bundle branch block morphology activates the clockwise anterograde ventricular tachycardia re-entry.
c) Type C’s characteristic induces ventricular tachycardia on the transitional frontalis axis at the postero-lateral position of left ventricular measuring from -90 to -180 axis, respectively.
Several hypotheses based on RBBB describe the dual effect of chambers in an abnormal pathway consistently revealing the -75 anterosuperior limb lead axis, which mechanically delays the ventricular junction at the atrioventricular (AV) junction. [9] The clinical integration of ventricular pacing physiologically activates the site attributing towards the susceptibility of dilated myopathies and ischemia, which periodically propagate the epicardial leads moving to the opposite direction at a fixed blocking placement. In such a case, atrial pacing at normal QRS observes the changes in the direction of the QRS interval after blocking the atrioventricular (AV) node at ≥ 35/ms on spontaneously showing the R/S1 wave direction but remain invisible in lead V1. The ‘U’ shaped left ventricular activation in the cycle length of tachycardia reciprocates (250-260 m/sec) heterogeneously showing deflection. Accordingly, the prolonged QRS 310/ms peak “R wave” timing in v5-v6 ≥ 60/ms. Thus, the pre-cordial lead correlation in the QRS terminal vector least broadens the R wave at 360/ms exceptional to AVL and I lead differentiating from incomplete to complete bundle branch block.
Limitation of Study
Firstly, we lacked the potential of 3D mapping in our case report. Further investigations are needed to localize the distal and proximal site in fibers for recognizing the risk factor of causing atrioventricular septal blocks. Secondly, the transverse ring concept in the QRS vector relation emphasizes retrograde study more precisely after ablation, concluding that the concealed maximum terminal QRS vector concordantly affects the accessory pathway (AP). Therefore, the comparative study of hemiblock in mahaim fibers between anterograde and retrograde at accessory pathways would be a unique idea to distinguish the pre-excitation type.
Conclusion
We reported a patient with latent pre-excitation suffering from atrial fibrillation episodes with a symptom of chest tightness and syncope. We visualized that the atrioventricular node is passing down faster compared to that of the accessory pathway. EKG monitoring before ablation showed the initial vector QRS changes with the absence of delta waves due to the superior atrioventricular node functionality over the accessory pathway. And after ablation, it showed the terminal vector changes, which showed the left-sided effect in myocardial infarction predicting left bundle branch block.
Patient Perspective
Based on the patient’s clinical perspective of frequent attacks of dizziness, fatigue, and symptom of exercise intolerance, he stopped responding to antiarrhythmic drugs. The use of radiofrequency ablation remained beneficial as a radical therapy when releasing his pressurized throbbing chest pain, making him feel better, and it successfully diagnosed the left-sided bypass that was responsible for bundle branch block. Also, the drug therapy of procainamide and amiodarone was given to him post-ablation.
References
- (2002) Handbook of cardiac electrophysiology : a practical guide to invasive EP studies and catheter ablation. Murgatroyd, Francis D. London: ReMEDICA Pub.
- Anderson RH, Becker AE, Brechenmacher C (1975) Ventricular preexcitation: a proposed nomenclature for its substrates. Eur J Cardiol3: 27-31.
- Rossi L (1980) Anatomic basis of preexcitation. In: Befeler B, Lazzara R, Scherlag BJ, eds. Selected Topics in Cardiac Arrhythmias. Mount Kisco, NY: Futura Publishing Co 1980: 261–276.
- Garratt CJ, Antoniou A, Griffith MJ, Ward DE, Camm AJ (1990) Use of intravenous adenosine in sinus rhythm as a diagnostic test for unapparent preexcitation. Am J Cardiol 65: 868-873.
- Liu RG, Chen J (2013) Pre-excitation syndrome with a change in QRS terminal vector. Acta Cardiol 68: 219–221.
- Lim HS, Kuchar D, Subbiah R, et al. (2011) Secondary r’ wave in V1 as a sign of left‐sided antegrade accessory pathway conduction. Ann Noninvasive Electrocardiol 16: 407–408.
- Brugada J, Martinez-Sanchez J, Kuzmicic B, Figueiredo MO, Matas M, et al. (1995) Radiofrequency catheter ablation of atriofascicular accessory pathways guided by discrete electrical potentials recorded at the tricuspid annulus. Pacing Clin Electrophysiol 18: 1388-1394.
- Coman JA, Trohman RG (1995) Incidence and electrocardiographic localization of safe right bundle branch block configuration during permanent ventricular pacing. Am J Cardiol 76: 781-784.
- Barold SS, Narula OS, Javier RP, Linhart JW, Lister JW, Samet P (1969) Significance of right bundle-branch block patterns during pervenous ventricular pacing. Br Heart J 31: 285-290.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...

.png)