Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6679
Review Article(ISSN: 2637-6679) 
Inguinal Hernias Repair by Laparascopy (Pet) Volume 6 - Issue 4
Olga Caridad León González1, Pedro Rolando López Rodríguez2*, Lais Angélica Ceruto Ortiz3, Jorge Agustín Satorre Rocha4, Eduardo García Castillo5,Luis Marrero Quiala6
- 1Assistant Professor and Assistant Researcher I Degree Specialist in General Surgery.
- 2Consulting Professor Assistant Professor and Assistant Researcher II Degree Specialist in General Surgery.
- 3Instructor teacher Resident of 3rd Year in General Surgery.
- 4Assistant Professor First Degree Specialist in General Surgery.
- 5Assistant teacher First Degree Specialist in General Surgery.
- 6Assistant Professor First Degree Specialist in General Surgery.
Received: November 13, 2021 Published: November 30, 2021
Corresponding author: Pedro Rolando López Rodríguez National Hospital. Calle Continental No. 152 between Calle D´Strampes and Calle Goicuría. Sevillano. October 10, Havana. Cuba.
DOI: 10.32474/RRHOAJ.2021.07.000254
Abstract
Introduction: The hernia affection is one of the processes that has been studied into much detail and whose treatment pursues
excellence, although many controversies are still yet to be resolved. Laparoscopy repair of inguinal hernia is a treatment method
that improves the quality of management given to our patients.
Objective: To identify perioperative events, surgical complications and to evaluate the pain referred for the patients who have
had inguinal hernia repair by the laparoscopic method. (TEP).
Methods: A prospective and descriptive study was done on 80 patients who have had endoscopic (TEP) repair of inguinal
hernias between January 2013 and December 2020.
Results: We performed 100 hernioplastias by laparocoscopy in 80 patients. The male sex predominated in a 5:1 ratio and
the surgical time average was, 53.5 minutes for unilateral hernias and 71.3 minutes for the bilateral ones. The most frequent
complication in the transoperatory stage was ¨minor bleeding¨. At 15 days after surgery, 86.3% of the operated did not complain
of pain, but social and laboral reintegration was at a 34% of the total.
Conclusions: Laparoscopic inguinal hernioplasty is a good therapeutic option, mainly in patients with bilateral and reproduced
inguinal hernias.
Keywords: Laparoscopic Hernioplasty; Inguinal Hernia; Hernia Recurrence
Introduction
Since the concept of endoscopic inguinal hernia repair was first described by Ger in 1982, endoscopic techniques have been modified; It was a time when failures and complications - coupled with high cost - outweighed initial enthusiasm [1]. Laparoscopic hernioplasty (LH) has gained popularity in the last decade and numerous controlled studies appear in the literature comparing laparoscopic techniques with conventional ones [2]. In recent years, HL, despite being one of the most controversial laparoscopic procedures, has established itself as a therapeutic option to consider. The advantages of this method are demonstrated in bilateral, recurrent hernias and in the labor-active subject, who requires early return to work [3].
Method
Between January 2013 and December 2020, a prospective, descriptive, longitudinal-cut study was carried out in 80 patients operated on by endoscopy (PET) with the diagnosis of inguinal hernia, at the General Teaching Hospital “Enrique Cabrera”. All patients who agreed with the type of surgical intervention, the study and who gave their informed consent were included; patients older than 30 years classified ASA I-III, without anesthetic contraindications for laparoscopic intervention and patients classified as Nyhus III and IV. Patients with previous surgical wounds in the inguinal region, to operate, not dependent on reproduced inguinal hernias and patients with complicated, irreducible or slipped inguinal hernias; they were excluded. The surgical techniques were: totally extraperitoneal laparoscopic inguinal hernioplasty (TEP). The PET technique was performed with some variants such as: no use of the balloon trocar, the preperitoneal space was decolorized by means of the 0º laparoscope and the insufflation of CO2 at 13 mmHg. In patients with large hernial rings, a polypropylene cone was placed in the hernial defect and subsequently a 15 x 12 cm polypropylene prosthesis. There was no need to fasten the meshes with clips [4]. In the immediate postoperative period, the visual pain scale analog scale (VAS) was applied and a pain value was assigned by means of “little faces”, which starts from very happy (I value) to very sad (X value). Pain quantification was repeated in consultation 7 days, 15 days and one month after the operation.
Results
100 hernias were operated on in 80 patients (20 patients [25%]
had bilateral hernias, 85 primary hernias, and 15 reproduced
hernias). The average age was 55.6 years, the youngest patient
was 30 years old and the oldest was 77 years old, but the majority
(14 patients) belonged to the fifth decade of life. The male sex
predominated in 84%, which represented a male / female ratio of 5:
1. 43% of the patients made great physical efforts on a regular basis
Table 1 shows that 36 patients had the habit of smoking, which
represents 45% of the total and 17 consumed alcohol for 21.2%.
Table 2 shows that right hernias were more frequent in 54.0%
of the total; the indirect variety with great dilation of the annulus
and destruction of the posterior wall (IIIb) was the most frequent
(41 hernias). Nine femoral hernias and 15 recurrent hernias were
operated on.The 100 surgeries were performed by PET technique
(100.0%). Two of the patients in whom a PET technique was started
had to be converted to a conventional prosthetic technique due to
accidental perforation of the peritoneum, passing CO2 into the
peritoneal cavity, and consequently, the loss of the preperitoneal
surgical space, and another was the conversion of a failed PET
technique. The mean surgical time for unilateral hernias was 53.5
min, with a minimum time of 25 min and a maximum of 120 min.
In bilateral repairs, the average surgical time was 71.3 min, with a
minimum of 40 min and a maximum of 110 minutes. The hospital
stay was less than 24 hours in 70 patients (87.5%), in 5 patients it
extended from 24 to 48 hours and in 5 patients it lasted more than
48 hours.
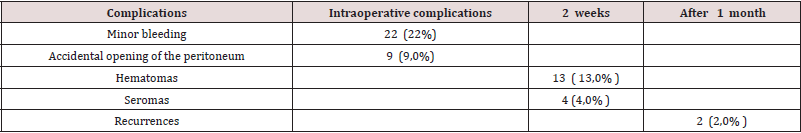
Table 3 shows minor bleeding as the most frequent complication
in the intraoperative period, in 22 repairs (22.0%) that originated
13 hematomas (13.0%). No complications were observed after
the second week, but two patients suffered recurrences (2.0%)
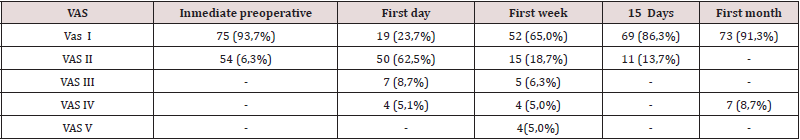
more than two months after the operation. Table 4 shows the
pain classification according to the VAS scale. In the immediate
postoperative period, after the patient recovered from anesthesia,
75 individuals (93.7%) were classified as VAS I and 5 patients
as VAS II. At 24 h after the operation, 19 patients (23.7%) were
classified as VAS I, 50 (62.5%) as VAS II, 7 patients as VAS III, and 4
as VAS IV. In the first week postoperative consultation, 52 patients
(65.0%) were classified as VAS I and 15 as VAS II, and two patients
with moderate pain (VAS V) appeared in this period. At 15 days
after surgery, 69 patients (86.3%) were VAS I and at one month 73
(91.3%) were. The incorporation to the usual activities, including
work, was of 3 patients (3.7%) a week after the operation, after 15
days there were 23 patients (28.7%) and at month 54 patients, for
67, 5% of the total.
Table 1: Toxic habits and personal pathological history (APP).
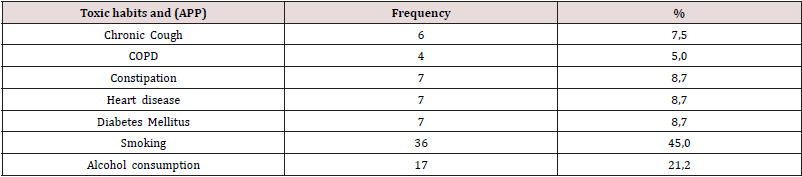
N= 80 COPD: Chronic obstructive pulmonary disease
Table 2: Distributión according classificatión to the Nyhus [5].
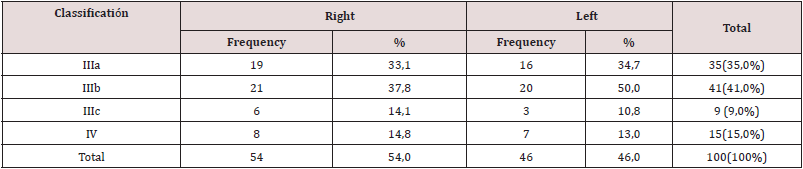
Thel total is 100 hernias operated on in 80 patients.
Discussion
Currently, with the improvement of laparoscopic techniques,
inguinal hernia surgery is emerging as safe, feasible and as a good
therapeutic option, regardless of the age of the patient; However,
the preoperative evaluation of the individual must be correct and
thorough, specifically the cardiorespiratory function, since with
the TEP method a working space is created between the sheets of
the transverse lamina, richly vascularized, so that the absorption
and elimination of the CO2 is greater than that produced in the
peritoneal cavity during pneumoperitoneum [7]. Although men
predominated, there was a slight increase in women in the series
with respect to other authors [8] In laparoscopic practice, the
finding of hernial defects diagnosed during the intraoperative
period is frequent, in men and women, the latter essentially with a
history gynecological disorders. Although the usefulness of hernia
repairs in asymptomatic patients is questioned in some articles,
the authors consider that it would be beneficial for the patient,
if conditions permit, to repair the hernial defect by the TAPP
method [9]. The relationship between hernial disease and physical
exertion has been classic since Cooper’s time. In the series, 68% of
the patients performed physical activities that involved great and
medium efforts and also analyzing the multifactorial nature in the
pathogenesis of hernia disease, it is striking that approximately
half of the operated patients were smokers, a factor that influences
in collagen metabolism, significantly linked to hernia recurrences
[10]. Most of the repairs were by means of the TEP technique and
we consider, like other authors, that although the TAPP technique
brings us closer to the area from a perspective familiar to the
surgeon (peritoneal cavity) and facilitates the so-called “learning
curve”; Hernia disease -because it is considered a parietal defectshould
be given a solution from this same plane, to avoid the
probability of serious complications of the intra-abdominal organs
and to leave the transperitoneal method as a tactical resource when
the totally extraperitoneal method is unsuccessful. (eleven)
Average surgical time was similar to other series [12]. It is
known that this tends to decrease when the surgical team gains in
experience. The longest operating time recorded was in a patient,
who started with a PET technique, but due to technical difficulties,
he was converted to a conventional posterior repair.
The main complications were related to minor intraoperative
bleeding and postoperative hematomas. In 3 patients it was
necessary to drain the hematoma due to the discomfort caused,
however, in the rest of the patients with hematomas and seromas
they were treated with conservative measures. In two patients,
recurrence occurred 2 months after the operation, which was
interpreted as a technical error [13,14]. Our results coincide with
numerous studies that affirm less postoperative pain with the use of
minimal access techniques, as well as a prompt socio-occupational
reincorporation of patients [1,3,9,15]. Despite the fact that 70%
and 93.3% of the patients at 1 week and 15 days after surgery,
respectively, had no pain or minimal discomfort; only 18 individuals
(30%) started their usual activities before 15 days. These results
contrast with other studies that report a return to work and social
activities between 10-15 days postoperatively, although it is likely
that some sociocultural factors are influencing these results [1,16].
In the series there were no major intraoperative or postoperative
complications, only minor bleeding and bruising. In most of the
patients, before 2 weeks postoperatively, the pain disappeared,
however, the return to social work activities after 15 days was low.
Conclusions
Laparoscopic inguinal hernioplasty was an effective therapeutic option, especially for patients with bilateral and reproduced hernias. It provided benefits to patients and families, the former joining work and social activities early.
References
- Ruiz Funes MAP, Farell RJ, Marmolejo CA, Sosa LAJ, Cruz ZA (2020) Approach to infrequent hernias by minimal access surgery: case series. Rev Mex Cir Endoscop 21 (1): 6-14.
- Magnus H, Anders B, Westerdahl J (2008) Laparoscopic extraperitoneal inguinal hernia repair versus open mesh repair: long-term follow-up of a randomized controlled trial. Surgery 143(3): 313-317.
- Bittner R, Bain K, Bansal VK, Berrevoet F, Bingener Casey J, Chen D et al. (2019) Update of Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endo hernia Society (IEHS))-Part A. Surg Endosc 33: 3069-3139.
- Cruz Alonso JR (2007) (Endohernioplasty. Technical details. Arch Cir Gen Dig [series on the Internet].
- Carbonell Tatay F (2001) Hernia inguinocrural. Valencia: Ethicon pp.141-142.
- DeLoach LJ, Higgins MS, Caplan AB, Stiff JL (1998) The Visual Analog Scale in the immediate postoperative period: intrasubject variability and correlation with a numeric scale. Anesth 86: 102-106.
- Halligan S, Parker SG, Plumb AA, Windsor AC (2018) Imaging complex ventral hernias, their surgical repair, and their complications. Eur radiol 28: 3560-3569.
- Henriksen NA, Kaufmann R, Simons MP et al. (2020) EHS and AHS guidelines for treatment of primary ventral hernias in rare locations or special circumstances. BJS Open 4: 342-353.
- León González OC, López Rodríguez PR, Danta Fundora LM, Satorre Rocha JA, García Castillo E, Ceruto Ortiz LA (2019) Inguinal Hernia Repair by Laparascopy. Surg Cas Stud op Acc J Vol3 (2).
- Bórquez MP, Garrido OL, Manterola DC, Peña P, Schlageter C, Orellana J, et al. (2003) Study of collagen and elastic fibers of the connective tissue of patients with and without primary inguinal hernia. Rev Méd Chile 131 (11): 1273-1279.
- Díaz Martínez J, Ramírez Colin G (2019) Extraperitoneal total endoscopic inguinal hernioplasty (TEP). Experience of our first 100 cases in the second level hospital. Cir Endoscop 18 (2): 125-134.
- Martin Gómez M (2018) Laparoscopic Surgery of the inguinal hernia. TEP. Cir Andal 29 (2): 174-177:
- Palmisano EM, Martínez JD, García MM, González JD (2018) Key maneuvers and tricks in TEP. Rev Hispanoamerican Hernia 6(2): 86-90.
- Hernia Surge Group (2018) International guidelines for groin hernia management. Hernia 22: 1-165.
- Liu J, Zhu Y, Shen Y, Liu S, Wang M, Zhao X et al. (2017) The feasibility of laparoscopic management of incarcerated obturator hernia. Surg Endosc 31: 656-660.
- Morera Pérez M, Roque González R, González León T, Sánchez Piñero RO, Olivé González JB (2019) Abdominal Surgery in the elderly. Rev Cubana Cir 58 (1).

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...

.png)