Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6679
Review Article(ISSN: 2637-6679) 
OSMF-A Review Volume 2 - Issue 1
Neha Aggarwal* and Sumit Bhateja
- Department of Oral Medicine & Radiology, Manav Rachna Dental College & Hospital, India
Received: May 18, 2018; Published: May 23, 2018
Corresponding author: Neha Aggarwal, Senior Lecturer (MDS), Department of Oral Medicine & Radiology, Manav Rachna Dental College & Hospital, Faridabad (Haryana)
DOI: 10.32474/RRHOAJ.2018.02.000128
Abstract
Oral submucous fibrosis is a premalignant condition that has received considerable attention in the recent past because of its chronic debilitating and resistant nature. In 600 B.C, Sushruta a well-known expert on Indian Medicine described in his classification of mouth and throat maladies mentioned about a condition (VIDARI) the features of which were progressive narrowing of mouth, depigmentation of oral mucosa and pain on taking food. The present article discusses etiopathogenesis, clinical features and medical management of this disease entity.
Keywords: OSMF; Pathogenesis; Review
Introduction
Oral submucous fibrosis is a premalignant condition that has received considerable attention in the recent past because of its chronic debilitating and resistant nature. It is now strongly believed that there is a definite relation of the condition with the habit of areca nut chewing [1]. Areca nut has been deeply rooted in Indian culture and been used as a mouth-freshening agent that has had various symbolic roles throughout Indian history [2]. The potential for malignant transformation in submucous fibrosis is considered high, and the disease affects persons of all ages and both sexes across the Indian subcontinent. Perhaps what is most disturbing about the condition is that it affects a number of adolescents as well. The disease occurs mainly in Indians. It affects between 0.2%-1.2% of urban population attending dental clinics in India. Pindborg JJ [3] defined oral submucous fibrosis an insidious, chronic condition that can affect any part of the oral cavity and sometimes even the pharynx. Although occasionally preceded by and/or associated with vesicle formation, OSF is always associated with juxta-epithelial inflammatory reaction followed by fibroelastic changes to the lamina propria with epithelial atrophy leading to stiffness of oral mucosa and causing trismus and inability to eat [3]. Rajendranelaborated Submucous fibrosis is an insidious, chronic disease affecting any part of the oral cavity and sometimes the pharynx. Occasionally it is preceded by and/or associated with vesicle formation and is always associated with a juxta-epithelial inflammatory reaction followed by progressive hyalinization of the lamina propria. The later subepithelial and submucosal myofibrosis leads to stiffness of the oral mucosa and deeper tissues with progressive limitation in opening of the mouth and protrusion of the tongue, thus causing difficulty in eating, swallowing and phonation [4].
Malignant Potential and OSMF
The precancerous nature of OSMF was first postulated by PAYMASTER in 1956, who described the development of a slow growing squamous cell carcinoma in one third of OSMF cases seen in Tata Memorial Hospital Bombay [5]. Epithelial dysplasia in OSF tissues appeared to vary from 7 to 26% depending on the study population .However, according to the current awareness of the disease and some refined criteria for grading dysplasia, it is reasonable to assume that the prevalence of dysplasia is more towards the midway of the reported range. Malignant transformation rate, of OSF was found to be in the range of 7-13% [1]. The hypothesis that dense fibrosis and less vascularity of the corium, in the presence of an altered cytokine activity creates a unique environment for carcinogens from both tobacco and areca nut to act on the epithelium is widely being accepted.
Some Common Classifications of OSMF
Khanna and Andrade [1] categorized OSF into different stages, as follows.
I. Group I: Very early
a. Normal mouth opening
b. burning sensation
c. Excessive salivation
d. Acute ulceration and recurrent stomatitis
II. Group II: Early cases
a. Mouth opening : 26-35mm (interincisal opening)
b. Soft palate and faucial pillars as the areas primarily affected
c. Buccal mucosa appears mottled and marbled, with dense, pale, depigmented and fibrosed areas alternating with pink normal mucosa.
d. Red erythematous patches
e. Widespread sheets of fibrosis
III. Group III: Moderately advanced
a. Mouth opening: 15-25mm (interincisal opening)
b. trismus
c. Vertical fibrous bands can be palpated and are firmly attached to underlying tissue
d. Patient unable to puff out the cheeks or whistle
e. Soft palate - fibrous bands seen to radiate from the pterygomandibular raphe or anterior faucial pillar in a scar-like appearance.
f. Lips -atrophy of vermillion border
g. Unilateral posterior cheek involvement with only ipsilateral involvement of the faucial pillar and soft palate, and mouth opening reduced to 15-18mm.
IV. Group IV (a): Advanced cases
a. Stiffness/inelasticity of oral mucosa
b. trismus
c. Mouth opening: 2-15mm (interincisal opening)
d. fauces thickened, shortened and firm on palpation
e. Uvula seen to be involved, as a shrunken, small and fibrous bud
f. Tongue movement restricted
g. Papillary atrophy (diffuse)
h. Lips -circular band felt around entire mouth
i. Intraoral examination is difficult
V. Group IV (b): Advanced cases with premalignant and malignant changes
V. Group IV (b): Advanced cases with premalignant and malignant changes
a. Oral submucous fibrosis and leukoplakia
b. Oral submucous fibrosis and squamous cell carcinoma
Ranganathan K et al (2001) used a baseline study on the mouth opening parameters of normal patients and divided the OSMF patients as:
i. Group I: Only symptoms, with no demonstrable restriction of mouth opening.
ii. Group II: Limited mouth opening 20mm and above.
iii. Group III: Mouth opening less than 20 mm.
iv. Group IV: OSMF advanced with limited mouth opening. Precancerous or cancerous changes seen throughout the mucosa.
Rajendran R [6] reported the clinical features of OSMF as follows:
a) Early OSMF: Burning sensation in the mouth. Blisters especially on the palate, ulceration or recurrent generalized inflammation of the oral mucosa, excessive salivation, defective gustatory sensation and dryness of mouth.
b) Advanced OSMF: Blanched and slightly opaque mucosa, fibrous bands in buccal mucosa running in vertical direction. Palate and the faucial pillars are the areas first involved. Gradual impairment of tongue movement and difficulty in mouth opening.
Bailoor Dn and Nagesh Ks [7]:
I. Grade 1 (Mild OSMF):
a) Mild blanching
b) No restriction in mouth opening, Central incisor tip to tip of the same side, Normally in Males 5.03 cm. Females 4.5 cm
c) No restriction in tongue protrusion, mesio incial angle of upper central incisor to the tip of the tongue when maximally extended with mouth wide open (Normally Males 6.73cm and Females 6.07cm)
d) Cheek flexibility, CF= V1-V2. Two points measured between at one third the distance from the angle of the mouth on a line joining the tragus of the ear and the angle of the mouth, the subject is then asked to blow his cheeks fully and the distance measured between the two points marked on the cheek V1. CF =V1-V2. Mean value for males- 1.2 cm, females- 1.08 cm.
II. Grade 2 (Moderate OSMF):
a) Moderate to severe blanching
b) Mouth opening reduced by 33%
c) Tongue protrusion reduced by 33%
d) Flexibility also demonstrably decreased, burning sensation even in absence of stimuli
e) Palpable bands felt
f) Lymphadenopathy either unilateral or bilateral.
III. Grade 3 (Severe OSMF):
a) Burning sensation very severe
b) Patient unable to do day to day work
c) More than 66% reduction in the mouth opening
d) Cheek flexibility and tongue protrusion, in many the tongue may appear fixed Ulcerative lesions may appear in cheek
e) Thick palpable bands felt
f) Lymphadenopathy is bilaterally evident.
Etiology
The etiology of the disease is still not well established. It is believed to be multi factorial. Factors include:
a) Betel nut chewing
b) Chilli consumption
c) Genetic factors
d) Auto immunity
e) Deficiency of iron, B complex
f) Folic acid deficiency
a) Areca Nut (Betel Nut) Chewing [8]: Quid is a substance or mixture of substances (in any manufactured or processed form) that is placed in the mouth, where it is sucked or actively chewed and thus remains in contact with the mucosa over an extended period. It usually contains one or both of 2 basic ingredients, tobacco and areca nut. The composition of betel quid, also known as paan, varies between communities and individuals, although the major constituents are areca nut and slaked lime (from limestone or coral) wrapped within a betel leaf. The paan is placed between the teeth and the buccal mucosa, and is gently chewed or sucked over a period of several hours. The slaked lime acts to release an alkaloid from the areca nut, which produces a feeling of euphoria and wellbeing. Other substances of local preference may be added, such as grated coconut or a variety of spices, for example, aniseed, peppermint, cardamom and cloves. Tobacco may also be used as a component of paan, and this ingredient is associated with a significant risk of oral cancer. In addition, the lime has been shown to release reactive oxygen species from extracts of areca nut, which might contribute to the cytogenetic damage involved in oral cancer. Variants of paan include use of sliced areca nut alone and addition of sweeteners to make the product particularly attractive to younger children, to whom it is sold under the names sweet supari, gua, mawa or mistee pan. Other variants such as kiwam, zarda and mitha pan may contain a variety of substances, including tobacco. 3 basic categories:
a. Quid with areca nut but without any tobacco products, which may involve chewing only the areca nut or areca nut quid wrapped in betel leaf (paan).
b. Quid with tobacco products but without areca nut, including chewing tobacco, chewing tobacco plus lime, mishri (burned tobacco applied to the teeth and gums), moist snuff, dry snuff, niswar (a different kind of tobacco snuff ) and naas (a stronger form of niswar).
c. Quid with both areca nut and tobacco products (paan with tobacco).
b) Ingestion of Chillies: The use of chillies (Capsicum annum and Capsicum frutescence) has been thought to play an etiological role in oral submucous fibrosis. Capsaicin, which is vanillylamide of 8-methyl-6-nonenic acid, is the active ingredient of chillies, play an etiological role in oral submucous fibrosis [9].
c) Genetic Susceptibility: A genetic component is assumed to be involved in oral submucous fibrosis because of reported cases of OSMF in non-betel nut chewers. Patients with oral submucous fibrosis have been found to have an increased frequency of Human Leukocyte Antigenhaplotypic pairs A1O/ DR3, B8/DR3 and A10/B8 [9].
d) Nutritional Deficiencies: A subclinical vitamin B complex deficiency has been suspected in cases of OSMF with vesiculations and ulcerations of oral cavity. The deficiency could be precipitated by the effect of defective nutrition due to impaired food intake in advanced cases and may be the effect, rather than the cause of the disease. Iron is essential for overall integrity and health of epithelia of the digestive tract and its importance may lie in its contribution to normal enzymes. Microcytic hypochromic anemia with high serum iron has been reported in sub mucous fibrosis.
e) Pathogenesis [10]: Areca alkaloids
a. Stabilization of collagen structure by tannins
b. Copper in nut and fibrosis.
c. Upregulation of cyclo-oxygenase (Cox-2)
d. Fibrogenic cytokines
e. Genetic polymorphisms predisposing to OSF
f. Inhibition of collagen phagocytosis
g. Stabilization of extracellular matrix
h. Collagen-related genes
i. OSF as an autoimmune disorder
Areca Alkaloids Causing Fibroblast Proliferation and Increased Collagen Synthesis
Alkaloids from areca nut are the most important biologically. Four alkaloids have been conclusively identified in biochemicalstudies, arecoline, arecaidine, guvacine, guvacoline, of which arecoline is the main agent. This suggests that arecaidine is the active metabolite in fibroblast stimulation. This view was further supported by the finding that, addition of slaked lime (Ca (OH)2) to areca nut in pan facilitates hydrolysis ofarecoline to arecaidine making this agent available in the oral environment (Figure 1).
Stabilization of Collagen Structure by Tannins (and Catachins Polyphenols)
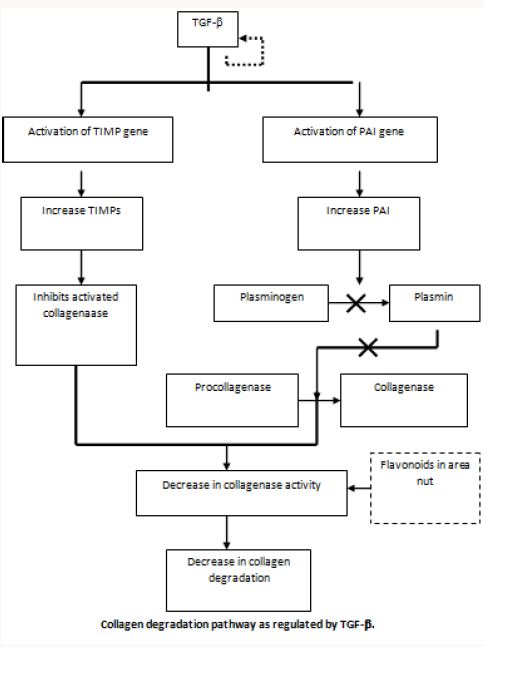
One of the mechanisms that can lead to increased fibrosis is by reduced degradation of collagen by forming a more stable collagen structure. The ability of large quantities of tannin present in areca nut reduced collagen degradation by inhibiting collagenases and proposed the basis for fibrosis as the combined effect of tannin and arecoline by reducing degradation and increased production of collagen respectively.
Copper in Nut and Fibrosis
The copper content of areca nut is high and the levels of soluble copper in saliva may rise in volunteers who chew areca quid. The enzyme lysyl oxidase is found to be upregulated in OSMF. This is a copper dependent enzyme and plays a key role in collagen synthesis and its cross linkage. The possible role of copper as a mediator of fibrosis is supported by the demonstration of up regulation of this enzyme in OSF biopsies.
Upregulation of Cyclo Oxygenase (COX -2)
Prostaglandin is one of the main inflammatory mediators and its production is controlled by various enzymes such as cyclooxygenase (COX). Biopsies from buccal mucosa of OSF cases and from controls were stained for COX-2 by immunohistochemistry and revealed that there was increased expression of the enzyme in moderate fibrosis and this disappeared in advanced fibrosis. This finding is compatible with the histology of the disease as there is lack of inflammation in the advanced disease. COX-2 expression started to decrease when the arecoline concentration was increased upto 160lg/ml, and this may be due to cytotoxicity.
Fibrogenic Cytokines
Areca nut may induce the development of the disease by increased levels of cytokines in the lamina propria. They were able to demonstrate increased levels of pro-inflammatory cytokines and reduced anti-fibrotic IFN- gamma in patients with the disease. These observations may suggest that the disease process in OSF may be an altered version of wound healing as our recent findings show that the expression of various ECM molecules are similar to those seen in maturation of granulation tissue
Genetic Polymorphisms Predisposing to OSF
Polymorphisms of the genes coding for TNF-a has been reported as a significant risk factor for OSMF. The G allele at position +49 of exon 1 was found to be significantly associated with OSF compared with controls.
Inhibition of Collagen Phagocytosis
Degradation of collagen by fibroblast phagocytosis is an important pathway of physiological remodeling of the extracellular matrix (ECM) in connective tissue. As OSF shows a gross imbalance in ECM remodeling. They also showed that the reduction of phagocytic cells was strongly related to the arecoline levels in fibroblast culture.
Stabilization of Extracellular Matrix
Increased and continuous deposition of extracellular matrixmay take place as a result of disruption of the equilibrium between matrix metalloproteinases (MMPs) and tissue inhibitors of matrix metalloproteinases (TIMP). OSF fibroblasts produced more TIMP- 1 protein than normal fibroblasts; Mrna expression of TIMP-1 in OSF firoblasts was also higher. With the above data the authors suggested that TIMP-1 expression is increased at transcriptional level. It was apparent that the expression of tenascin disappeared when the lesion advanced from early to intermediate phase. Heparan sulphate proteoglycans (perlecan), fibronectin, type III collagen and elastin appeared in the early and intermediate phases but there was complete replacement by collagen type I when the lesion progressed to an advanced phase.
Collagen Related Genes
As OSF is a disease with disregulation of collagen metabolism. There is evidence to suggest that collagen-related genes are altered due to ingredients in the quid. The genes CoL1A2, COL3A1, CoL6A1, COL6A3 and COL7A1 have been identified as definite TGF-beta targets and induced in fibroblasts at early stages of the disease. The transcriptional activation of procollagen genes by TGF-beta suggests that it may contribute to increased collagen levels in OSF.
OSF as an Autoimmune Disorder
It was revealed that ANA (23.9%), SMA (23.9%) and GPCA (14.7%) were positive in OSF patients compared with healthy control subjects. Increased levels of immune complexes and raised serum levels of IgG, IgA and IgM when compared with control groups have also been reported. A recent study has revealed higher haplotype frequencies in pairs HLA B51/Cw7 and B62/Cw7 in OSF patients. Two new HLA DRB1 alleles were identified by sequencingbased typing and named as HLA DRB1-0903 and DRB1-1145.
Clinical Features
Most frequently affected locations are the buccal mucosa and the retromolar areas. It also commonly involves the soft palate, palatal fauces, uvula tongue and labial mucosa. Common age of occurrence varies from 12-62 years with the mean age being 40 years but there are reports of OSMF even in as younger as 4 year old. Female predilection with the ratio of 3:2
I. Symptoms
a) Burning sensation aggravated by spicy food.
b) Vesiculation , Ulceration and Pigmentation changes
c) Excessive salivation or Dryness of mouth
d) Recurrent stomatitis
e) Defective gustatory sensation
f) Gradual stiffening of the oral mucosa leads to inability to open mouth and difficulty in swallowing food.
g) Referred pain in ears, deafness and nasal voice observed.
II. Signs
a) Blanching ie- marble like appearance of oral mucosa
b) Types:
i. Localized blanching
ii. Diffuse blanching
iii. Reticular blanching
c) Presence of palpable fibrous bands
d) Affected tongue is devoid of papillae and in extreme cases it is stiff and protrusion of tongue is impaired.
e) Affected soft palate leads restricted movements with BUD-SHAPE uvula in extreme cases.
f) Gingiva is fibrotic, depigmented and devoid of normal stippling.
Investigations [1]
a. Blood chemistry
b. Raised ESR, Anemia, eosinophilia
c. Increased gamma-globulin
d. Decreased serum iron, increased total iron binding capacity
e. Decreased albumin,
f. Alteration in serum copper and zinc ratio.
g. Depression of lactate dehydrogenase isoenzyme ratio at tissue level.
h. AgNOR study shown count is higher in advanced OSF than in moderately advanced case
i. Cell kinetic studies:
j. Effect of areca nut on cells results in excess accumulation of collagen later results in permanent change in fibroblast population, characterized by continued abnormal accumulation of collagen.
Medical Management [1]
The essential elements of treatment of tobacco dependence include:
a. Assessing, and where necessary increasing, motivation to stop.
b. Assessing nicotine dependence.
c. Provision of counselling / behavioural support.
d. Encouraging the use of appropriate pharmacotherapies (nicotine replacement therapy (NRT) or bupropion) to reduce the severity of the withdrawal symptoms.
Various strategies have been proposed for medical management of OSMF:
a. Patient counselling
b. Nutritional Support
c. Immunomodulatory drugs
d. Physiotherapy
e. Local drug delivery
e. Local drug delivery
Patient Education
a. Instruct patients regarding the importance discontinuing the habit of chewing betel quid.
b. Inform patients that eliminating tobacco from the quid product may reduce the risk of oral cancer.
c. Instruct patients to avoid spicy foodstuffs.
d. Instruct patients to eat a complete and healthy diet to avoid malnutrition.
e. Instruct patients regarding maintaining proper oralhygiene and scheduling regular oral examinations.
“Prevention is better than cure”, cessation of BQ chewing habit is very important for any of the treatment modalities.
Placental Extracts [1]
a. The rationale for using placental extract (PE) in patients with OSF derives from its proposed anti-inflammatory effect hence, preventing or inhibiting mucosal damage.
b. Cessation of areca nut chewing & submucosal administration of aqueous extract of healthy human PE (Placentrex) showed marked improvement of the condition.
Levamisole
Dose 150 mg O.D. for 3 days-twice in a month for 3 month (Vermisol, Levazole). Pentoxifylline Therapy: A New Adjunct in Treatment of osmf: Pentoxifylline is a drug of methylxanthine derivative that has vasodilating properties and was helps to increase mucosal vascularity. Rajendran R (2006) conducted a pilot study of Pentoxifylline therapy (Trental) 400 mg 3 times daily for 7 months for the treatment of OSMF patients. Side effects involve Gastrointestinal and Central nervous system.
Corticosteroids [1]
Local-Hydrocortisone injection along with procaine hydrochloride injection locally in the area of fibrosis. Injections are given fortnightly. The early cases shows good improvement with this therapy. Systemic-A therapy with hydrocortisone 25mg tablet, in doses of 100mg/day is useful in relieving burning sensation without on toward effects. Triamcinolone or 90mg of dexamethasone can be given. This is supplemented with local injection of hydrocortisone 25mg at biweekly intervals at the affected sites. Increased vascularity of the site is observed, which is attributed to fibrinolytic, anti-allergic and anti-inflammatory action of corticosteroid. Decreases inflammation by suppressing migration of polymorphonuclear leukocytes and reducing capillary permeability. Fibrosis is prevented by decreasing fibroblastic production and deposition of collagen.
Hyaluronidase
The use of topical hyaluronidase has been shown to have quicker improvement in symptoms compared with steroids alone. Hyaluronidase, by breaking down hyaluronic acid lowers the viscosity of intracellular cement substance i.e., hyaluronidase decreases cell formation by virtue of this action on hyaluronic acid, which plays an important role in collagen formation. The combination of steroids and topical hyaluronidase shows better long term results than either agent used alone. Dose150 U added to vehicle solution.
IFN-Gamma
Immunoregulatory effect. IFN-gamma is a known antifibrotic cytokine. IFN-gamma, through its effect of altering collagensynthesis, appears to be a key factor to the treatment of patients with OSF, and intralesional injections of thecytokine may have a significant therapeutic effect on OSF.
Lycopene
It is an antioxidant from tomato extract, along with other previously used antioxidants in the treatment of OSMF. Dose tab lycopene 2000mcg.The drug will be given for a period of 3 months duration during which time patient will be reexamined every 15 days.
Turmeric
Alcoholic extracts of turmeric - turmeric oil and turmeric oleoresin, patient with submucous fibrosis were given a total oral dose of Turmeric oil (600 mg TO mixed with 3 g TE/day) Turmeric oleoresin (600 mg + 3 g TE/day) & 3g Turmeric/day as a control for 3months. It was observed that all three treatment modalities decreased the number of micro nucleated cells both in exfoliated oral mucosal cells and in circulating lymphocytes.
Physiotherapy
a. Hot rinses, lukewarm water
b. Muscle stretching exercises
c. Selective deep heating therapies like short wave and microwave diathermy.
References
- Ongole R, Parveen BN (2013) Textbook of Oral Medicine Oral Diagnosis and Oral Radiology. Red and white lesions, (2nd edn), Elsevier, Chennai, India, pp. 133-173.
- Kumar A, Bagewadi A, Keluskar V, Singh M (2007) Efficacy of lycopene in the management of OSMF. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 103(2): 207-213.
- Pindborg JJ, Sirsat SM (1966) Oral submucous fibrosis. Oral Surg Oral Med Oral Pathol 22(6): 764-779.
- Rajendra R (1994) OSMF: etiology, pathogenesis, and future research. Bull World Health Org 72(6): 985-996.
- Paymaster JC (1956) Cancer of the buccal mucosa. A clinical study of 650 patients. Cancer 9(3): 431-435.
- Rajendra R (2003) Oral submucous fibrosis. J Oral Maxillofacial Pathology 7(1): 1-4.
- Bailoor DN, Nagesh KS (2005) Fundamentals of Oral medicine and radiology (1st edn.), Jay pee brothers, New Delhi, India, pp. 446.
- Gupta PC, Warnakulsuriya S (2002) Global epidemiology of areca nut use. Addict Biol 7(1): 77-83.
- Vedtofte P, Holmstrup P, Hjorting Hansen E, Pindborg JJ (1987) Surgical treatment of premalignant lesions of the oral mucosa. Int J Oral Maxillofac Surg 16(6): 656-664.
- Rajalalitha P, Vali S (2005) Molecular pathogenesis of oral submucous fibrosis a collagen metabolic disorder. J Oral Pathol Med 34(6): 321-328.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...

.png)