Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6679
Research Article(ISSN: 2637-6679) 
Pseudo-Infarction Patterns Leading to Undue Thrombolysis Volume 2 - Issue 5
Ahmad Hasan*, Muhammad Muzamil, Hassan Irshad, Aqib Javed, Muhammad Iqbal and Muhammad Waqas
- FCPS Cardiology , Pakistan
Received: November 19, 2018; Published: November 27, 2018
Corresponding author: Ahmad Hasan, FCPS Cardiology, Assistant Professor of Cardiology, Pakistan
DOI: 10.32474/RRHOAJ.2018.02.000147
Abstract
Background: Acute ST elevation Myocardial Infarction (MI) is a life-threatening emergency, recognized on Electrocardiogram as ST Elevation requiring urgent management in the form of reperfusion therapy. There are some other causes of ST elevation as well, that are needed to be kept in mind before giving reperfusion therapy to only to true ischemic events. This study was carried out to look for the pseudo-infarction patterns leading to undue delivery of thrombolytic therapy.
Methods: A retrospective study was done. All patients suspected of ST elevation MI given thrombolytic therapy were analyzed, with cardiac enzymes and echocardiography (ECHO), that whether the event was truly ischemic or they were unduly diagnosed and treated as infarction.
Results: There are few causes of pseudo ST Elevation that are to be looked for before giving thrombolytic therapy in suspected ST elevation MI.
Conclusion: Every ST Elevation is not an infarction so a careful approach is required to rule in and rule out infarction in emergency room.
Keywords: ST Elevation Myocardial Infarction; Pseudo-infarction; Reperfusion
Abbreviations: MI: Myocardial Infarction; STEMI: ST Elevation myocardial infarction; ECHO: Echocardiography; LBBB: Left Bundle Branch Block; LVH: Left ventricular Hypertrophy; ERP: Early repolarization pattern; ECG: Electrocardiogram; WPW: Wolf Parkinson White; STE: ST elevation; ERP: Early repolarization syndrome; ACS: acute coronary syndrome
Introduction
Acute ST Elevation myocardial infarction (STEMI) constitutes a major chunk of the health problem in public sector not only in western countries but also increasing in developing countries as well [1]. In United States, the cerebrovascular events are estimated to be more than half a million annually and these have urged strong desire not only to increase in the need of health care delivery but also the importance of better providence of management therapies. [2-4]. Acute MI due to a thrombus causing vessel occlusion is recognized on Electrocardiogram (ECG) by ST elevation [3]. Early (60 to 90) and complete patency of the infarct-related artery determines the chances of survival after acute myocardial infarction [5-7].
Reperfusion therapy, either thrombolytic or primary angioplasty, is the way to get the patency back and is known to be beneficial in such cases. Time is myocardium so earlier the achievement of flow in the vessel by reperfusion therapy, the better the chances of survival and less incidence of morbidity and mortality. Thrombolysis is the established treatment in the early management of myocardial infarction and it reduces 35 day mortality by about 25% [8]. In developing countries, where thrombolytic therapy is still the most carried out treatment than primary PCI, it is important to keep in mind that acute infarction is not the sole cause of ST elevation and similar changes of ST Elevation can be seen in patients with nonobstructive coronary artery disease meaning by having pseudoinfarction patterns [9].
Methods
Patients presenting in the emergency department of JHL during the month of July, 2017 to July, 2018 with chest pain and ST elevation in two contagious leads, thrombolysed with streptokinase on standard protocol were retrospectively analyzed. There data including the serial ECGs done on daily basis during their hospital stay for evolutionary changes, two sets of cardiac enzymes (Troponin I) for rise and fall pattern, Echocardiography (ECHO) done on 3rd or 4th post admission day for regional wall motion abnormalities, and coronary angiography within 5 days for evaluation of coronary anatomy, culprit lesion assessment and further intervention, were evaluated to confirm the true occurrence of cardiac ischemic event. The Study was approved from the ethical board review of the institution. Data was analyzed in SPSS version 22.
Results
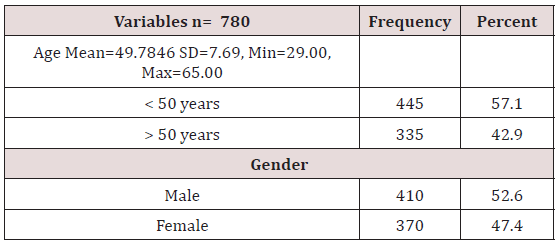
Age distribution of the patients was done which shows that 57.1% (n = 445) were less than 50 years of age while 42.9% (n = 335) were above 60 years of age, mean ± SD was calculated as 49.78 ± 7.69 years (Table 1).
Patients were distributed according to gender showing that 52.6% (n = 410) were male while 47.4% (n = 370) were female (Table 1). The mean hospital stay of the patients was 5±1 day. Among these patients 59% were of suspected anterior wall MI, 7% of inferior wall MI, 33% of inferior wall MI with RV infarct and only 01% isolated posterior wall MI. Doing analysis with the help of various modalities like ECG, ECHO, Angiography, Cardiac enzymes, total 83 (10.64%) out of 780 patients were found to be having pseudo-infarction pattern, not fulfilling the criteria of having acute ischemic event receiving thrombolytic therapy.
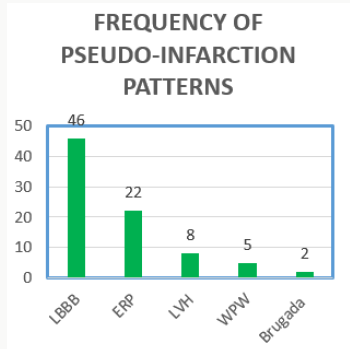
Following were the patterns with decreasing frequency: (Figure 1)
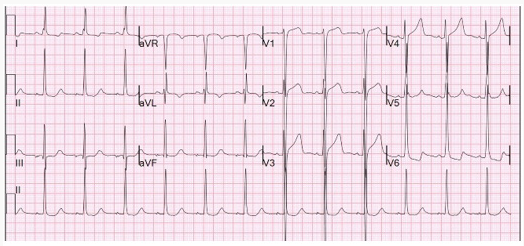
i. Left bundle branch block (LBBB) 55% (n=46)
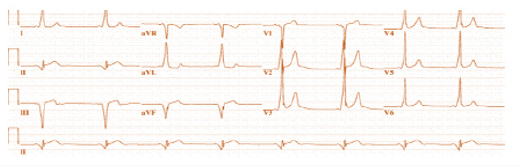
ii. Early repolarisation therapy (ERP) 26.5% (n=22)
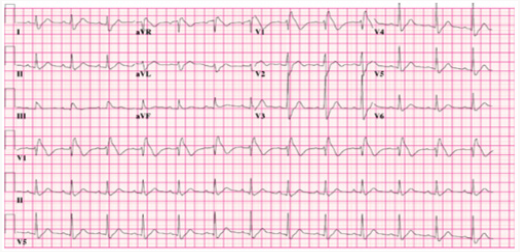
iii. Left ventricular hypertrophy (LVH) 9.63% (n=08)
iv. Wolf-parkinson-White pattern (WPW) 6.02% (n=05)
v. Brugada Syndrome 2.40% (n=02)
All 780 patients were given thrombolytic therapy with success except for three patients who became hypotensive and were not completely given thrombolytics. The mean time for SK administration was 47+-5 minutes.
Discussion
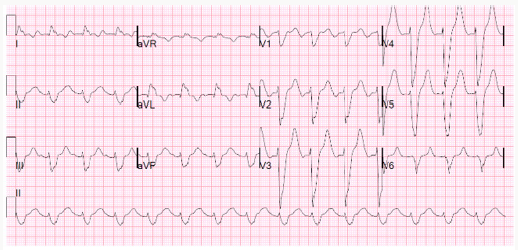
The American College of Cardiology/American Heart Association Guidelines for the Management of Patients with Acute Myocardial Infarction consider the presence of electrocardiographic ST segment elevation of >0.1 mV in two anatomically contiguous leads as a class I indication for urgent reperfusion therapy in the patient presumed to have Acute Myocardial Infarction (MI). There are several other causes of ST elevation apart from MI which have close resemblance to the ST elevation of infarction pattern like Left Bundle Branch Block (LBBB), Left ventricular Hypertrophy (LVH), Early repolarization pattern (ERP), Brugada Syndrome, Male ECG Pattern, Wolf Parkinson White (WPW) syndrome, Hyperkalemia, Pericarditis, etc [10]. These patterns are misinterpreted as acute infarction and sometimes given undue thrombolytic therapy. Elevation of the ST segment due to non-ischemic etiologies was reported up to 15% in the general population. Goldberger et al [11] through his study showed that the LBBB pattern is one of the most commonly misinterpreted pseudo-infarct pattern encountered in emergency room, resulting in inappropriate treatment. Of the patients with LBBB having STEMI protocol initiation, only 39% had a final diagnosis of actual ACS, 36% do turned out to have cardiac diagnoses but other than ACS which may be hypertensive emergency, acute heart failure, atrial fibrillation, severe aortic stenosis, etc. and 25% had non-cardiac diagnosis [10,11] (Figure 2).
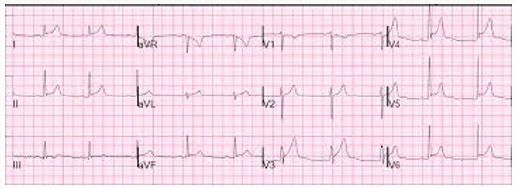
The LBBB causes significant changes in the depolarization and repolarization masking the acute changes caused by infarction. There are number of proposed criteria’s which help in the differentiation of acute LBBB due to acute ischemia/infarction. Sgarbossa et al [13] proposed an algorithm based on ST-segment changes having a sensitivity of 78% and a specificity of 90% for the diagnosis of MI. The criteria comprises of three points including ≥ 0.1 mV of concordant ST elevation (STE) or ≥ 0.1 mV ST depression in leads V1 to V3 with discordant STE ≥ 0.5 mV in leads while smith and colleagues [14] found replacing the third criteria of > 5mm absolute deviation in leads with discordant QRS complex with an ST/S ratio ≤ -0.25 increasing the sensitivity to around 91% keeping specificity same. Our study also confirms the same results showing LBBB prevalence to be 55%, making the most common pseudo-infarction pattern, leading to a diagnostic dilemma for emergency physicians in making correct diagnosis. The second most common cause in our study for undue activation of thrombolytic protocol came out to be Early repolarization syndrome (ERP). It has been called by a variety of names including “unusual RT Segment deviation”, “premature repolarisation“, normal RS-T elevation variant”, and “early repolarisation syndrome” [15]. The “early repolarization” pattern is usually found 1% to 5% in the population [16-17] most commonly found in young, athletic, black males [15,18] but this distribution is not rare in women, older persons, whites and inactive persons [15]. The mechanism of early repolarisation is not completely understood; although accumulating evidence suggests a vagal origin [16,19]. In the past, early repolarization pattern was considered a benign pattern [18] but now it has its own association with cardiac morbidity and mortality. Even then the presence of ERP doesn’t warrant administration of thrombolytic therapy (Figure 3).
It is diagnosed when there is no S wave in V3; Concave STsegment elevation of 1-4 mm in leads V2-V5 (most prominent in V3) and may be in inferior leads; and notching of the down-stroke of the R waves (“J” wave), most prominent in lead V5 and V6 [15]. Additional ECG criteria for the ERP include reciprocal ST segment elevation in AVR and waxing and waning of the ST Segment over time [20]. Early repolarisation of the ST segment is an electrocardiographic variant with a benign long-term prognosis [15]. Larsen et al. [21] have shown that hypertrophy of the left ventricle (LVH) is incorrectly interpreted more than 70% of the time in patients thought to have an acute coronary syndrome (ACS). Failure to make this diagnosis is responsible for large financial payments in the medico legal arena involving malpractice cases against emergency physicians [22-23]. Retrospective analysis of a significant minority of these cases has revealed that misinterpretation of the ECG has played a role in as many as 25% of the cases [23] (Figure 4). ST Elevation due to LVH is usually seen in leads V1-V3. Typically, there are QRS amplitude criteria for hypertrophy of the left ventricle and ST segment depressions in the lateral wall leads (V5-V6 and I and aVL). As the amount of LV mass increases, proportionately the ST segment chnges also increase rendering more difficullty in the diagnosis [24]. LVH and bundle branch block represent other frequently encountered patterns in three studies [25-26], which were either misinterpreted or interpreted with disagreement among the interpreters.
Wolff-Parkinson-White is a pre-excitation syndrome, having a accessory pathway leading to characteristic ECG changes of short PR interval, delta waves, wide QRS complexes, and Q wave-T wave vector discordance, with a prevalence rate of about 0.1 to 3.1 per 1000 persons in general population [27]. The pseudo-infarct Q waves resulting from secondary repolarization changes due to altered ventricular activation [28] mimic true infarction, so special attention must be given to make a proper diagnosis. (Figure 5) It is interesting to mention that one of the gentlemen in our study was thrombolyzed twice over a period of 01 year having WPW pattern. Brugada pattern is another pattern mimicking ST elevation associated with a pattern resembling RBBB with elevation of the ST segment in the precordial leads (V1-V2) [29-30]. The Brugada syndrome, though, is linked to an increased risk of ventricular arrhythmia and sudden cardiac death secondary to defect in NA channel transport system, but is not an acute cardiac emergency requiring reperfusion therapy. There are mainly three types of Brugada patterns but type I is the most common misinterpreted pseudo-infarct pattern due to a saddle shape ST elevation in V1-V3 but without reciprocal changes (Figure 6). There was a prevalence rate of 2.40% of this pattern in our population presenting in emergency departments getting reperfusion therapy.
The thrombolytic therapy has its own side effects, some of which may be life threatening like intra cranial bleed, major bleeding requiring transfusion, hypersensitivity reactions etc., [31]. Inappropriate fibrinolysis is not without morbidity and mortality [32-34] and any reduction in undue administration of the therapy would be beneficial resulting less complication rates. Also, the thrombolytic therapy also poses a financial burden especially in developing countries like ours where still the emergency services are not completely free yet. There is another way of seeing the thing that if a patient is unduly thrombolyzed, he might be needing in future thrombolysis for a true ischemic event rendering a relative contraindication within next 6 months. So recognition of these patterns is very necessary for accurate supply of thrombolytic therapy for proper management, avoidance of complications and saving cost burden on the patient as well as health system.
References
- Antman EM, Anbe DT, Armstrong PW, Bates ER ,Green LA, et al. (2004) ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology / American Heart Assiciation Task Force Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infarction. J Am Cardiol 44(3): 671-719.
- Thygesen K, Alpert JS, White HD, Allan S. Jaffe Fred S Apple, et al. (2007) Universal definition of myocardial infarction: Kristian Thygesen, Joseph S, Alpert, Harvey D White on behalf of the Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Eur Heart J 28(20): 2525-2538.
- Ryan TJ, Antman EM, Brooks NH, Anderson JL, Braniff BA, et al. (1996) ACC/AHA guidelines for the management of patients with acute myocardial infarction. A report of the American College of Cardiology/ American Heart Assocation Task Force on Practice Guidelines [Committee on Management of Acute Myocardial infarction].J Am Coll Cardiol 28(5): 1328-1428.
- The GUSTO Angiography Investigators (1993) The effects of tP, Streptokinase, or both on coronary angiography patency, ventricular function, and survival after acute myocardial infarction. N Engl J Med 329(22): 1615-1622.
- ML. Stadius (1993) Angiographic monitoring of repolarisation therapy for acute myocardial infarction: TIMI grade 3 perfusion is the goal. Circulation 87(6): 2055-2057.
- JW Kennedy (1995) Optimal management of acute myocardial infarction requires early and complete reperfusion. Circulation 91(7): 1905-1907.
- ISIS-2 (Second International Study of Infarct Survival) Collaborative Group (1988) Randomized trial of Intravenous Streptokinase, oral aspirin, both or neither among 17187 cases of suspected acute myocardial infarction: ISIS-2. Lancet 12(6): 349-360.
- Cheng TO (1987) The International Textbook of cardiology. New York, USA: Per-gamon: 72-73.
- WANG K, Asinger RW, Marriot HJL (2003) ST-Segment elevation in conditions other than acute mi. N Eng J Med 349(22): 2128-2135.
- Mehta N, Huang HD, Bandeali S, Wilson JM and Birnbaum Y (2012) Prevalence of acute myocardial infarction in patients with presumably new left bundle-branch block. J Electrocardiol 45(4): 361-367.
- AL Goldberger (1991) Myocardial Infarction: Electrocardio-graphic Differential Diagnosis. (4th edn), Mosby, St. Louis, USA.
- Jain S, Ting HT, Bell M, Bjerke CM, Lennon RJ, et al. (2011) Utility of left bundle branch block as a diagnostic criterion for acute myocardial infarction. Am J Cardiol. 107(8): 1111-1116.
- Sgarbossa EB, Pinski SL, Barbagelata A, Underwood DA,Gates KB, et al. (1996) Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. N Engl J Med 334(8): 481-487.
- Smith SW, Dodd KW, Henry TD, Dvorak DM, Pearce LA (2012) Diagnosis of ST-elevation myocardial infarction in the presence of left bundle branch block with the ST-elevation to S-wave ratio in a modified Sgarbossa rule. Ann Emerg Med 60(6): 766-776.
- Klatsky AL1, Oehm R, Cooper RA, Udaltsova N and Armstrong MA (2003) The ERP normal variant electrocardiogram: Correlates and consequences. Am J Med 115(3): 171-177.
- Mehta MC, Jain AC (1995) Early repolarization on scalar electrocardiogram. Am J Med Sci 309(6): 305-311.
- Mehta M, Jain A, Mehta A (1999) Early repolarisation. Clin Cardiol 22(2): 59-65.
- Tikkanen JT, Anttonen O, Junttila MJ, Aro AL, Kerola T, et al. (2009) Long-term outcome associated with early repolarization on electrocardiography. N Engl J Med 361: 2529-2537.
- Haydar ZR, Brantley DA, Gittings NS, Wright JG, Fleg JL (2000) Early repolarization: an electrocardiographic predictor of enhanced aerobic fitness. Am J Cardiol 85(2): 264-266.
- Gussak I, Antzelevitch C (2000) Early repolarisation syndrome: clinicl characteristics and possible cellular and ionic mechanism. J Electrocardiol 33(4): 299-309.
- Pope JH, Aufderheide TP, Ruthazer R, Woolard RH, Feldman JA, et al. (2000) Missed diagnoses of acute cardiac ischemia in the emergency department. N Engl J Med 342(16): 1163-1170.
- Karcz A, Holbrook J, Burke MC, Doyle MJ, Erdos MS, et al. (1993) Massachusetts emergency medicine closed malpractice claims: 1988- 1990. Ann Emerg Med 22(3): 553-559.
- Rusnak RA, Stair TO, Hansen K, Fastow JS (1989) Litigation against the emergency physician: common features in cases of missed myocardial infarction. Ann Emerg Med 18(10): 1029-1034.
- Estes EH Jr , Jackson KP (2009) The electrocardiogram in left ventricular hypertrophy: past and future. J Electro cardiol 42(6): 589-592.
- Rude RE, Poole WK, Muller JE, Turi Z, Rutherford J, et al. (1983) Electrocardiographic and clinical criteria for recognition of acute myocardial infarction based on analysis of 3697 patients. Am J Cardiol 52(8): 936-942.
- Otto LA, Aufderheide TP (1994) Evaluation of ST segment elevation criteria for the prehospital electrocardiographic diagnosis of acute myocardial infarction. Ann Emerg Med 23(1): 17-24.
- Al-Khatib SM, Pritchett EL (1999) Clinical features of Wolff-Parkinson- White syndrome. Am Heart J 138(3 Pt1): 403-413.
- Goldberger AL (1980) Pseudo-infarct patterns in the Wolff-Parkinson- White syndrome: Importance of Q wave-T wave vector discordance. J Electrocardiol 13(2): 115-118.
- Antzelevitch C, Nof E (2008) Brugada syndrome: recent advances and controversies. Curr Cardiol Rep 10(5): 376-383.
- Brugada P, Brugada R, Brugada J (2000) The Brugada syndrome. Curr Cardiol Rep 62(11): 1297-315.
- Sgarbossa EB, Pinski SL, Barbagelata A, Underwood DA, Gates KB, et al. (1996) Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle branch block. N Engl J Med 334(8): 481-487.
- Rogers WJ, Bowlby LJ, Chandra NC, French WJ, Gore JM, et al. (1994) Treatment of myocardial infarction in the United States (1990 to 1993). Observations from the National Registry of Myocardial Infarction. Circulation 90(4): 2103-2114.
- Ryan TJ, Anderson JL, Antman EM, Braniff BA, Brooks NH, et al (1996) Committee on the Management of Acute Myocardial Infarction, ACC/ AHA Guidelines for the Management for Patients with Acute Myocardial Infarction. J Am Coll Cardiol 94(9): 2341-2150.
- Ryan TJ, Antman EM, Brooks NH, Califf RM, Hillis LD,et al (1999) Committee on the Management of Acute Myocardial Infarction, 1999 update: ACC/AHA Guidelines for the Management for Patients with Acute Myocardial Infarction. J Am Coll Cardiol 34(3): 890-911.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...

.png)