
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6679
Research Article(ISSN: 2637-6679) 
Influence of COVID-19 pandemic on the prevalence of Helicobacter Pylori infection in Westside Community of Chicago Volume 8 - Issue 5
William Xu1, Ejazul Haque2,3, Haoliang Xu*2,3, Marianne Greene2, Shanching Ying2, Russell Fiorella2
- 1Walter Payton College Preparation High School, Chicago, USA
- 2Mount Sinai Hospital, Sinai-Healthcare System, Chicago, USA
- 3Ross University, School of Medicine, Miramar, USA
Received: October 16, 2023; Published: October 27, 2023
Corresponding author: Haoliang Xu, Mount Sinai Hospital, Sinai-Healthcare System, Chicago, Ross University, School of Medicine, Miramar, Florida, USA
DOI: 10.32474/RRHOAJ.2023.08.000296
Abstract
This study was designed to evaluate the impact of the COVID-19 pandemic on the prevalence of Helicobacter pylori - associated gastritis. Retrospective analysis was performed on all gastric biopsy cases collected at the Sinai Health System - Chicago during both pre-pandemic (12/2017 – 11/2019) and pandemic (12/2020 – 11/2022) periods. Helicobacter pylori prevalence markedly decreased during the pandemic period (30.8% pre-pandemic vs 20.7% pandemic) across all age groups, particularly in the youngeraged and middle-aged groups. There was no significant gender-related predilection detected. The significant decline in Helicobacter pylori infection may be related to COVID-19 pandemic-related lifestyle alterations.
Keywords: Helicobacter pylori; gastritis; peptic and duodenal ulceration; gastric cancer; lymphoma
Introduction
The United States Department of Health and Human Services (HHS) declared the severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2) outbreak a public health emergency in the United States on Jan 31, 2020. SARS-CoV-2, which causes coronavirus disease 2019 (COVID-19), is spread primarily through airborne particles and droplets [1]. Since the beginning of this outbreak, over 1 million COVID-19-related deaths have been confirmed. This outbreak demonstrated a high mortality rate and expanded globally, becoming one of the deadliest pandemics in human history. Several steps were taken by the Centers for Disease Control and Prevention (CDC) to prevent the rapid growth of this airborne infectious disease in the US, including mask mandates, social distancing, and routine testing.
These policies created a dramatical lifestyle change for many during this pandemic. Demand for better hygiene increased, and many individuals participated in social distancing, minimized travelling, avoided social gathering and dining, and worked remotely. Helicobacter Pylori (H. pylori) is a gram-negative, spiralshaped bacterium that lives naturally in the mouth and stomach. Fifty percent of the population worldwide and 30-40% of population in the United States is infected with H. pylori in their lifetime, with an especially high prevalence rate in lower socioeconomic regions [2]. Most of these individuals have no clinical symptoms and are asymptomatic carriers of the bacteria. However, the bacteria can break down gastric mucosa lining and cause acute and/or chronic inflammation. The complications of the infection can be persistent gastritis, peptic and duodenal ulceration, gastric cancer, and lymphoma [3,4].
H. pylori can spread through contact between individuals, consumption of contaminated food, and ingestion of water from an unreliable source [5,6]. Living in a crowded area with frequent social contact is considered as a high-risk factor of infection. In the current study, we expected that the dramatic personal lifestyle alterations (i.e., decreased social activity and increased demand of personal hygiene) during the COVID-19 pandemic would have strongly impacted the routes of H. pylori transmission, which would subsequently suppress the bacteria’s prevalence/incidence in the community.
Methods
Study Design and Case Collection
We conducted a retrospective analysis of all gastric biopsies performed in the Sinai Healthcare System – Chicago, during the prepandemic (Dec 2017 - Nov 2019) and pandemic (Dec 2020 - Nov 2022) periods. This study was reviewed and approved by Mount Sinai Hospital Institutional Review Board (IRB #: MSH-IRB-22-44). Cases from patients subjected to the endoscopic examination and gastric biopsy were retrieved through the MEDITECH information system at Mount Sinai Hospital. Patients of both genders (male and female) and all ages (19-89 years old) were included. Cases with suboptimal tissue sampling for histological evaluation or equivocal diagnosis in H. pylori infection (after immunohistochemical stain) were excluded from this study. Monthly case volumes and H. pyloripositivity rates were recorded.
Data Analysis
The influence of the pandemic on the H. pylori infection rate was calculated by comparing pre-pandemic months to their matched pandemic months using a student’s t-test. The statistical significance for the t-test was set at a two-sided p < 0.05. The patients were further divided into two subgroups, male and female, to assess the possible gender predilection in H. pylori infection during pre-pandemic and pandemic periods. The influence of the pandemic on different age groups were also addressed by dividing cases into three subgroups: the youth group (<30 years old), middleaged group (30-60 years old), and elderly group (>60 years old). The overall infection rate of H. pylori in each subgroup during the pandemic was calculated and expressed as (positive case number / total case number) x 100%.
Results
Figure 1: Influence of COVID-19 pandemic on H. Pylori prevalence. A) During pandemic, the monthly H. Pylori-positive rate was significantly decreased (20.7 ± 4.7 %, pandemic vs 30.8 ± 7.2 %, pre-pandemic; mean ±SE, *P<0.01). B) H. Pylori-infection showed no apparent gender predilection in both pre-pandemic and pandemic periods. C) Pandemic-associated declines of H. Pylori infection were seen across all age groups.
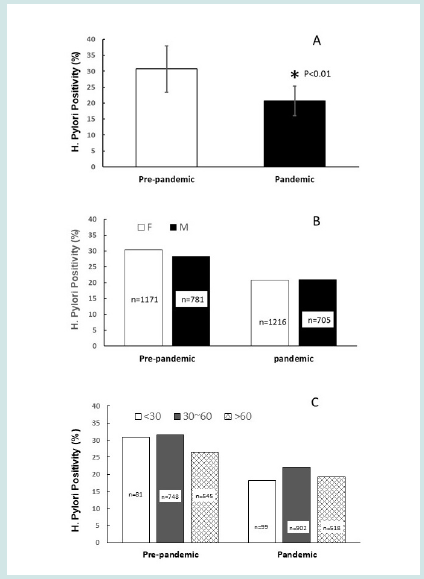
Figure 2: Monthly H. Pylori infection rates in the observed two-year periods of per-pandemic and pandemic, respectively.
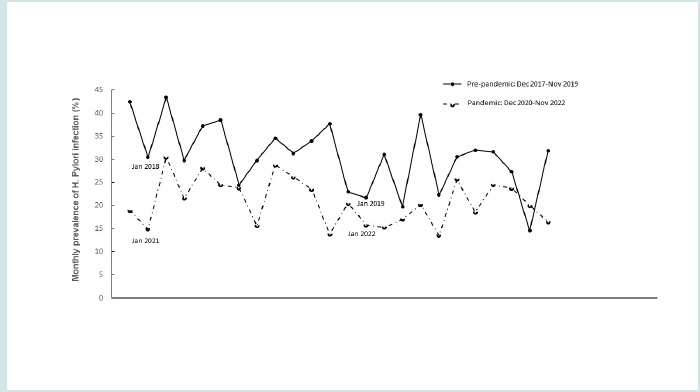
During the observed two-year pre-pandemic period, 1,952 patients received gastric biopsies at Mount Sinai Hospital. Monthly biopsy numbers ranged from 53 to 158, and the monthly positivity rate was between 14.5% to 43.4%. Within the same length of time, the procedure volume during the pandemic essentially remained unchanged, totaling to 1,920 cases, and the monthly biopsy numbers ranged from 19 and 126 cases. The monthly positivity rates during the pandemic period ranged from 13.5% to 28.7%. Compared with the pre-pandemic period, a sharp and statistically significant decrease in H. pylori positivity rate was noted (20.7±4.7% vs 30.8±7.2%, pandemic vs pre-pandemic; p < 0.01) (Figure 1A). The positivity rates of each month in both pre-pandemic and pandemic periods are shown in the scatter plot, in which a declining trend was clearly demonstrated (Figure 2). It was noted that compared to the male patients, 50% more female patients received endoscopic examination/biopsy procedures during the pre-pandemic period (female vs male: 1171 vs 781). This number increased to 72.4% during pandemic period (female vs male: 1216 vs 705).
However, there was no gender predilection detected in the H. pylori infection at both pre-pandemic and pandemic periods (Female vs male: 30.4 % vs 28.4 %, pre-pandemic; 20.8 % vs 21.1 %, pandemic; Figure 1B). In the current study, the youngest age of patients was 19 years old. Therefore, no cases from children were included in this project. In addition to gender, the patients were divided into three age groups:
a) youth, <30 years old (n=117 pre-pandemic, n=121 pandemic)
b) middle age, 30-60 years old (n=1093 pre-pandemic, n=1158 pandemic)
c) elderly: >60 years old (n=741 pre-pandemic, n=642 pandemic).
The results revealed that during the pre-pandemic period, the middle-age group showed the highest infection rate (31.6%), followed by the youth group (30.8%). The elderly group had the lowest infection rate overall (26.5%). Although the pandemic markedly decreased infection rates across all age groups, the biggest impact was detected in the youth group (30.8% pre-pandemic vs 18.2% pandemic) (Figure 1C).
Discussion
The COVID-19 pandemic has had a profound and a far-reaching impact on social and economic infrastructures and has led to tremendous disruptions in the healthcare system. The drastic changes in people’s lifestyles during the pandemic have been linked with alterations in risk and prognoses in many infectious diseases. In this study, we are the first to report that the COVID-19 pandemic is associated with a significant decrease in H. pylori prevalence across all age groups. It has impacted the youth group the most, with much less influence on the elderly group. Although female patients are more prone to report abdominal discomfort and receive endoscopic procedures, there were no gender predilections observed in H. pylori infection in both pre-pandemic and pandemic periods. H. pylori infection has been linked to various respiratory diseases in previous studies, including chronic bronchitis and pulmonary tuberculosis [7,8].
More interestingly, studies suggest that H. Pylori infection may facilitate / potentiate SARS-CoV-2 virus transmission by increased expression of the angiotensin converting enzyme-2 (ACE-2) receptors in the gastrointestinal tract [9,10]. Therefore, H. Pylori infection in patients with COVID-19 has been recently addressed in multiple studies. Nikpour S, et al. detected an extremely high prevalence of H. pylori in a COVID-19 positive population (71.2 % H. pylori positive rate) [11]. Because of the high prevalence, a concurrent surge of H. pylori infection during the pandemic would be expected, considering the extremely contagious nature of SARSCoV- 2. However, it should be noted that other studies conducted by Balamtekin N, et al. and Genc A, et al. found no significant increase of H. pylori co-infection [12,13]. All these studies are composed of small research samples, and large sized, multi-center cohort studies are needed to elucidate the possible relationship between H. pylori positivity and SARS-CoV-2 infection.
Nevertheless, our study mainly focused on the alteration of H. pylori prevalence during COVID-19 pandemic period, with no intention of exploring the underlying pathogenic relationship or crosstalk between these two pathogens. We considered that the various hygiene mandates/recommendations during the pandemic established a perfect epidemiological model to evaluate the preventive measures in community infectious diseases, including H. pylori. As we expected, the occurrence of the COVID-19 pandemic led to a significant decrease in the prevalence of H. pylori infection. Although the underlying cause is uncertain, personal lifestyle changes must be considered as a potential contributor because health professionals believe that direct contact with infected patients, drinking unreliable water, and eating contaminated foods are the main risk factors of disease spreading.
During the pandemic, governments enforced social distancing policies, stressing the importance of personal hygiene, which consequently forced many public gathering spaces to close. All these steps can potentially interrupt the spreading pathways of H. pylori, and theoretically decrease the opportunity of infection. Compared to the elderly, young and middle-aged adults are more likely to be socially active, which may explain higher H. pylori infection rates detected within these two age groups. During pandemic, the largest decrease in H. pylori prevalence was seen in the youth group, further supporting our hypothesis. There are several limitations in this study. First, a total of 3855 gastric biopsy cases were collected from the pre-pandemic period (2017-2019;1952 cases) and the pandemic period (2020-2022;1903 cases). Although a large sample size was achieved, the statistical power in some subgroups could be improved (i.e., the youth groups had case numbers of 117 for the pre- pandemic and 121 for the pandemic).
Second, this study was performed within the population located within the west urban area of Chicago. Therefore, this finding is limited and may not represent other urban areas or adjacent suburbs with different socioeconomic settings. Multi-center cohort studies may be necessary to resolve these limitations. Third, during the pandemic period, COVID-19 screening was mandated and applied to all patients of elective procedures. Only patients who tested negative for COVID-19 were admitted for this procedure. This process may have led to a selective bias in our final analysis. Additionally, due to the same reason, a direct correlation between COVID-19 infection and H. pylori positivity cannot be captured. Lastly, there are some other risk factors of H. pylori infection, such as alcohol use and diabetes [14,15], which are most likely impacted by lifestyle changes, and became the confounding factors of this study.
Conclusion
The H. pylori prevalence rate significantly decreased during COVID-19 pandemic and may be associated with decreased social activity and increased personal hygiene demand.
Author Contributions
William Xu: Involved in study design, data collection and analysis, and manuscript preparation.
Ejazul Haque: Involved in data analysis and manuscript preparation.
Marianne Greene: Involved in manuscript preparation and result discussion.
Shanqing Ying: Involved in study design and manuscript preparation.
Russell Fiorella: Involved in manuscript preparation and result discussion.
Haoliang Xu: Involved in study design, data analysis, and manuscript preparation.
Acknowledgement
We would like to acknowledge the Department of Pathology and the Research Administration Committee, Sinai Healthcare System, for their support in carrying out this study.
Conflicts of Interest
All authors declare that the research was conducted in the absence of any commercial and financial relationships that could be considered with potential conflict of interest.
Funding
The study was not supported by research funding and was not involved with any other significant financial support.
References
- Meyerowitz EA, Richterman A (2022) SARS-CoV-2 Transmission and Prevention in the Era of the Delta Variant. Infect Dis Clin North Am 36(2): 267-293.
- Salih BA (2009) Helicobacter pylori infection in developing countries: the burden for how long? Saudi J Gastroenterol 15(3): 201-207.
- McColl KE, el-Omar E, Gillen D (2000) Helicobacter pylori gastritis and gastric physiology. Gastroenterol Clin North Am 29(3): 687-703.
- Parsonnet J, Hansen S, Rodriguez L, Gelb AB, Warnke RA, et al. (1994) Helicobacter pylori infection and gastric lymphoma. N Engl J Med 330(18): 1267-1271.
- Goh KL, Chan WK, Shiota S, Yamaoka Y (2011) Epidemiology of Helicobacter pylori infection and public health implications. Helicobacter 1(01): 1-9.
- Kotilea K, Bontems P, Touati E (2019) Epidemiology, Diagnosis and Risk Factors of Helicobacter pylori Adv Exp Med Biol 1149: 17-33.
- Kanbay M, Gur G, Akcay S, Yilmaz U (2005) Helicobacter pylori seroprevalence in patients with chronic bronchitis. Respir Med 99(10): 1213-1216.
- Perri F, Clemente R, Festa V, Ambrosio C, Quitadamo M, et al. (1999) Serum tumour necrosis factor-alpha is increased in patients with Helicobacter pylori infection and CagA antibodies. Ital J Gastroenterol Hepatol 31(4): 290-294.
- Sugimoto M, Yamaoka Y, Shirai N, Furuta T (2012) Role of renin-angiotensin system in gastric oncogenesis. J Gastroenterol Hepatol 27(3): 442-451.
- D'Amico F, Baumgart DC, Danese S, Peyrin-Biroulet (2020) Diarrhea During COVID-19 Infection: Pathogenesis, Epidemiology, Prevention, and Management. Clin Gastroenterol Hepatol 18(8): 1663-1672.
- Nikpour S, Gachkar L, Rezaei R, Salehi M, Futuhi F, et al. (2022) Prevalence of Helicobacter pylori infection and its associated factors in patients with COVID-19. Novelty in Biomedicine 10(3): 167-177.
- Balamtekin N, Artuk C, Arslan M, Gülşen M (2021) The Effect of Helicobacter pylori on the Presentation and Clinical Course of Coronavirus Disease 2019 Infection. J Pediatr Gastroenterol Nutr 72(4): 511-513.
- Genc AB, Yaylaci S, Dheir H, Şenocak D, Şahin E, et al. (2021) The prevalence of Helicobacter pylori and its effect on prognosis of patients with COVID-19. Medical Science and Discovery 8(4): 208-212.
- Kouitcheu Mabeku LB, Noundjeu Ngamga ML, Leundji H (2020) Helicobacter pyloriinfection, a risk factor for Type 2 diabetes mellitus: a hospital-based cross-sectional study among dyspeptic patients in Douala-Cameroon. Sci Rep 10(1): 12141.
- Brenner H, Berg G, Lappus N, Kliebsch U, Bode G, et al. (1999) Alcohol consumption and Helicobacter pylori infection: results from the German National Health and Nutrition Survey. Epidemiology 10(3): 214-218.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...

.png)


