Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6679
Review Article(ISSN: 2637-6679) 
Current Clinical Applications of 3D Printing in Spine Surgery: A Literature Review Volume 8 - Issue 1
Konstantinos Paraskevopoulos1*, Anthimos Keskinis2, Maria Alexanidou3, Konstantinos Tilkeridis4 and Athanasios N Ververidis5
- 1Medical School, Democritus University of Thrace, University General Hospital of Alexandroupolis, Greece
- 2Specialty trainee in Orthopedic Surgery, Department of Orthopedic Surgery, Medical School, Democritus University of Thrace, University General Hospital of Alexandroupolis, Greece
- 3Apostolos Loukas’ Medical Center, Cyprus
- 4Associate Professor, Department of Orthopedic Surgery, Medical School, Democritus University of Thrace, University General Hospital of Alexadroupolis, Greece
- 55Professor, Department of Orthopedic Surgery, Medical School, Democritus University of Thrace, University General Hospital of Alexandroupolis, Greece
Received: June 01, 2023; Published: June 08, 2023
Corresponding author: Konstantinos Paraskevopoulos, Medical School, Democritus University of Thrace, University General Hospital of Alexandroupolis, Greece
DOI: 10.32474/RRHOAJ.2023.08.000280
Abstract
Three-dimensional printing (3DP), also known as additive manufacturing (AM), has emerged as a recent advancement in the medical field, offering the capability to produce 3D printed bio models. This innovative technology has found various applications within the medical community, particularly in orthopedics and, more specifically, in the field of spinal surgery. The implementation of 3DP in spine surgery has yielded numerous benefits, both in the pre-operative and intra-operative settings. In the realm of preoperative planning, 3DP has facilitated educational programs, enabling enhanced visualization and comprehension of complex spinal pathologies. Additionally, it has provided spine surgeons with precise pedicle screw insertion models, patient-specific templates, guides, and devices. These advancements have proven particularly valuable in challenging spinal surgeries, encompassing fractures, tumors, infections, degenerative diseases, and spinal deformities such as scoliosis or varus deformity. While 3DP technology offers significant advantages, it is important to acknowledge the associated limitations and concerns. These include the high installation cost, increased pre-operative time required for planning and printing processes, the need for specialized personnel to operate the technology effectively, and the inherent limitations in accurately simulating soft tissue and bony structures. The objective of this mini-review article was to comprehensively analyze the current clinical applications of 3DP in spine surgery, specifically focusing on its utilization in both the pre-operative and intra-operative settings. By examining the advantages and limitations of 3DP, this article aims to provide insights into its efficacy, potential pitfalls, and considerations relevant to its implementation in the field of spinal surgery.
Keywords: 3D Printing; 3DP Technology; Additive Manufacturing; Spine Surgery; Bio models; AM Models
Introduction
Three-dimensional printing (3DP), also referred to as additive manufacturing (AM), was initially introduced to clinical practice twenty years ago [1,2]. Since its emergence in the 1980s, 3DP has garnered substantial attention. However, recent significant technological advancements have propelled its growth, enabling the production of large-scale items, such as cars. The relatively low cost of 3DP has contributed to its rapid expansion in the medical field [3]. This novel technology has been successfully applied by surgeons across diverse clinical conditions, encompassing craniofacial prostheses, cardiothoracic surgery, dermatological grafts, human earlobes, and orthopedic surgery [1,4-6]. In contrast to conventional manufacturing techniques, which involve material removal to create objects, AM employs layer-by-layer additive processes guided by Computer-Aided Design (CAD) models, facilitating the production of 3D printed models [5,7]. While AM has been utilized in spine surgery since the 1990s, recent years have witnessed a remarkable evolution in its application for managing various spinal conditions, ranging from tumors to trauma, infections, deformities, and degenerative diseases [8-10]. Contemporary applications of 3DP technology encompass both the pre-operative and intra-operative settings within spine surgery. Elaborately crafted anatomical models of spinal deformities are specifically designed for pre-operative purposes, enabling surgical planning, patient education, and training for residents and fellows, as well as replicating diverse spinal pathologies. Furthermore, in the intra-operative setting, 3DP has been employed to produce insertion guidance systems, templates, and implants [8,11]. The objective of this mini-review article is to comprehensively analyze the current clinical applications of 3DP in pre-operative and intra-operative settings within spine surgery, shedding light on its multifaceted utility.
Process Of 3D Printing
Three-dimensional printing (3DP) includes two main manufacturing approaches: additive and subtractive methods. The additive approach, predominantly employed in orthopedic device fabrication, involves layer-by-layer addition of materials to achieve high precision in the final product [1,12]. The 3DP process comprises three stages: image acquisition, image post-processing, and 3DP itself (13). Image acquisition methods differ depending on the intended subject to be printed. For rapid prototyping of devices such as implants, guides, and prostheses, computer-aided design (CAD) programs are utilized, enabling surgical intervention during the design phase [12,13]. Conversely, the manufacturing of custom-made anatomical models necessitates the use of computed tomography (CT) and magnetic resonance imaging (MRI) to obtain detailed depictions of the patient’s anatomy [12,13]. High-quality images are essential to ensure precise design accuracy [1,7]. While CT enables the acquisition of thin-section axial images with submillimeter slice thickness, MRI provides accurate visualization of articular cartilage and extra-osseous abnormalities, albeit with potential image quality limitations due to patient motion during scanning [13].
The acquired images are stored in the digital imaging and communications in medicine (DICOM) format, subsequently edited using image post-processing software, and exported in the Standard Triangular Language (STL) format [7,12,13]. STL, developed in 1984 by Chuck Hall, is a software language that encodes processed images into a suitable format compatible with 3D printers [12]. After slicing the 3D digital model into layers, the printing process commences by adding material layer by layer [12,13]. Various printing technologies exist, including stereolithography apparatus (SLA), fused deposition modeling (FDM), selective laser sintering (SLS), and electron beam melting (EBM), each differing in construction quality and usability [13]. Physicians commonly employ office 3D printers, such as FDM and SLA [12]. Material selection is of paramount importance, considering factors such as mechanical strength and structural requirements specific to the intended application. Commonly utilized materials encompass metals, bio ceramics, synthetic polymers, and natural polymers. Achieving compatibility between the chosen material and the structure’s mechanical properties and target tissue remains a significant challenge, one that 3DP aims to address [1].
Application in Orthopedic Surgery
The increasing affordability and accessibility of 3DP have led to significant advancements in the field, particularly benefiting orthopedic surgeons. With the continuous development of the sector, surgeons are gaining valuable experience, and the applications of 3DP in orthopedics are expanding. Common applications in orthopedic surgery include the production of anatomical models, implants, patient- specific tools, or jigs, and [14] graft substitute printing [16]. The utilization of 3D printed models offers substantial improvements in understanding the patient’s anatomy and facilitates a comprehensive pre-operative assessment of fractures or deformities, such as scoliosis or varus deformity [12]. Anatomical models also aid in pre-operative planning, including screw measurement and anatomical plate selection [4,12]. Furthermore, they have educational value for discussions with patients, education of less experienced physicians, and surgical training [7]. Patient education regarding the pathology and surgical approach is enhanced, reducing anxiety and uncertainty [12, 17]. Custom- made implants, tools, and jigs play a prominent role in various orthopedic procedures such as total joint arthroplasties (TJA), orthopedic oncology, traumatology, spine surgery, and deformity correction [1,12, 18]. These customized devices are used to replace degenerated, crushed, or cancerous bone tissue, as well as to guide surgeons accurately during bony cuts, implant placement, and overall surgical precision [1]. In certain cases of TJA, where conventionally designed implants are not suitable, custom-made implants are the only viable option, particularly in individuals with unique anatomical considerations such as dwarfs [4]. In addition to their pre- and intra-operative contributions, 3DP technology also enables the production of custom- made immobilization devices, external aids, and prosthetics for individuals with amputated limbs [4,12]. These personalized instruments address challenges associated with breathability and weight, offering enhanced comfort, and facilitating uncomplicated recovery for patients [4].
Application In Spine Surgery
Pre-operative setting
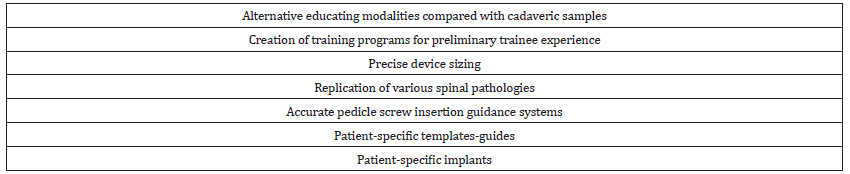
In the field of spine surgery, the application of AM or 3DP technology in the pre-operative setting has proven beneficial, leading to improved surgical planning, reduced operative time, enhanced surgical precision, and decreased intra-operative blood loss, particularly in complex spinal deformities [19,20]. Various spinal conditions, including severe scoliosis, spine tumors, rheumatoid arthritis of the cervical spine, and degenerative spine disease, can be effectively managed with the implementation of 3DP technology through the crea tion of patient-specific anatomical models (Table 1) [21]. The use of 3D printed models in spine surgery offers advantages over traditional cadaveric samples, including fewer cultural, medicolegal, security, and accessibility concerns, making them a viable alternative for educational purposes [10,22]. Residents and fellows specializing in spine surgery can benefit from 3D printed models as they provide an opportunity to gain preliminary experience in various surgical maneuvers, potentially reducing the learning curve. Additionally, 3DP technology allows for the development of training programs aimed at enhancing trainees’ skills in general anatomy and pathology. However, it should be noted that while 3DP models are practical, they may not accurately replicate the details and textures of soft tissues, and cadaveric specimens are still considered the gold standard for training programs [22].
Another area revolutionized by 3DP technology in spine surgery is device sizing. Precisely designed devices built with the assistance of dynamic bio models enable the performance of sophisticated surgical approaches, such as decompression or restoration of sagittal balance, with improved surgical outcomes. By utilizing 3DP technology, the need for multiple trial device insertions in vulnerable areas, which can potentially cause neurological damage, can be reduced, thereby reducing surgical time and associated risks [23]. For example, a study by Thespian et al. demonstrated the utilization of 3D printed bio models in a series of 129 patients undergoing minimally invasive transforaminal lumbar interbody fusion. The bio model, along with 3D printed tools, pedicle screws, rods, and cages, all customized for each patient, were used for pre-operative planning and patient education. The surgeon required less than five minutes for pre-operative planning, and all patients reported satisfaction and improved understanding of the underlying pathology and surgical procedure [24]. Another study by Bohl et al. utilized a Living Spine Model (LSM) created through 3DP to assess face and content validity in open posterior lumbar surgery. Less experienced residents took longer to complete the procedure and placed fewer pedicle screws compared to more experienced surgeons. The overall face validity ranged between 60-97%, and the content validity suggested that the LSM could be a potential tool for surgical education and testing in open posterior lumbar surgery [25]. Furthermore, a systematic review by Lopez et al. examined the benefits of 3DP in pre-operative planning and pedicle screw placement in spinal deformity. Most of the reviewed articles indicated that 3DP provided residents with a better understanding of spinal anatomy and associated osseous structures, thus facilitating the surgical procedure. Additionally, the application of 3DP in educational and training settings resulted in improved communication and confidence among surgical team members [26].
Intra-operative setting
Pedicle screws play a critical role in spine surgery as they provide effective vertebral stabilization. However, due to the anatomical complexity of the surgical site, which often involves proximity to neurovascular structures, the insertion of pedicle screws (PSI) can be challenging and carries the risk of severe neurological damage, even in the hands of experienced surgeons [27,28]. Conventional techniques of freehand screw insertion have shown pedicle cortex breaching rates ranging from 25% to 43% (11). To address these challenges, the application of 3DP technology has emerged as a promising approach to improve the accuracy and precision of PSI, particularly in challenging scenarios such as the cervical spine region, spinal deformities, and pediatric patients [27,28].
The utilization of 3D printed personalized guides and templates in pre-operative planning has provided several advantages for surgeons and the surgical team, including reduced operative time, decreased radiation exposure, and minimized iatrogenic complications [21,29]. For example, Zhang et al. conducted a randomized controlled trial (RCT) involving 40 patients to evaluate the feasibility of thermoplastic regulators combined with 3D printed templates for guiding pedicle needle insertion in percutaneous screw fixation (PPSF) for thoracolumbar fractures compared to conventional PPSF. The study demonstrated that the use of 3D printed templates was associated with lower post-operative Visual Analogue Scale (VAS) and Owelty Disability Index (ODI) scores, as well as a higher success rate for the initial pedicle insertion [30]. Another RCT by Feng et al. found that the use of 3D printed templates for cervical lateral mass screw insertion improved visualization of the operative area and increased the accuracy of screw insertion. A meta-analysis conducted by Yu et al. comparing the efficacy of 3D printed guide templates with freehand screw insertion reported that the use of 3D printed templates resulted in reduced operative time, intra-operative blood loss, and improved accuracy of pedicle screw placement [31].
AM has also been employed for the fabrication of personalized spinal implants, including spinal cages for interbody fusion surgery, vertebral replacements, implants for total disc replacement, and surgical reconstruction of bone defects following malignancies. However, the application of AM in personalized spinal implants is currently limited to complex spinal lesions in specific areas where it can provide anatomical and mechanical stability, leading to optimized osseointegration [19,28]. The use of personalized implants in these cases reduces intra-operative trauma and peri-operative morbidity, as it eliminates the need for surgical preparation to fit standard implants [20]. Additionally, 3D printing has been explored in the context of minimally invasive spine surgery (MISS). Patel et al. conducted a prospective study involving fifty-one patients to assess the efficacy of minimally invasive sacroiliac joint fusion (SJIF) using a 3D printed device. The study demonstrated that this technique resulted in improvements in pain, disability, physical status, and quality of life, as well as a reduction in opioid usage [32]. Zhuang et al., in a study involving fourteen subjects, investigated the efficacy of 3D printed vertebral body implantation combined with robotic radiotherapy in patients with spinal tumors. The authors reported successful reduction of symptoms, achievement of spinal stability, and tumor control without associated complications or adverse events [33].
Pitfalls and Concerns
While 3DP technology offers significant advantages in various medical applications, its widespread adoption is hindered by several concerns and limitations that warrant careful consideration [28,29]. These concerns encompass various important aspects that have been highlighted in literature. One of the primary concerns is the additional pre-operative time required for the creation of 3D printed bio models, which can take up to 12 hours to produce. This extended production time acts as a prohibitive factor, particularly in emergency cases and busy hospital settings where time is crucial [28]. Another major limitation is the high cost associated with the installation of 3DP technology, including the acquisition of specialized software, 3D printers, cameras, and the maintenance of these devices. This cost factor is particularly relevant in hospitals where complex spinal lesions are encountered infrequently, making it challenging to justify the significant financial investment required [29].
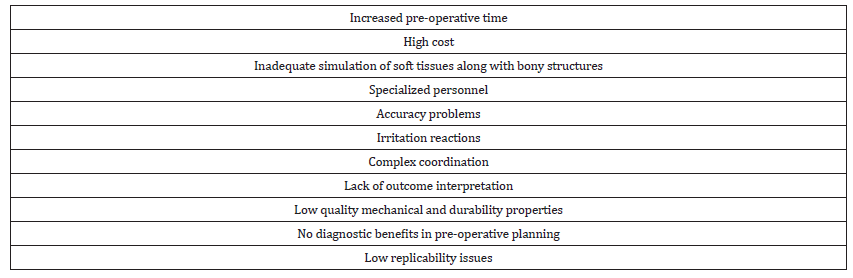
In addition, the current limitations of 3DP technology in simulating soft tissues alongside bony structures prevent adequate resident education and training in this specific area. This limitation hampers the comprehensive understanding of complex anatomical structures involving both bone and soft tissues [28]. Furthermore, the preparation of 3D printed models from 3D software requires specialized personnel, adding complexity to the implementation process and potentially limiting its widespread application [29]. Other reported drawbacks in the literature include accuracy issues, such as deviations between the 3D printed model and the actual patient tissue, as well as potential complications such as irritation reactions (Table 2). Complex coordination, lack of established criteria to define patient outcomes, low quality mechanical properties and durability, limited diagnostic benefits in terms of pre-operative planning, and low replicability issues have also been identified as challenges associated with 3DP in spine surgery [34]. These concerns emphasize the need for further research and development to address the limitations of 3DP technology and refine its application in spine surgery. By addressing these concerns, the full potential of 3DP can be realized, leading to improved patient care and surgical outcomes [28,29].
Conclusions
Being a recent technological advancement, 3DP technology has several applications in spine surgery, facilitating spine surgeons in managing particularly complex spinal disorders that are associated with numerous risks and complications when performed using conventional techniques. Although its application has expanded considerably, the associated pitfalls and concerns, including the need for experienced personnel, high equipment costs, and time-consuming problems, have not yet allowed for its universal adoption among the medical community.
References
- Wong TM, Jin J, Lau TW (2017) The use of three-dimensional printing technology in orthopedic surgery. J Orthop Surg 25(1): 2309499016684077.
- Mulford JS, Babazadeh S, Mackay N (2016) Three-dimensional printing in orthopaedic surgery: review of current and future applications. ANZ J Surg 86(9): 648-653.
- Gadia A, Shah K, Nene A (2018) Emergence of Three-Dimensional Printing Technology, and Its Utility in Spine Surgery. Asian Spine J 12(2): 365-371.
- Eltorai AE, Nguyen E, Daniels AH (2015) Three-Dimensional Printing in Orthopedic Surgery. Orthopedics 38(11): 684-687.
- Anderson PA (2017) Clinical Applications of 3D Printing. Spine 1;42 Suppl 7: S30-S31.
- Hoang D, Perrault D, Stevanovic M, Ghiassi A (2016) Surgical applications of three-dimensional printing: a review of the current literature & how to get started. Ann Transl Med 4(23): 456.
- Javaid M, Haleem A (2018) Additive manufacturing applications in orthopedics: A review. J Clin Orthop Trauma 9(3): 202-206.
- Cho W, Job AV, Chen J, Baek JH (2018) A Review of Current Clinical Applications of Three-Dimensional Printing in Spine Surgery. Asian Spine J 12(1): 171-177.
- Cai H, Liu Z, Wei F, Yu M, Xu N, et al. (2018) 3D Printing in Spine Surgery. Adv Exp Med Biol 1093: 345-359.
- Senkoylu A, Daldal I, Cetinkaya M (2020) 3D printing and spine surgery. J Orthop Surg 28(2): 2309499020927081.
- Tong Y, Kaplan DJ, Spivak JM, Bendo JA (2020) Three-dimensional printing in spine surgery: a review of current applications. Spine J 20(6): 833-846.
- Skelley NW, Smith MJ, Ma R, Cook JL (2019) Three-dimensional Printing Technology in Orthopaedics. J Am Acad Orthop Surg 27(24): 918-925.
- Wong KC (2016) 3D-printed patient-specific applications in orthopedics. Orthop Res Rev 8: 57-66.
- Mok SW, Nizak R, Fu SC (2016) From the printer: Potential of three-dimensional printing for orthopaedic applications. J Orthop Translat 6: 42-49.
- Bagaria V, Bhansali R, Pawar P (2018) 3D printing- creating a blueprint for the future of orthopedics: Current concept review and the road ahead. J Clin Orthop Trauma 9(3): 207-212.
- Dhawan A, Kennedy PM, Rizk EB, Ozbolat IT (2019) Three-dimensional Bioprinting for Bone and Cartilage Restoration in Orthopaedic Surgery. J Am Acad Orthop Surg 27(5): e215-e226.
- Vaishya R, Vaish A (2019) 3D Printing in Orthopedics. Iyer K, Khan W (Eds.), General Principles of Orthopedics and Trauma. Springer, Cham.
- Mumith A, Thomas M, Shah Z, Coathup M, Blunn G (2018) Additive manufacturing: current concepts, future trends. Bone Joint J 100-B (4): 455-460.
- Provaggi E, Leong JJH, Kalaskar DM (2018) Applications of 3D printing in the management of severe spinal conditions. Proc Inst Mech Eng H 231(6): 471-486.
- Sheha ED, Gandhi SD, Colman MW (2019) 3D printing in spine surgery. Ann Transl Med 7(Suppl 5): S164.
- Yamaguchi JT, Hsu WK (2019) Three-Dimensional Printing in Minimally Invasive Spine Surgery. Curr Rev Musculoskelet Med 12(4): 425-435.
- Wu AM, Lin JL, Kwan KYH, Wang XY, Zhao J (2018) 3D-printing techniques in spine surgery: the prospects and current challenges. Expert Rev Med Devices 15(6): 399-401.
- Parr WCH, Burnard JL, Wilson PJ, Mobbs RJ (2019) 3D printed anatomical (bio)models in spine surgery: clinical benefits and value to health care providers. J Spine Surg 5(4):549-560.
- Thayaparan GK, Owbridge MG, Linden M, Thompson RG, Lewis PM, et al. (2020) Measuring the performance of patient-specific solutions for minimally invasive transforaminal lumbar interbody fusion surgery. J Clin Neurosci 71: 43-50.
- Bohl MA, McBryan S, Pais D (2020) The Living Spine Model: A Biomimetic Surgical Training and Education Tool. Oper Neurosurg 19(1): 98-106.
- Lopez CD, Boddapati V, Lee NJ (2021) Three-Dimensional Printing for Preoperative Planning and Pedicle Screw Placement in Adult Spinal Deformity: A Systematic Review. Global Spine J 11(6): 936-949.
- Wilcox B, Mobbs RJ, Wu AM, Phan K (2017) Systematic review of 3D printing in spinal surgery: the current state of play. J Spine Surg 3(3): 433-443.
- Garg B, Mehta N (2018) Current status of 3D printing in spine surgery. J Clin Orthop Trauma 9(3): 218-225.
- Hsu MR, Haleem MS, Hsu W (2018) 3D Printing Applications in Minimally Invasive Spine Surgery. Minim Invasive Surg 2018: 4760769.
- Zhang M, Li J, Fang T (2020) Evaluation of a Three-Dimensional Printed Guide and a Polyoxymethylene Thermoplastic Regulator for Percutaneous Pedicle Screw Fixation in Patients with Thoracolumbar Fracture. Med Sci Monit 26: e920578.
- Yu C, Ou Y, Xie C, Zhang Y, Wei J, et al. (2020) Pedicle screw placement in spinal neurosurgery using a 3D-printed drill guide template: a systematic review and meta-analysis. J Orthop Surg Res 15(1): 1.
- Patel V, Kovalsky D, Meyer SC (2020) Prospective Trial of Sacroiliac Joint Fusion Using 3D-Printed Triangular Titanium Implants. Med Devices 13: 173-182.
- Zhuang H, Wei F, Jiang L, Wang Y, Liu Z (2020) Assessment of Spinal Tumor Treatment Using Implanted 3D-Printed Vertebral Bodies with Robotic Stereotactic Radiotherapy. Innovation (N Y) 1(2): 100040.
- Martelli N, Serrano C, van den Brink H (2016) Advantages and disadvantages of 3-dimensional printing in surgery: A systematic review. Surgery 159(6): 1485-1500.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...

.png)