Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6679
Research Article(ISSN: 2637-6679) 
Evaluation of Pregabaline Efficiency in Reducing Opioid Use and Pain in Post-Operating Patients Subject to Total Knee Arthroplasty Surgery Volume 4 - Issue 5
Rogério Nascimento Costa1*, Laércio Pol Fachin2, Caio da Silva Ramos Leal3, Daniel Menezes Tenório Cavalcante4, Lorena Fernandes Rosendo de Melo5, Pool Aníbal Alarcón León6 and Thalis Braga Batista7
- 1Specialist in Orthopedics and Traumatology, Santa Casa de Misericórdia de Maceió, Brazil
- 2Post-doctorate in cellular and molecular biology, CESMAC University Center, Rua Cônego Machado, Brazil
- 3Post-doctorate in cellular and molecular biology, CESMAC University Center, Rua Cônego Machado, Brazil
- 4Resident Physician in Orthopedics and Traumatology, Santa Casa de Misericórdia de Maceió Address: Avenida Moreira e Silva, Brazil
- 5Anesthesiology Resident Physician, Santa Casa de Misericórdia de Maceió, Rua Prof. Sandoval Arroxelas,
- 6Resident Physician in Orthopedics and Traumatology, Hospital Santa Casa de Misericórdia de Maceió, Rua Jangadeiros Alagoanos, Brazil
- 7Medical student at CESMAC University Center, CESMAC University Center, Rua Rodolfo Abreu, Cruz das Almas, Brazil
Received: February 03, 2020; Published: February 18, 2020
Corresponding author: Rogério Nascimento Costa, Specialist in Orthopedics and Traumatology, Santa Casa de Misericórdia de Maceió, Brazil.
DOI: 10.32474/RRHOAJ.2020.04.000198
Abstract
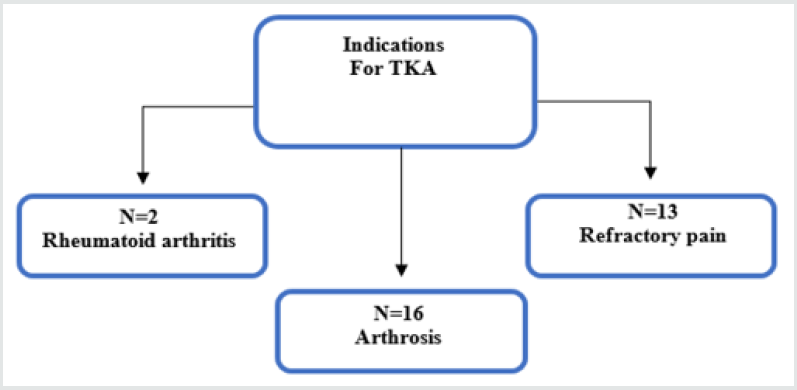
Total knee arthroplasty (TKA) is a very efficient surgical process in the treatment of degenerative knee changes. However, this procedure involves extensive tissue trauma, which contributes to the occurrence of severe postoperative pain. In this sense, pregabalin seems to be effective when administered before surgery with significant pain reduction and consequently the amount of opioid used postoperatively. Considering the importance of the subject and considering that there is no work in Alagoas and or Northeast Brazilian populations that justifies the advantages of using Pregabalin in the preoperative period of TKA, this study aims to gather information collected from patients operated at Santa Casa de Misericórdia de Maceió in a period of one year. Thirty-six patients were studied during the research, where four were excluded due to data collection failure. The main indications for TKA were 2 patients with rheumatoid arthritis, 16 with arthrosis and 13 with refractory pain. In this context, pregabalin has recognized side effects, but in the study, it was observed safety in the administration of this drug in the patient group 24 hours before the surgical procedure compared to the patient group 1 hour earlier as shown in Table 1. A greater reduction was observed. of pain according to VAS pain 24 and 48 hours after surgery, in the pregabalin group 24 hours before, in relation to the others. No decrease in postoperative opiod use was observed, as no study group achieved a VAS pain lower than 3 points over the length of stay. Therefore, a larger study with larger patient samples and case-controls is needed to obtain significant results.
Keywords: Total knee arthroplasty; pregabalin;opioid; postoperative; Placebo
Introduction
Total knee arthroplasty (TKA) is a highly successful operation in the treatment of degenerative knee changes and is in increasing demand worldwide due to the aging population and the need to preserve people’s quality of life. However, it involves extensive tissue trauma, which contributes to the occurrence of severe postoperative pain, and analgesia in this phase is of fundamental importance Zabeu, Migon, Junior [1]. Approximately half of patients undergoing TKA experience severe pain after the procedure. Postoperative pain not only represents a time of physical and emotional distress, but also negatively affects patient recovery Jokela et al. [2]. As with inflammatory metabolic endocrine response secondary to surgical trauma, untreated or inadequately treated pain leads to changes in the endocrine, cardiovascular, and central, peripheral, and sympathetic nervous systems. There is release of catabolic hormones such as cortisol, glucagon, growth hormone, endogenous catecholamines and inflammatory cytokines resulting in immunological impairment Berber, Mcguire, Click [3]. We can also cite for example increased oxygen demand and increased pressure on the cardiovascular system, which may then be associated with serious complications including ischemic cardiac events and myocardial insufficiency, which results in increased pressure on the arterial system Sinastra, Torres, Bustos [4].In addition, pain immobilization may increase the risk of reduced lung function, gastrointestinal complications, and thrombus formation that are related to surgical stress Apfelbaum et al.[5]. In particular, such complications may negatively affect the mental status of elderly patients, causing delirium and or anxiety. In addition, severe uncontrolled immediate postoperative pain may progress to chronic pain due to sensitization of the nervous system Aubrun et al. [6]. Thus, early rehabilitation and recovery may be delayed, resulting in longer hospital stays and increased hospital costs Abu Shahwan [7], Filos, Lehmann, [8], Amin Hanjani et al. [9], Antall, Kresevic [10], Arnett , Jones, Horger [11], Arthur et al. [12] Bamigboye, Hofmeyr [13].Faced with this problem, adequate pain management after TKA has been sought. It is not just for the human purpose of releasing patients from suffering but is essential for success in terms of improving patient satisfaction, quality of life and preventing complications. The most important concept of current pain management after TKA is preventive use through a multimodal approach Kehlet, Dahj [14].
“Preference” refers to initiating pain management prior to surgical stimuli. In addition, “multimodal approach” means more than 2 drugs or modalities with different mechanisms or sites for synergistic effects. These two concepts are also known to be extremely effective in reducing opioid consumption, which has been associated with high complication rates Mathiesen, Moiniche, Dahl [15].Recently, several guidelines for postoperative pain management have emerged, one of which recommends the use of pregabalin as part of a multimodal regimen in patients undergoing surgery. This drug is associated with a reduced need for opioids after any surgical procedure, and some studies have reported lower incidence of postoperative pain Gonano et al [16]. Pregabalin has hyperanalgesic action in humans and is also used to treat chronic neuropathic pain Ifuku et al. [17]. Also, when used preoperatively, it can play a role in preventing acute pain from developing in chronic pain Katz, Clarke, Seltzer [18]. Although pregabalin was initially identified as treatments for neuropathic pain and other neurological disorders, several recent comments have revealed that pregabalin also reduces postoperative opioid consumption and improves pain levels after spinal surgery, laparoscopic surgery and thyroidectomy. Macrae, Davies [19]. Thus, there are no comprehensive data regarding the analgesic efficacy of pregabalin in patients undergoing Tka Chizh Ba et al. [20]. In this sense, pregabalin appears to be effective when administered at a preoperative dose of 150 to 300 mg, one to two hours before surgery. Although some trials have also tested regimens including postoperative dosing, proving to be equally effective, typically using pregabalin 150 to 300 mg after 12 hours of the procedure Singla et al. [21]. This study gathered information collected from patients who underwent surgery and who participated in 3 intervention groups: pregabalin 1 hour before and placebo 24 hours before; pregabalin 24 hours before the procedure and placebo 1h before; placebo 1h and 24h before; being analyzed using pain assessment scales.
Methods
Design: Randomized clinical trial.
Local: Orthopedics and Traumatology Service of the Santa Casa de Misericórdia Maceió.
Sample: The sampling was done by convenience, inviting all patients submitted to total knee arthroplasty at the Santa Casa de Misericórdia de Maceió from August 2018 to May 2019.
Sampling: Patients who underwent surgical treatment of total knee arthroplast (TKA) within one year from the month of AUGUST 2018, who meet the inclusion criteria mentioned in item 3.4.1, and agree to participate in the research according to Informed Consent (IC), being submitted for evaluation according to the VAS and an adverse effects questionnaire.
Inclusion criteria
Patients with knee gonarthrosis who underwent surgical
intervention for total knee arthroplasty.
Over 50 years at the time of surgery.
Exclusion criteria
Patients undergoing total knee arthroplasty for any indication other than gonarthrosis. Known or suspected sensitivity or contraindication to pregabalin. Pacientes com hipersensibilidade a dipirona e tramadol conjuntamente. Patients who have a neurocognitive disorder that prevents them from communicating with interviewers. Patients with rare hereditary problems of galactose intolerance, Lactase deficiency, Lapp deficiency or glucose-galactose malabsorption. Patients with heart problems, edema, renal failure, uncontrolled hypertension or hyperaldosteronism.
Methodological procedures
After the consent of the informed consent, the patients received a brief explanation about the criteria that will evaluate the postoperative period of the surgery to which it was submitted and about the questionnaires to be applied. Pregabalin and sodium bicarbonate hypersensitivity tests were performed, with the permission of the patient who wishes to volunteer the research, during the preoperative consultations, before ingestion of these drugs. Eligible patients were randomized into three groups, two intervention groups and one control group, using the Random Allocation Software version 1.0 program. Group 01 patients received placebo 24 hours before surgery and pregabalin one hour before surgery. Group 02 patients received pregabalin tablet 24h before and placebo tablet 1 hour before the surgical procedure. Patients in group 03, control group, received the placebo tablet 24 hours before surgery and placebo 1h before surgery. Subjects from the experimental group received pregabalin at a dosage of 300mg. In the control groups a tablet containing sodium bicarbonate of the same color, size, shape and weight as pregabalin tablets will serve as a placebo. A researcher B, who is unaware of the result of randomization, will administer the pills after being directed by researcher A, who consulting the list of random numbers defines which group the patient belongs to. Another blind C researcher was responsible for the outcome assessment. All groups underwent arthroplasty under spinal anesthesia with 20mg isobaric bupvacaine and at the end of the procedure, femoral nerve block with 0.25% levobupivacaine was performed to complement the analgesia. The surgical technique of total knee prosthesis is described in annex 3. Statistical analysis of the data was performed by the program in Epi-Info ;7.1 and then a profile of the patients was drawn, and the data distributed in tables and graphs of descriptive statistics, in order to allow analysis and further discussion.
Results
Thirty-six patients were studied during the research, where
four were excluded due to data collection failure. The main
indications for TKA were 2 patients with rheumatoid arthritis,
16 with arthrosis and 13 with refractory pain (Figure 1). Thus, of
the 32 participants, 25 patients presented deformity in genuvaro
and 7 in genuvalgo. The average age of the volunteers was 69
years ranging from 53 to 93 years, with a total of 22 female and
10 male patients. It should also be noted that 22 patients reported
that they clearly understood the surgery, its possible detrimental
effects on their health and postoperative pain. As is well known by
the medical profession, the process of knee degeneration due to
arthrosis is mechanical, thus, 100% of the patients presented pain
with the standard ambulation movement. Of these patients, 51%
had reduced and or limited knee extension and flexion movements,
requiring even a wheelchair for locomotion.
In this context, the degree of limitation was so extensive that 16
patients (~ 50%) reported that they could not effectively perform
even their personal hygiene activities, as an example. The vast
majority of patients who have undergone this surgical procedure
have had pain for years, consequently abusing NSAIDs, common
analgesics and even morphine-derived analgesics. Regarding the
undesirable effects of the drugs during the research, no cases of
constipation, vomiting, attention disorder or mental confusion
were found in any group. In the pregabalin group 1h before, cases of
dizziness (n = 3), drowsiness (n = 2), insomnia (n = 1) and nausea (n =
1) were reported. None of these effects were found in the pregabalin
group 24h before. In the placebo group there were reports of
nausea (n = 1), dizziness (n = 5) and drowsiness (n = 2) (Chart 1).
During the research it was found that only 18.1% of patients had
pathological knee pain less than 1 year and 81.8% reported pain for
more than 3 years, some cases reaching even 20 years of pain. Data
on the Visual Analog Pain Scale (VAS) indicate that patients who did
not take pregabalin before surgery, totaling 16 patients, reported
an average VAS of 9.19. Concomitantly, patients taking pregabalin
one hour before surgery (13 total) or 24 hours before surgery (4
total) reported mean VAS of 6.0 and 7.0, respectively, indicating a
possible “immediate” analgesic action”. of the drug. Also, regarding
pain data, in all three groups analyzed, there was a reduction in the
mean value reported for VAS (Table 1) when comparing pre- and
post-operative 24 hours or 48 hours after the end of the surgical
procedure. However, when applying a Student’s t-test to compare
such groups, statistical significance was observed in the VAS
values of patients undergoing placebo treatment at postoperative
evaluation 24h and 48h. In the pregabalin 1h before (P1B) and
pregabalin 24 hours before (P24B) groups, statistical significance
was observed in the 24h postoperative VAS assessments (Table
1). These results indicate a possible partial blocking activity of the
action of opioids administered postoperatively. Such antagonism
can be explained by the action that pregabalin exerts by inhibiting
the release of Serotonin and Noradrenaline, thereby preventing
the indirect action of tramadol, which involves the inhibition of
Noradrenaline and Serotonin reuptake which is essential for pain
reduction.
Table 1: Mean value reported in VAS by patients undergoing TKA surgery.
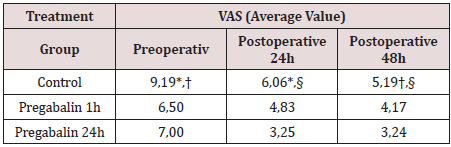
* Significant difference, Student’s t-test, p < 0,001
† Significant difference, Student’s t-test, p < 0,001
§ Significant difference, Student’s t-test, p < 0,001
Discussion
Evaluation of Pain and Quantity of Opioids: Pregabalin is a structural analog compound of gamma aminobutyric acid (GABA) and acts on the central nervous system because it crosses the blood-brain barrier Bockbrader [22], due to this property its anticonvulsant, antihyperalgesic and anxiolytic actions. However, it binds with high affinity and specificity to voltage-dependent calcium channel alpha2-delta-1 proteins in the Central Nervous System, inhibiting their functional expression. This also inhibits calcium influx and the action of noradrenaline and serotonin neurotransmitters in the synaptic cleft Davies et al. [23], Field et al. [24], Gajraj [25]. These same neurotransmitters are part of the tramadol antinociception mechanism of action which, through two differents and independents but synergistic mechanisms of action, acts as an opioid agonist and indirectly performs an action contrary to that of pregabalin, as it triggers mechanisms that inhibit the reuptake of noradrenaline and serotonin Driessen [26], Dayer [27]. As this pharmacokinetics of pregabalin and tramadol have been studied in animals and in vitro separately, further studies are needed to elucidate such drug interaction. However, this is the possible explanation for the fact that in our study similar effects of pain reduction were found between the groups receiving Placebo preoperatively and the pregabalin groups, both 1h before and 24h before surgery, as both used tramadol, as recommended by the Santa Casa Maceió antinociception guide. In the pregabalin groups, both P1B and P24B at the time of surgery had a reduced VAS compared to the control group. It was observed that in the P1B group there was an immediate effect (1h after administration) and that lasted until the 24h postoperative reevaluation, however, there was no statistically significant reduction in the 48h postoperative period. As in the P24B group, pain reduction was statistically significant at the time of surgery (24h post-administration) and 24h postoperatively, and it was found that the antinociceptive effects of pregabalin did not last until the 48h postoperative reevaluation in any of the patients. group. Pharmacodynamicly this fact can be explained due to the fast absorption of pregabalin, reaching the maximum plasma concentration in about 1 hour and its half-life being around 7 hours, thus explaining its ineffectiveness in post 48h of medication administration Bockbrader [22]. It is also observed that these characteristics did not change even when pregabalin is associated with tramadol Lee [28]. Effective pain reduction at the time of surgery (1h after administration) and 24h postoperatively when administering pregabalin (300mg) 1 hour before the procedure was also found by a Brazilian study conducted by Santiago et al. who, however, no significant reduction in inflammation mediating interleukin levels was found. Seeing that the immediate hypoalgesic effect (1 hour after administration) is present both when there are surgical procedures and false surgeries, thus observing the character of pregabalin for neuropathic pain reduction Rodrigues [29], Pourfakhr [30]. Corroborating our findings of hypoalgesia lasting up to 24 hours in both pregabalin groups even under a regime of implicit drug combinations of anesthetic procedures and after surgical trauma were also found by Zhang [31], Sattari [32], Park [7] and Sawan [33]. However, in the study by Khetarpal (2016) involving lower limb orthopedic surgeries, the pregabalin group (300mg) found effective hypoalgesia up to a maximum time of about 15h. The character of dose-dependent hypoalgesia becomes observable in a study using pregabalin 75mg to reduce postoperative septorhinoplasty pain in which the effectiveness remained until 6h after the procedure and did not persist in the 24-hour reassessment Pourfakhr [30]. In this context, one should enthusiastically assess the fact that chronic post-thoracotomy pain does not persist with pregabalin for a prolonged period of 14 days, which gives patients a better quality of life Anwar [34]. However, further studies are needed to elucidate the correct longterm pregabalin prescription regimen for eliminating chronic postoperative pain. However, in a study conducted in South Korea, a 75 mg dose of the drug (pregabalin) in tablet form was used one night before surgery and one capsule once a night until the 2nd postoperative day. In this study, there was no difference between the control group and the placebo group YIK, Jing Hui Et Al [35]. Similar research was conducted with a total of 70 patients undergoing abdominal gastroplasty who randomly received oral pregabalin (75 mg) or an identical placebo 1 hour before surgery. Again, it was shown that there was no improvement in the quality of postoperative patient recovery and not even pain reduction Martins Et Al. [36]. As the effectiveness of postoperative pain reduction has been demonstrated with dosages of 150mg and 300mg Singla et al. [37] these interpretations become questionable.
Unwanted effects
Undesirable effects in the 3 groups were not significant, a few patients on pregabalin or placebo experienced dizziness, drowsiness or nausea. However, none of the groups demonstrated sufficient effects to distinguish the causative drug in isolation, mainly because tramadol was used in all groups. A Korean study with healthy patients showed no increase in adverse effects when combining tramadol with pregabalin Lee [37]. Similar results with the use of pregabalin for postoperative pain reduction were found by Martins [36], Zhang [31], Mathiesen [15] respectively after bariatric cholecystectomy and hip arthroplasty procedure. In a postoperative TKA study following pregabalin use for another 3 months no patient had a common adverse effect of pregabalin even though the study addressed an extensive list of endocrine, cardiovascular, respiratory, neurological, gastrointestinal, musculoskeletal, psychiatric disorders. and renal YIK [35]. The importance of assessing the amount of adverse effects in the control and pregabalin groups is even more necessary after studies in thoracic surgery relating the pregabalin groups to the reduction of adverse effects, especially headache, dysuria, constipation and nausea LI [38]. However, Park’s (2016) study found a significantly prevalent finding of blurred vision in the postoperative period after nasal surgery when using pregabalin before anesthesia [39-45].
Conclusion
Pregabalin has recognized side effects, but in the study, it was observed safety in the administration of this drug in the patient group 24 hours before the surgical procedure compared to the patient group 1 hour before, as shown in (Table 1). There was a greater reduction in pain according to VAS in the postoperative period of 24 and 48 hours in the pregabalin group 24 hours before, compared to the others [45-49], as shown in Table 1. No decrease in postoperative opiod use was observed, as no study group achieved a VAS pain lower than 3 points over the length of stay. Therefore, a larger study with larger patient samples and case controls is needed to obtain significant results.
References
- Zabeu JL, Migon EZ, Alves WM (2010) Pain following total knee arthroplasty -a systematic approach. Campinas Rev Bras Ortop V 45(5): 384-339.
- Jokela R, Ahonen J, Tallgren M, Haanpaa M, Korttila K, et al. (2008) Premedication with pregabalin 75 or 150 mg with ibuprofen to control pain after day-case gynaecological laparoscopic surgery. Br J Anaesth 100(6): 834-840.
- Barber FA, McGuire DA, Click S (1998) Continuous-flow cold therapy for outpatient anterior cruciate ligament reconstruction. Arthroscopy 14(2): 130-135.
- Sinatra RS, Torres J, Bustos AM (2002) Pain management after major orthopedic surgery: current strategies and new concepts. J Am AcadOrthop Surg 10(2): 117-129.
- Apfelbaum JL, Chen C, Mehta SS, Gan TJ (2003) Postoperative pain experience: Results from a national survey suggest postoperative pain continues to be undermanaged. AnesthAnalg 97(2): 534-540.
- Aubrun F, Langeron O, Heitz D, Coriat P, Riou B, et al. (2000) Randomised, placebo-controlled study of the postoperative analgesic effects of ketoprofen after spinal fusion surgery. ActaAnaesthesiolScand 44(8): 934-939.
- Abu Shahwan I (2008) Ketamine does not reduce postoperative morphine consumption after tonsillectomy in children. Clin J Pain 24(5): 395-398.
- Filos KS, Lehmann KA (1999) Current concepts and practice in postoperative pain management: need for a change? EurSurg Res 31(2): 97-107.
- Amin Hanjani S, Corcoran J, Chatwani A (1992) Cold therapy in the management of postoperative cesarean section pain. Am J ObstetGynecol 167(1): 108-109.
- Antall GF, Kresevic D (2004) The use of guided imagery to manage pain in an elderly orthopedic population. OrthopNurs 23(5): 335-340.
- Arnett RM, Jones JS, Horger EO (1990) Effectiveness of 1% lidocaine dorsal penile nerve block in infant circumcision. Am J ObstetGynecol 163(3): 1074-1080.
- Arthur HM, Daniels C, McKelvie R, Hirsh J, Rush B (2000) Effect of a preoperative intervention on preoperative and postoperative outcomes in low-risk patients awaiting elective coronary artery bypass graft surgery. A randomized, controlled trial. Ann Intern Med 133(4): 253-262.
- Bamigboye AA, Hofmeyr GJ (2009) Local anesthetic wound infiltration and abdominal nerves block during caesarean section for postoperative pain relief. Cochrane Database Syst Rev 8(3): CD006954.
- Kehlet H, Dahl JB (2003) Anaesthesia, surgery, and challenges in postoperative recovery. The Lancet362(9399): 1921-1928.
- Mathiesen O, Moiniche S, Dahl JB (2007) Gabapentin and postoperative pain: A qualitative and quantitative systematic review, with focus on procedure. BMC Anesthesiol 7: p. 6.
- Gonano C, Latzke D, SabetiAschraf M, Kettner SC, Chiari A, et al. (2011) The anxiolytic effect of pregabalin in outpatients undergoing minor orthopedic surgery. J Psychopharmacol 25(2): 249-253.
- Ifuku M, Iseki M, Hidaka I, Morita Y, Komatus S, et al. (2011) Replacement of gabapentin with pregabalin in postherpetic neuralgia therapy. Pain Med 12(7): 1112-1116.
- Katz J, Clarke H, Seltzer Z (2011) Preventive analgesia: quo vadimus? AnesthAnalg 113(5): 1242-1253.
- Macrae W, Davies H (1999) Chronic post-surgical pain. In: Crombie IK, Linton S, Croft P, Von Knorff M, LeResche L, editors. Epidemiology of pain. Washington, DC: IASP Press 125-142.
- Chizh BA, Gohring M, Troster A, Quartey GK, Schmelz M, et al. (2007) Effects of oral pregabalin and aprepitant on pain and central sensitization in the electrical hyperalgesia model in human volunteers. Br J Anaesth 98(2): 246-254.
- Singla NK, Chelly JE, Lionberger DR, Gimbel J, Sanin L, et al. (2014) Pregabalin for the treatment of postoperative pain: results from three controlled trials using different surgical models. Journal of pain Research Pasadena 8: 9-20.
- Bockbrader H, Wesche D, Miller R, Chapel S, Janiczek N, et al. (2010) A comparison of the pharmacokinetics and pharmacodynamics of pregabalin and gabapentin. Clinical Pharmacokinetics, Michigan, USA 49:661–669.
- Davies, Anthony (2007) Functional biology of the α2δ subunits of voltage-gated calcium channels. Trends in pharmacological sciences 28(5): 220-228.
- Field, Mark J, OLES, Ryszard J, SINGH, Lakhbir (2001) Pregabalin may represent a novel class of anxiolytic agents with a broad spectrum of activity. British journal of pharmacology 132(1):1-4.
- Gajraj N (2007) Pregabalin: its pharmacology and use in pain management. Anesthesia & Analgesia Journal, Texas, USA 105: 1805–1815.
- Driessen B, Reimann W, Giertz H (1993) Effects of the central analgesic tramadol on the uptake and release of noradrenaline and dopamine in vitro. British journal of pharmacology 108(3): 806-811.
- Dayer Pierre, Collart Laurence, Desmeules Jules (1994) The pharmacology of tramadol. Drugs 47(1): 3-7.
- LEE, Soyoung (2018) A pharmacokinetic drug-drug interaction study between pregabalin and tramadol in healthy volunteers. European journal of clinical pharmacology74(12): 1605-1613.
- Rodrigues, Rafaela Figueiredo (2016) Influência da duloxetina e amitriptilina na farmacocinética e efeito biológico da pregabalina para tratamento da dor crônica em animais.
- Pourfakhr, Pejman (2019) Low-dose preoperative pregabalin improves postoperative pain management in septorhinoplasty surgery: a double-blind randomized clinical trial. European Archives of Oto-Rhino-Laryngology 276(8):2243-2249.
- Zhang Dan, You, Guangqiang YAO, Xiaoxiao (2019) Influence of pregabalin on post-operative pain after laparoscopic cholecystectomy: A meta-analysis of randomized controlled trials. Journal of Minimal Acess Surgery.
- Sattari, Hossein (2018) Preoperative oral pregabalin reduces acute pain after thoracotomy. Open access Macedonian journal of medical sciences 6(9):1606-1610.
- Sawan, Hind (2014) Pregabalin reduces opioid consumption and improves outcome in chronic pain patients undergoing total knee arthroplasty. The Physician and sportsmedicine42(2): 10-8.
- Anwar, Sibtain (2019) Prolonged Perioperative Use of Pregabalin and Ketamine to Prevent Persistent Pain after Cardiac Surgery. Anesthesiology: The Journal of the American Society of Anesthesiologists 131(1): 119-131.
- Yik JH, Tham WYW, Tay KH, Shen L, Krishna L, et al. (2019) Perioperative pregabalin does not reduce opioid requirements in total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy 27(7): 2104-2110.
- Martins, Marcelo (2018) Pregabalin to improve postoperative recovery in bariatric surgery: a parallel, randomized, double-blinded, placebo-controlled study. Journal of pain research 11: 2407-2415.
- LEE, Cheol (2018) Pregabalin and Dexmedetomidine Combined for Pain After Total Knee Arthroplasty or Total Hip Arthroplasty Performed Under Spinal Anesthesia. Orthopedics41(6):365-370.
- LI, Shuangjiang (2019) Does pregabalin effectively and safely relieve postoperative pain in patients undergoing pulmonary resections? Interactive cardiovascular and thoracic surgery29(4):555-560.
- Bockbrader, Howard N. et al. (2010) Clinical pharmacokinetics of pregabalin in healthy volunteers. The Journal of Clinical Pharmacology 50(8): 941-950.
- Follin SL, Charland SL (1997) Acute pain management: operative or medical procedures and trauma. Ann Pharmacother. 31(9): 1068-1076.
- Maheshwari AV, Blum YC, Shekhar L, Ranawat AS, Ranawat CS, et al. (2009) Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopedic Center. Clin OrthopRelat Res 467(6): 1418-1423.
- Mangano DT, Wong MG, London MJ, Tubau JF, Rapp JA, et al. (1991) Perioperative myocardial ischemia in patients undergoing non cardiac surgery--II: Incidence and severity during the 1st week after surgery. The Study of Perioperative Ischemia (SPI) Research Group J Am CollCardiol 17(4): 851-857.
- Park KK, Shin KS, Chang CB, Kim SJ, Kim TK, et al. (2007) Functional disabilities and issues of concern in female Asian patients before TKA. Clin OrthopRelat Res 461: 143-52.
- Ballantyne JC, Carr DB, de Ferranti S, Suarez T, Lau J, et al. (1998) The comparative effects of postoperative analgesic therapies on pulmonary outcome: cumulative meta-analyses of randomized, controlled trials. AnesthAnalg 86(3): 598-612.
- Butler GS, Hurley CAM, Buchanan KL, Smith VanHorne J (1996) Prehospital education: Effectiveness with total hip replacement surgery patients. Patient EducCouns 29(2): 189-197.
- Freedman BM, O’Hara E (2008) Pregabalin has opioid-sparing effects following augmentation mammoplasty. AesthetSurg J 28(4): 421-424.
- Ittichaikulthol W, Virankabutra T, Kunopart M, KhamhomW, Putarawuthichai P, et al. (2009) Effects of pregabalin on post-operative morphine consumption after abdominal hysterectomy with/without salphingooophorectomy: A randomized, double-blind trial. J Med Assoc Thai 92(10): 1318-1323.
- Parvataneni HK, Ranawat AS, Ranawat CS (2007) The use of local periarticular injections in the management of postoperative pain after total hip and knee replacement: a multimodal approach. Instr Course Lect 56: 125-131.
- Khetarpal, Ranjana (2016) Gabapentin vs pregabalin as a premedication in lower limb orthopaedics surgery under combined spinal epidural technique. Anesthesia, essays and researches10(2)262-267.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...

.png)