Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6679
Review Article(ISSN: 2637-6679) 
Overview of COVID19 In Hypertension Patients Volume 5 - Issue 4
Sarah Alqurmalah*
- MBBS College of Medicine, Majmaah University, Kingdom of Saudi Arabia
Received: September 14, 2020; Published: September 24, 2020
Corresponding author: Sarah Ibrahim Alqurmalah, MBBS College of Medicine, Majmaah University, Kingdom of Saudi Arabia
DOI: 10.32474/RRHOAJ.2020.05.000220
Abstract
Introduction: The coronavirus disease 2019 (COVID-19) is worldwide outbreak. Globally there are 21,159,730 reported confirmed cases and there is almost no country in the world that is not affected by COVID-19 (3). It is caused by severe acute respiratory syndrome coronavirus 2 respiratory syndrome coronavirus 2 (SARS-CoV-2) enter the cells through angiotensin converting enzyme 2 (ACE2) receptor that act as key regulator of blood pressure.
Objective: To summarize the most updated data on COVID-19 and hypertension.
Methodology: A PubMed and UpToDate search was completed in Clinical Queries using the key terms ‘COVID-19 in hypertension patients ‘and ‘COVID-19 ‘. The search strategy included meta-analyses, randomized controlled trials, clinical trials, observational studies, and reviews.
Result: 1099 patients with confirmed COVID-19, of which the single highest risk factor of infection was hypertension reported in 15% of patients. Meta-analysis of six studies (1527) patients, hypertension was present in 17.1% of patients with the infection. The median age of SARS-CoV-2–positive patients who died was 78.5 years. significantly higher usage of ARBs in hypertensive patients with moderate COVID-19 disease than those with a severe and critical course of disease. There is no advantage to any group of medications within RAAS inhibitors. There are no data regarding the association between RAAS inhibitors and the outcome.
Conclusion: There is a relation between COVID-19 and HTN and need more data to be clarify weather HTN is isolated risk factor or as a reflection of ACEI or ARB. Age is associated with COVID19.
Abbreviations: COVID-19; Hypertension; ACE; ARB
Introduction
The coronavirus disease 2019 (COVID-19) is worldwide outbreak (1). Globally there are 21,159,730 reported confirmed cases (2) and there is almost no country in the world that is not affected by COVID-19 (3). It is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection (4) a positive stranded RNA virus (5). It transmitted animal to person and person to person. During this outbreak person to person is the main mode of transmission. The transmission occurs through respiratory droplets; when a person with infection coughs or sneezes he or she can infect another close-range contact person (5) respiratory syndrome coronavirus 2 (SARS-CoV-2) enter the cells through angiotensin converting enzyme 2 (ACE2) receptor (6). It catalyzes the conversion of angiotensin II to angiotensin I (7) ACE2 receptor act as key regulator of blood pressure. High or uncontrolled blood pressure cause the patient a preventable cardiovascular disease witch is a leading cause of morbidity and mortality globally (8) Alot of studies have been raising the question about the relation between COVID- 19 and hypertension. A lot of published article reviews, retrospectives and metaanalysis regard the association between COVID 19 and hypertension. Here, we summarize the most updated data on COVID-19 and hypertension.
Hypertension
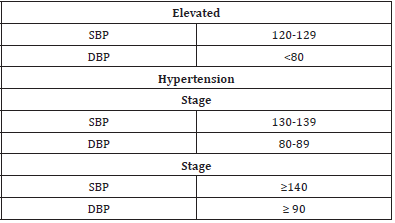
Hypertension defined as a systolic blood pressure (BP) ≥130 or diastolic BP ≥80 mm Hg by American collage academy (8). It is determined by at least two measurements in the clinic setting one minute at least apart (10). Globally, 1 in 4 men and 1 in 5 women diagnosed with chronic HTN (11.12). Raised blood pressure is a major risk factor for chronic heart disease, stroke, and coronary heart disease. It is a global cause of mortality (13) (Table1).
Other complication of hypertension including heart failure, peripheral vascular disease, renal impairment, retinal hemorrhage, and visual impairment (14) hypertension symptomless so it consider a silent killer (15) Singh and Shikha summarized the hypertension risk factor in their study to : male, elderly, married subjects, upper socioeconomic status, illiterate, retirement , tobacco and alcohol consumption, overweight and obesity (15).
The association of HTN and COVID-19
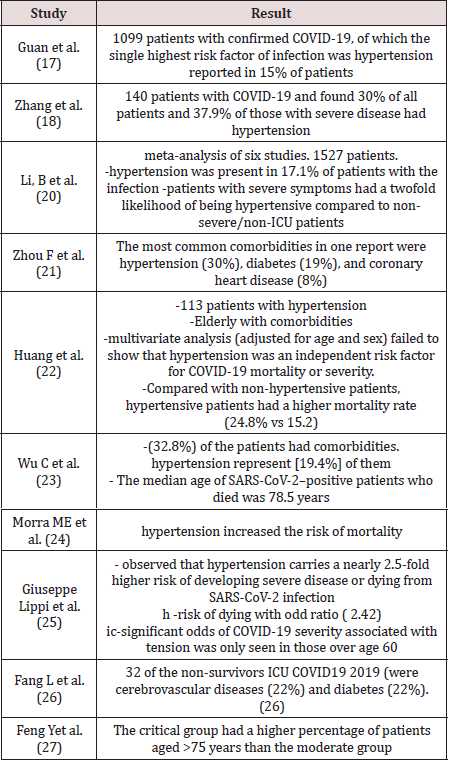
The concern about the relationship between hypertension and COVID19 was the concern of many studies. Since the pathogenesis of COVID19 interact with ACE2 receptors a one of the components of the renin-angiotensin system (RAS) (16) that paly rule in blood pressure regulation. Hypertension is the highest risk factor of COVID- 19 patients regard Guan et al study of 1099 patient with confirmed COVID-19 (17). Zhang et al. result that 30% of 140 patients of COVID19 suffer from HTN (18). Although Kulkarni et al comment on Guan et al and Zhang et al with unknown timing of hypertension diagnosis, antihypertensive medication usage and adherence and control of hypertension and since the rapidity of the data collection in the current climate it has have limitations. (19) Meta-analysis of Li, B et al on 1527 COVID 19 patient found 17.1% suffer from HTN and there are suffering from COVID-19 severity by 2 fold than non HTN (20) and the most comorbidities in COVID19 is hypertension witch represent (30%) of the patients (21) On other hand - multivariate analysis of Huang et al failed to show that hypertension was an independent risk factor for COVID-19 mortality or severity .(22) In Wu C st al study (32.8%) of the patients had comorbidities . hypertension represent [19.4%] of them, then diabetes 10.9%, liver disease [3.5%], nervous system disease [3.5%], chronic lung disease 2.5%, chronic kidney disease 1.0%, non-diabetes endocrine diseases 1.0% then tumors 0.5% (23). Regarding the mortality of COVID-19, hypertension is risk factor of mortality (24) and high risk of dying with odd ratio ( 2.42) and higher risk of developing severe disease or dying from SARS-CoV-2 infection with 2.5-fold (25) in another study 32 of the non-survivors from a group of 52 intensive care unit patients with novel coronavirus disease 2019 (COVID-19 were cerebrovascular diseases (22%) and diabetes (22%) without assessing the treatment (26) All the previous study there was no assessment of antihypertension treatment intake or age of the patients.
The association of age and COVID-19
Is the association of hypertension with covid-19 anything
more than a reflection of the age of hypertensive patients? Because
HTN prevalence increases in parallel with aging, this pattern may
represent the expected prevalence for the given age group (23)
There is lack of data in age group and association with COVID19
Giuseppe Lippi et al meta-regression showed significant odds
of COVID-19 severity with hypertension was only seen in those
over age 60 years old (25). And in another study the median age
of SARS-CoV-2–positive patients who died was 78.5 years (median,
80 years; range, 31-103 years; interquartile range, 73 to 85 years)
(23) A retrospective study from three hospitals designated for the
treatment of COVID- 19 Jinyintan Hospital in Wuhan, Shanghai
Public Health Clinical Center in Shanghai, and Tongling People’s
Hospital in Anhui Province, China , the critical group that had a
higher percentage of patients are aged >75 (27)(Table2).
ACE2 and ARB
SARS-COV-2 enter the cells through angiotensin converting
enzyme 2 (ACE2) receptor (6). which is expressed by epithelial cells
of the blood vessels, lung, intestine and kidney (25) ACE inhibitors
and angiotensin receptor blockers (ARBs) are antihypertensive
medication upregulate the ACE2 (26) and inceases its expression
. Consequently, the increased expression of ACE2 would facilitate
infection with COVID-19 (28) by supplying SARS-CoV-2 with a
more of “anchors” for infecting cells (25) RAAS activation plays a
major pathogenic role in HTN through hemodynamic actions and
cytokines and intracellular signaling pathways, which ultimately
promote many adverse cellular processes result in systemic
damage. (29) Many hypothesis been raising about which is more
beneficial or should withdrawing the medication? Although the
number of fatal COVID-19–positive patients treated with ACEIs was
more than twice the number of those treated with ARBs, it cannot
definitely conclude the risks or benefits of these therapies due to
confounding variables of age, HTN, and impact of yet-unidentified
comorbidities on outcome with the COVID-19 pandemic. (23)
ACE2 limits the adverse vasoconstrictor and profibrotic effects
of Ang II through its degradation and by counteracting its actions
through the formation of Ang 1-7. The high expression of ACE2 in
heart, type II alveolar cells, capillary endothelium, and enterocytes
demonstrates its essential role in the CV and immune systems,
being principally involved in heart function and the development of
HTN and complications of diabetes mellitus (DM) Sanchis- Gomar
et al study suggest that ARBs might be a better treatment option in
COVID-19 patients at higher risk of severe forms of disease due to
the equal efficacy but fewer side effects than ACEIs (30-32).
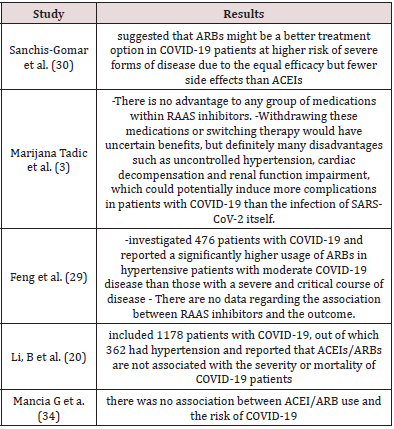
A report of 476 patients with COVID-19 that moderate
COVID-19 hypertensive patients are higher usage of ARBs with
than those with a severe and critical course of the disease and there
are no data regarding the association between RAAS inhibitors
and the outcome (33) on other hand Marijana Tadic et al study
conclude that no advantage to any group of medications within
RAAS inhibitors. (3)and there was no association between ACEI/
ARB use and the risk of COVID- 19 (34) and there is no association
with the severity or mortality of COVID-19 patients (20) Regarding
Withdrawing these medications or switching therapy would
have uncertain benefits, but definitely many disadvantages such
as uncontrolled hypertension, cardiac decompensation and
renal function impairment, which could potentially induce more
complications in patients with COVID-19 than the infection of
SARS-CoV-2 itself (34) (Table3).
References
- WHO (2020) Coronavirus disease 2019 (COVID-19)?
- (2020) COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU).
- Tadic M, Cuspidi C, Mancia G, Dell'Oro R, Grassi G (2020) COVID-19, hypertension and cardiovascular diseases: Should we change the therapy?. Pharmacol Res 158: 104906.
- Gorbalenya AE, Baker SC, Baric RS, et al. (2020) The species Severe acute respiratory syndromerelated coronavirus: classifying 2019-nCoV and naming it SARS- CoV-2. Nature Microbiology. 5(4): 536-544.
- Kenneth McIntosh (2020) Coronavirus disease 2019 (COVID-19): Epidemiology, virology, and prevention.
- Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, et al. (2020) Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell. 181(2):281-292.e6.
- Tikellis C, Thomas MC (2012) Angiotensin-Converting Enzyme 2 (ACE2) Is a Key Modulator of the Renin Angiotensin System in Health and Disease. Int J Pept. (5): 256294.
- Arnett DK, Blumenthal RS, Albert MA, et al. (2019) ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. J Am Coll Cardiol 74: e177–232.
- Whelton PK, Carey RM, Aronow WS, Casey DE, Jr, Collins KJ, et al. (2018) ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American heart association Task Force on clinical practice guidelines. Circulation. 2017;138(17): e426–e483.
- Ferdinand KC, Vo TN, Echols MR (2020) State-of-the-Art review: Hypertension practice guidelines in the era of COVID-19. Am J Prev Cardiol 2:100038.
- Arnett DK, Blumenthal RS, Albert MA, Buroker AB, et al. (2019) ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American heart association Task Force on clinical practice guidelines. Circulation 140(11): e596–e646.
- Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, et al. (2020) Heart disease and stroke statistics-2020 update: a report from the American heart association. Circulation. 141(9): e139–e596.
- Hypertension (2020) https://www.who.int/health- topics/hypertension/#tab=tab_12020 World Health Organization at. Accessed on 2020.
- Mendis (2010) “Global status report on non-communicable diseases 2010,” Tech Rep, World Health Organisation.
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, et al. (2003) Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 42(6): 1206-1252.
- Shibata S, Arima H, Asayama K et al. (2020) Hypertension and related diseases in the era of COVID-19: a report from the Japanese Society of Hypertension Task Force on COVID-19. Hypertens Res.
- Guan WJ, Ni, ZY, Hu, Y, et al. (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 382(18).
- Zhang JJ, Dong X, Cao, YY, et al. (2020) Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 75(7):1730-1741.
- Spoorthy Kulkarni, Bernadette L, Jenner and Ian Wilkinson (2020) COVID-19 and hypertension. Journal of the Renin-AngiotensinAldosterone System. P:1–5.
- Li B, Yang, J, Zhao, F, et al. (2020) Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 109(5):531-538.
- Zhou F et al. linical Course and Risk Factors for Mortality of Adult Inpatients With COVID-19 in Wuhan, China: A Retrospective Cohort Stud
- Huang S, Wang J, Liu F, et al. (2020) COVID-19 patients with hypertension have more severe disease: a multicenter retrospective observational study. Hypertens Res 43: 824–831.
- Wu C, Chen X, Cai Y, et al. (2020) Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients with Coronavirus Disease 2019 Pneumonia in Wuhan. JAMA Intern Med 180 (7):1-11.
- Morra ME, Van Thanh L, Kamel MG, Ghazy AA, Altibi AMA, Dat LM, et al. (2018) Clinical outcomes of current medical approaches for Middle East respiratory syndrome: a systematic review and meta-analysis. Rev Med Virol 28: e1977.
- Giuseppe Lippi et al. (2020) Hypertension and its severity or mortality in Coronavirus Disease 2019 (COVID19): a pooled analysis. Pol Arch Intern Med 130(4):304-309.
- Fang L, Karakiulakis G, Roth M (2020) Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 8(4): e21.
- Feng Y, Ling Y, Bai T, Xie Y, Huang J, et al. (2020) COVID-19 with different severity: a multi-center study of clinical features. Am J Respir Crit Care Med 201(11):1380-1388.
- Yang X, Yu Y, Xu J, et al. (2020) Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 8(5).
- Velkoska E, Patel SK, Burrell LM, et al. (2016) Angiotensin converting enzyme 2 and diminazene: role in cardiovascular and blood pressure regulation. Curr Opin Nephrol Hypertens 25(5):384–395.
- Hamming I, Timens W, Bulthuis ML, Lely AT, et al. (2004) Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus: a first step in understanding SARS pathogenesis. J Pathol 203(2):631–637.
- Turner AJ, Hiscox JA, Hooper NM (2004) ACE2: from vasopeptidase to SARS virus receptor. Trends Pharmacol Sci 25(6): 291–294.
- Sanchis Gomar F, Lavie CJ, PerezQuilis C, Henry BM, Lippi G, et al. (2020) Angiotensin-Converting Enzyme 2 and Antihypertensives (Angiotensin Receptor Blockers and Angiotensin-Converting Enzyme Inhibitors) in Coronavirus Disease 2019. Mayo Clin Proc 95(6): 1222–1230.
- Feng Y, Ling Y, Bai T, Xie Y, Huang J, et al. (2020) COVID-19 with different severity: a multi-center study of clinical features. Am J Respir Crit Care Med 201(11):1380-1388.
- Mancia G, Rea F, Ludergnani M, Apolone G, Corrao G (2020) Renin-angiotensin- Aldosterone system blockers and the risk of Covid-19. N Engl J Med 382(25):2431-2440.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...

.png)