Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6679
Research Article(ISSN: 2637-6679) 
Construction and Application of the Continuous Knowledge- Attitude-Practice Model for Spinal Cord Injury Patients with Neurogenic Bladder: A Randomized Controlled Trial Volume 8 - Issue 3
Zun cheng Zheng1,2*, Chunyan Zhu3, Xiuzhen Cao4, Mingjing Yang5, Yuexia Chen6, Haoyue Chen7, Jing Li8, Xiaoyu Wang1, Ronghui Zhai2
- 1Department of Rehabilitation, Taian City Central Hospital, China
- 2Department of Nursing, Taian City Central Hospital, China
- 3Master, Department of Rehabilitation, Taian City Central Hospital, China
- 4Master, Department of Anorectal surgery, Taian City Central Hospital, China
- 5Master, Department of Rehabilitation, Taian City Central Hospital, China
- 6Bachelor, Skills Training Base, Taian City Central Hospital, China
- 7Master, Department of Rehabilitation, Taian City Central Hospital, China
- 8Master, Nursing Quality Management Section, Taian City Central Hospital, China
Received: July 21, 2023; Published: July 26, 2023
Corresponding author: Zun cheng Zheng, Department of Rehabilitation, Taian City Central Hospital, China.
DOI: 10.32474/RRHOAJ.2023.08.000289
Abstract
Objective: The purpose of this study was to construct a neurogenic bladder continuous knowledge-attitude-practice management model that starts from the shock phase of spinal cord injury, and to observe the clinical application effect of this model.
Design: This research was conducted as a single-center, single-blind, randomized controlled study
Participants: A total of 60 patients with neurogenic bladder dysfunction were randomly assigned into either test group (n = 30) or the control group (n = 30).
Methods: The Delphi method was used to establish “the neurogenic bladder continuous knowledge-attitude-practice management model”. The control group was treated with conventional drinking plan + intermittent catheterization + medication and conventional education model, while the test group was treated according to the knowledge-attitude-practice management model. Data were collected at the early admission, late spinal shock, the inpatient rehabilitation period, and discharge follow-up period. The two groups were compared with self-cleaning intermittent catheterization knowledge-attitude-practice questionnaire scores, pelvic floor muscle surface electromyography evaluation, urodynamic evaluation, and autonomous bladder indexes.
Results: After the intervention, the neurogenic bladder patients in the test group self-cleaning intermittent catheterization behavioral questionnaire scores, pelvic floor muscle surface electromyography assessment, urodynamic evaluation indicators (bladder safe volume, residual urine volume, bladder compliance) were higher than those of the control group, The first reflex urination time and the establishment time of autonomous bladder are earlier than those of the control group (P<0.05).
Conclusions: The continuous knowledge-attitude-practice management model provides patients with a lifelong spinal cord injury management program. Help patients to achieve self-management from the management of medical and nursing compliance, maximize the recovery of the patient’s bladder function, rebuild the autonomous bladder.
Registration number: ChiCTR2100049574
Tweetable abstract: an optional additional 140-character message that can be ‘tweeted.’
What is already known?
a) The incidence of neurogenic bladder after spinal cord injury is high and affects patients’ quality of life and survival.
b) Intermittent catheterization is the preferred method for neurogenic bladder, but due to the lack of self-care knowledge and ability, the performance of intermittent catheterization after discharge is poor.
c) The importance of neurogenic bladder rehabilitation training has been paid much attention to, but the late start of the training and the insufficient continuous training after discharge lead to the poor effect.
What this paper adds
a) This study established a knowledge-attitude-practice management model for neurogenic bladder after spinal cord injury.
b) It emphasizes the role of patients from the beginning of admission.
c) Emphasis on early intervention and whole-process management.
d) Combine nursing and rehabilitation, emphasizing that intermittent catheterization is not only a replacement mode of urination but also a bladder training mode.
Keywords: Spinal cord injury; neurogenic bladder; intermittent catheterization; knowledge-attitude-practice; behavior management
Introduction
The prevalence of spinal cord injury worldwide is about 236 to 1009 per million, with 10 to 83 new cases per million per year [1]. Bladder urethral voiding dysfunction and urine storage dysfunction after spinal cord injury is also called neurogenic bladder. It has been reported that the incidence of neurogenic bladder after spinal cord injury is as high as 90% [2]. Renal failure caused by neurogenic bladder is a common serious complication after spinal cord injury [3], which is the first cause of death in patients with SCI [4]. Intermittent catheterization is currently considered as the “gold standard” for the treatment of neurogenic bladder [5,6] and is the preferred method for bladder management in spinal cord injury patients [7]. Although intermittent catheterization has helped restore bladder function in many patients with neurogenic bladder in recent years, about 19% of patients still need catheterization for life [8]. However, some scholars found that the failure of intermittent catheterization after discharge was as high as 50% due to irregular intermittent catheterization after 5 years of follow-up [9]. The reasons for failure of intermittent catheterization include poor patient compliance, lack of a comprehensive follow-up mechanism in hospitals, and lack of effective technical support for chronic disease management in the community. At present, institutional rehabilitation and community rehabilitation of spinal cord injury in China are both in the initial stage [10], and it is difficult for most patients to get the opportunity of systematic rehabilitation after discharge [11], which cannot meet the needs of patients.
To improve the success rate of long-term bladder management and guide patients to gradually transition from medical compliance management to patient-based self-management, we introduced the theory of knowledge-attitude-practice management. The theory is about behavior change that individual behavior changes can be divided into three processes: knowledge acquisition, belief generation, and behavior formation. Patients have acquired knowledge and methods of neurogenic bladder management, can establish correct beliefs about bladder management, form an overall understanding of the bladder, reasonable expectations, and positive attitudes, and are ultimately willing to actively implement bladder management program. To achieve effective bladder selfmanagement. At the same time, guided by the theory of continuous of care, we then established a continuous knowledge-attitudepractice management model for neurogenic bladder, and provided patients with a lifelong neurogenic bladder management program to maximize self-management ability, improve urination and urinary control ability, and ensure bladder safety.
Methods
Construction of the continuous behavior management model of knowledge-attitude-practice in neurogenic bladder with spinal cord injury
Establishment of a spinal cord injury neurogenic bladder management team
It is composed of 5 rehabilitation doctors, 5 rehabilitation nurses, 2 physiotherapists, 2 occupational therapists, 1 psychotherapist and patients, including 3 senior professional titles, 7 intermediate professional titles, and 5 junior professional titles personnel. One chief physician is the team leader and is responsible for the whole planning; Five junior professional titles personnel are responsible for consulting literature, collecting, and sorting out data, and other personnel are responsible for discussing and determining items, preparing expert consultation questionnaires. And organize, analyze, discuss and modify the results and opinions put forward by experts.
Establishment of the first draft of the continuous knowledge-attitude-practice management plan
According to the guidelines and the theory of knowledgeattitude- practice, the initial item of the plan is determined by searching the database both Chinese and foreign literature. The searched English databases include PubMed, Web of Science, the Cochrane Library. Key words include spinal cord injury, neurogenic bladder, behavior management of knowledge-attitude-practice. The searched Chinese databases include CNKI, Wan fang, VIP. Keywords include spinal cord injury, neurogenic bladder, knowledge-attitudepractice management, Search the literature of the past five years, summarize, and sort them, and finally form a letter of inquiry. The content includes three intervention periods: spinal shock period, inpatient rehabilitation period, and discharge follow-up period. A total of 52 items were included, including 27 items for knowledge, 7 items for belief, and 18 items for behavior.
Design expert consultation questionnaire
The expert consultation questionnaire includes:
a. Expert invitation letter.
b. Expert general situation survey form.
c. The main part of the scale is composed of items and their scores; Experts are asked to use the Likert 5-level scoring method to make judgments based on the importance of the items. From “very unimportant” to “very important”, 1 to 5 points are counted. Each item is left with blank columns and remarks for experts to fill in their comments.
d. Experts’ familiarity with the field and the basis for judgment.
Selection of experts for consultation
a) A total of 15 experts from 8 tertiary general hospitals in my country were selected as the subjects of consultation. Inclusion criteria:
b) Work in relevant departments (such as rehabilitation, urology, orthopedics) for 10 years or more, and have accumulated rich practical experience in the field of spinal cord injury.
bachelor’s degree or above.
c) Intermediate and above professional titles.
d) Pay attention to and actively participate in this research.
Letter inquiry
According to the experts, we will issue paper questionnaires and e-mails for letter inquiries, collect the first round of letter questionnaires, sort out and analyze expert opinions, and determine the second round of letter questionnaires. In this study, a total of 2 rounds of letter inquiries were conducted, with an interval of 2 months, and expert opinions tended to be consistent. In the first round of expert consultation, a total of 15 questionnaires were issued and 13 valid questionnaires were returned. The effective response rate was 86.7%. In the second round, experts issued 15 questionnaires and recovered 14 valid questionnaires. The effective response rate was 93.3%. Experts are highly motivated; The expert authority coefficients of the two rounds were 0.877 and 0.883 respectively, both> 0.7. Prompt experts to have a high degree of authority and reliable consultation results. According to project selection criteria (project retention criteria: importance score ≥ 3.5 points, and coefficient of variation <0.25) [12]. At the same time, in accordance with expert suggestions, the items should be modified, deleted, or added after discussion by the team members.
Determination of the final plan
After 2 rounds of consultation, a continuous knowledgeattitude- practice management plan for spinal cord injury patients with neurogenic bladder is finally formed. Including three intervention periods: spinal shock period, inpatient rehabilitation period, and discharge follow-up period. A total of 49 items were included, including 25 items for knowledge, 6 items for attitude, and 18 items for practice (supplementary material 1).
Clinical application of the continuous knowledge-attitude- practice management model in neurogenic bladder with spinal cord injury
Design
The research was conducted as a single-center, single-blind, randomized controlled study from January 2019 to December 2020 at rehabilitation medicine department of a tertiary hospital in Tai’an City, Shandong Province, China.
Study participants
A total of 60 patients with spinal cord injury and neurogenic bladder dysfunction who were admitted to the rehabilitation medicine department of a Third-class A hospital in Tai’an City, Shandong Province from January 2019 to December 2020 were selected as the research objects. The random number table was used as a simple randomization method to recruit patients into the test and control groups.
a) Inclusion criteria: ①18-75 years old, normal intelligence and language skills, able to cooperate in the evaluation questionnaire; ②Meet the spinal cord injury diagnostic criteria of MRI, and the spinal cord is not completely detached. Meets International Continence Society diagnostic criteria for neurogenic bladder. ③Patients with incomplete spinal cord injury above sacral and urinary dysfunction after acute spinal cord injury; ④Admission to the hospital at the shock stage of spinal cord injury. ⑤ It has good tolerance to the urine volume measurement and urine routine inspection methods required for this study; ⑥ the patient’s condition is stable and does not need rescue or monitoring treatment; ⑦ No organic urinary tract obstruction, urinary calculi, no metal implants near the bladder, and no pacemaker.
b) Exclusion criteria: ①Patients with long-term intravenous fluid infusion unable to control urine output per unit time; ②Patients requiring long-term indwelling catheterization for disease reasons ③Patients or their family members unable to complete intermittent urinary catheterization ④Combined with serious complications, such as severe heart and kidney, Diabetes patients; ⑤Patients who are unwilling to cooperate with the trial.
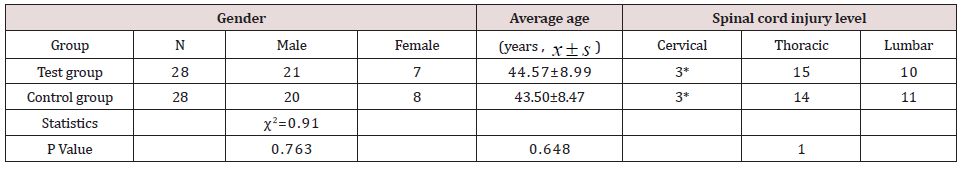
During the intervention, two patients in the control group were lost to follow-up. one patient was stopped because of other complications and one patient was lost to follow-up in the test group. A total of 4 patients were lost. The general information of the two groups is shown in Table 1.
Table 1. Comparison of general information of the two groups of patients (n=56) *The expected values of the cells were < 5, Fisher’s exact test was performed, and the results showed that P=1.000.
Intervention
Control group intervention methods
The control group received indwelling catheterization during spinal shock. After the shock period, the control group was given regular intermittent catheterization. The drinking plan was developed according to the drinking habits of the patients, and the water was regularly quantified; Ensure that the urine output is controlled at 1500-2000ml, with intermittent catheterization 4-6 times a day. Meanwhile, bladder function training and other rehabilitation measures were given. The neurogenic bladder knowledge should be publicized, and the emergency response, urine volume imbalance and urinary tract infection should be treated in time.
Test group Intervention methods
After the patients in the test group had stabilized during the spinal shock stage, the catheter was removed within 48 hours and then intermittent catheterization was performed. According to the behavior management plan, which has been inquired by experts, Intervention was carried out in the three rehabilitation periods of spinal cord injury, spinal cord shock, inpatient rehabilitation, and discharge follow-up period.
Evaluation Index
Timing of evaluation
a) Early admission (spinal shock period): complete the first evaluation within 3 days after admission.
b) Late spinal shock: the appearance of the bulbocavernosus reflex is the sign of the end of the shock period, and the second evaluation is given after the end of the shock period.
c) Inpatient rehabilitation:three months after admission to the hospital.
d) Discharge follow-up:six months after discharge. Measurement indicators:
a) The Clean Intermittent Self-Catheterization of Knowledge-Attitude-Practice Scale for patients with neurogenic bladder
The Clean Intermittent Self-Catheterization of Knowledge- Attitude-Practice Scale of patients with neurogenic bladder compiled by Chen Ling in 2021 [13] (Supplementary material 2). The Cronbach’sα coefficient of the scale reliability test is 0.937, and the content validity is 0.927. The scale Includes 3 dimensions: 7 items for knowledge, 6 items for attitude and 6 items for behavior, 19 items in total. Likert1-5 rating (1 = highly unlikely, 2 = unlikely, 3 = indeterminate, 4 = likely, 5 = highly likely) was used for scoring, the total score of 19 items is 95 points. A higher score indicates a higher compliance with neurogenic bladder self-management.
b) Evaluation of pelvic floor muscle surface electromyography
The pelvic floor surface electromyography assessment (Glazer assessment [14]is divided into 5 stages: the pre-rest stage (myoelectric value in the resting state), the rapid contraction stage (mainly represents the muscle strength of the type II muscle fibers, rapid contraction for 5 times, relax for 10 seconds before each contraction, assess the basin Bottom fast muscle function, the reference value is 35-45 μV), tension contraction stage (mainly represents the coordination function of type Ⅰ and Ⅱ muscle fibers, continuous contraction and relaxation for 5 times, contraction for 10 seconds, relaxation for 10 seconds, mainly to assess slow muscle strength, the reference value is 30-40μV), endurance contraction stage (mainly represents type I muscle fiber strength, endurance contraction for 60s, evaluation of pelvic floor slow muscle endurance, the reference value is 25-35 μV), and the post-rest period (muscles after endurance contraction).
c) The basic collection table of the international database of spinal cord injury urodynamics index
The indexes were selected from International Standards for Autonomic Nervous Remaining After Spinal Cord Injury [15]. In this study, according to Appendix II ‘International Spinal Cord Injury Urodynamic Basic Data Set Form’, three aspects of bladder volume, residual urine volume and bladder compliance were collected during urodynamic examination.
d) Autonomous bladder establishment indexes
The criteria for autonomous bladder establishment are: The bladder can store urine at low pressure and has a larger bladder capacity; Can empty the bladder autonomously and regularly without a urinary tube (residual urine volume ≤ 20% of the bladder volume or <100 ml); The interval between two urinations can be 2.5-4h, the number of leaks per day is less than 3 times, and the upper urinary tract function is not impaired.
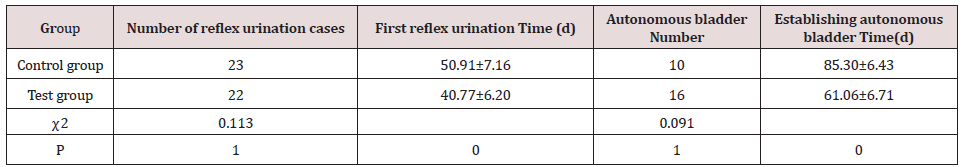
Evaluation index: the number of reflex urination cases, the time of first reflex urination, autonomous bladder number and the time of establishing autonomous bladder.
Statistical methods
The data was analyzed using SPSS 20.0 (SPSS Inc., Chicago, IL, USA) software. The characteristics of the test and control groups were described using descriptive statistics. The independent group t-test for continuous variables and a chi-square test for categorical variables were utilized to compare the two groups for all baseline variables. Two-way repeated-measures analysis of variance (ANOVA) was applied to assess differences in repeated measures at different time points. P values less than 0.05 were considered statistically significant via two-tailed tests.
Ethical considerations
This study was reviewed and approved by the ethics committee of the hospital (NO.2019-05-26). Test registration number ChiCTR2100049574. The purpose of the research was explained to the participants. A written letter of consent was also obtained from the research participants.
Comparison of the two groups at baseline
The distribution of the test and control groups’ individual and spinal cord injury level are presented in Table 1. There were no statistically significant differences between the two groups.
Comparison of the Clean Intermittent Self-Catheterization of Knowledge-Attitude-Practice Scale
Table 2. The scores comparison of the Clean Intermittent Self-Catheterization of Knowledge-Attitude-Practice Scale.
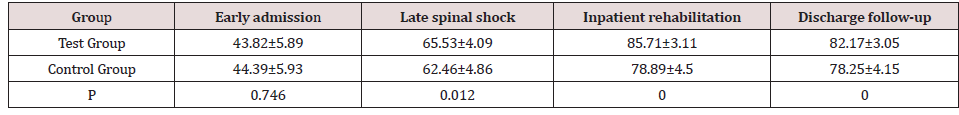
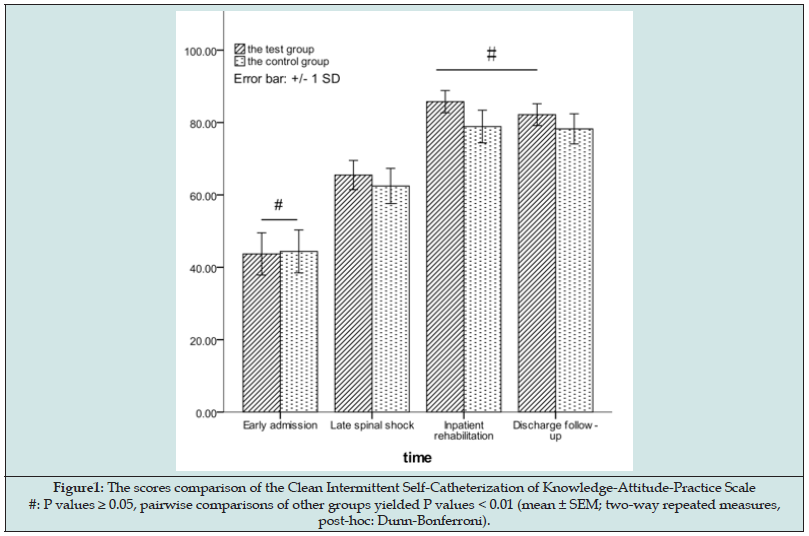
With the progress of treatment, the Clean Intermittent Self- Catheterization of Knowledge-Attitude-Practice Scale of the subjects gradually increased, and pairwise comparisons within the test group showed statistical significance. (P = 0.000). In the control group, the scale score gradually increased during hospitalization, and the intra-group comparison showed a statistical difference (P=0.000). The score of patients after discharge decreased compared with that during hospitalization, but the difference did not reach a statistical difference (P=0.000). In the comparison between the control group and the test group, there was no statistical difference at the early admission (P=0.746). The other pairwise comparison results showed that there were significant differences (P<0.05) (Table 2).
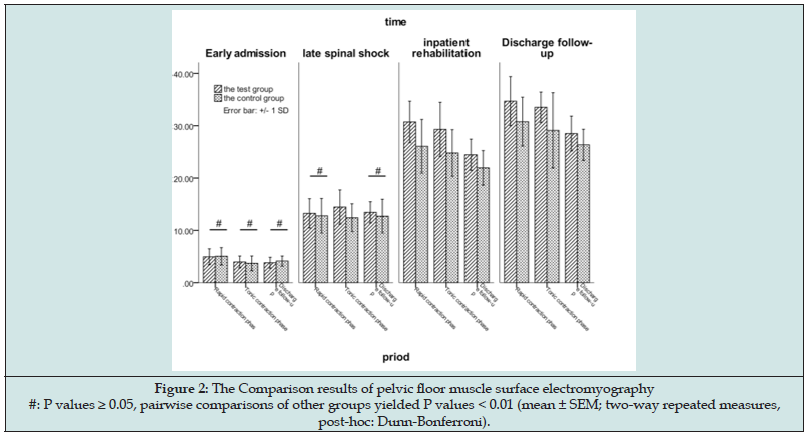
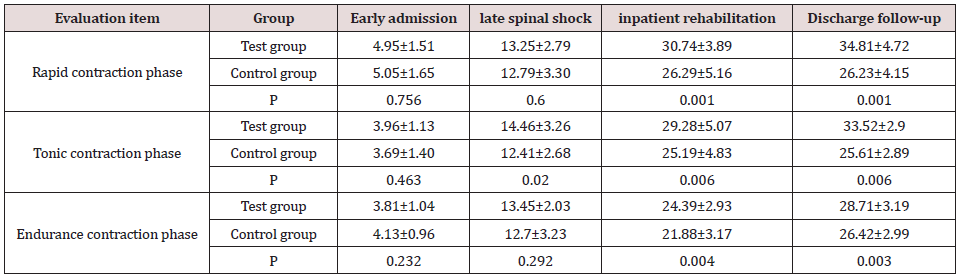
Results of pelvic floor muscle surface electromyography evaluation
The two groups were compared in the three stages of rapid contraction, tension contraction, and endurance contraction. Intra-group comparison showed that pelvic floor muscle strength increased gradually in two groups, and the differences in each period were statistically significant(P<0.01). The comparison between the control group and the experimental group showed that there was a significant difference in the tension-contractile phase at the end of spinal shock (P=0.020) and there were no other statistical differences in the three monitoring stages in the early admission period and the end of spinal shock stage (P> 0.05). In the two periods of inpatient rehabilitation and discharge followup, the test group was significantly better than the control group in all three stages, and the comparison was significantly different (P<0.01). (Table 3 and Figures 1 & 2).
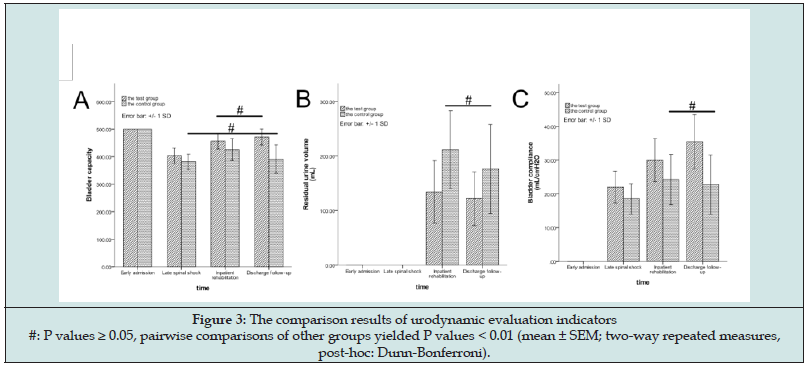
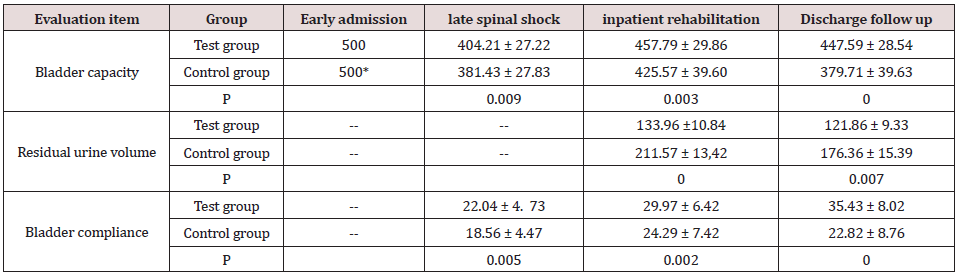
Collection of urodynamic evaluation indicators
In the control group, the comparison of the bladder capacity and bladder compliance between the late spinal shock period and the discharge follow-up period showed no statistical significance (P=1.000), and the other pairwise comparisons showed statistical significance. The residual ruined volume of the control group between inpatient rehabilitation period and follow-up was statistically different (P=0.000). The comparison of bladder compliance between the late spinal shock period and the discharge follow-up period showed no statistical differences (P=0.250), the other pairwise comparisons showed statistical significance.
In the test group, the comparison of bladder capacity and residual urine volume between the inpatient rehabilitation and the discharge follow-up period was no statistical difference (P=0.250, P=0.122); and the rest pairwise comparisons of the evaluation indicators were significant differences (P<0.01). The comparison between the control group and the test group showed that there were statistically significant differences in bladder volume, bladder compliance and bladder residual urine volume in all phases. (Table 4, Figure 3).
Table 4. Urodynamic evaluation indicators *At the early stage of admission, there was no spontaneous bladder contraction due to spinal shock. To ensure the safety of patients, urodynamics examination was stopped when perfusion reached 500ml. So, bladder volume and residual urine volume were not recorded, and bladder compliance was not calculated.
The result of autonomic bladder formation index
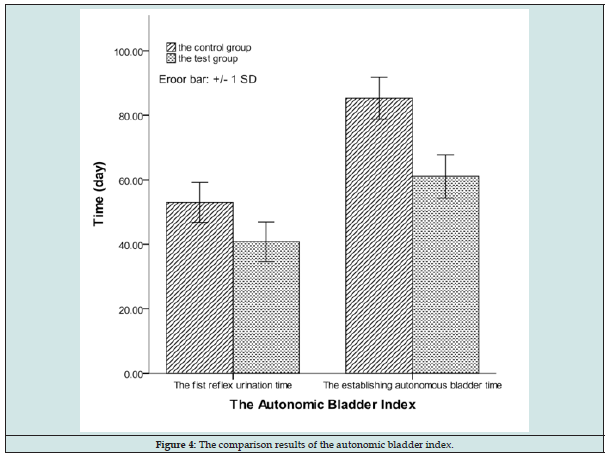
As shown in Table 5, there is little difference in the number of reflex voiding cases between the test group and the control group after the intervention, while the first reflex voiding time in the test group is shorter than that in the control group (P<0.01).The number of cases in which autonomous bladders were established in the test group was more than that in the control group, and the time to establish the autonomous bladder was significantly shorter than that in the control group (P<0.01).(Table 5, Figure 4).
Discussion
In this study, the continuous knowledge-attitude-practice management model was applied to patients of SCI with neurogenic bladder. The results showed that after the intervention, the test group had CISC-KAPS scores and pelvic floor s EMG evaluation, urodynamic evaluation indicators (bladder volume, residual urine volume, bladder compliance), the time of reflex urination, and the time of autonomous bladder establishment were better than those of the control group. The continuous knowledge-attitude-practice management model provides patients with a lifelong spinal cord injury management program and maximizes the recovery of the patient’s bladder function.
The comprehensive rehabilitation treatment of neurogenic bladder has been a hot spot in recent years. In the process of rehabilitation, reconstruction of the autonomous bladder and improvement of urinary control are the main means to extend the life expectancy and improve the quality of life of patients with SCI. It is of great significance to reduce the fatality rate. The rehabilitation of neurogenic bladder is a long-term and complex process that requires patients and their families to have good compliance, active participation, dynamic management, and lifelong management16. In view of the characteristics of neurogenic bladder rehabilitation, this study designed a targeted continuous knowledge-attitudepractice model, which has three characteristics: 1. It emphasizes the role of patients from the beginning of admission, and gradually transitions from the joint participation of doctors and patients to the self-care of patients as the center. 2. Emphasis on early intervention and whole-process management. Early (shock stage) knowledge-attitude-practice management is conducive to the recovery of bladder function, and long-term (post-discharge) selfmanagement is conducive to the prognosis of bladder function, so the intervention throughout the whole process can ensure the bladder safety of patients. 3. Combine nursing and rehabilitation, emphasizing that intermittent catheterization is not only a replacement mode of urination but also a bladder training mode, and emphasizing the influence of bladder training on prognosis.
The influence of knowledge-attitude-practice management on self-management compliance of patients
The premise of neurogenic bladder management and intermittent catheterization requires higher compliance from patients and their families. Studies have pointed out that patient behavioral compliance is directly related to the quality of bladder management [16]. So, it is necessary to consider intermittent catheterization as an important therapeutic measure and implement all measures carefully. During the different stages of bladder rehabilitation, various problems may arise due to behavioral compliance that lead to the inability to restore bladder function. The Clean-Intermittent Self-Catheterization of Knowledge-Attitude-Practice Scale is designed to evaluate the patient’s knowledge and application of intermittent catheterization at different stages of the disease and to guide the implementation of the neurogenic bladder management plan for patients. In the control group, bladder management and health education during inpatient rehabilitation are effective for patients’ compliance. However, due to lack of continuous education and supervision after discharge, the neurogenic bladder self-management ability has a downward trend. In contrast, the results of the test group showed that it can maintain good self-behavior management compliance from admission to follow-up.
The continuous nursing intervention under the theory of knowledge-attitude-practice is different from the traditional nursing model. It pays more attention to patients’ acquisition of neurogenic bladder management knowledge and methods at different stages of the disease and enables patients to establish correct attitude in bladder management. Through individual interventions at different stages, the bladder management program was proactively implemented to improve the living behavior of the patients, so that the patients could eventually become neurogenic bladder selfmanagement experts and improve the compliance of the behavior management of patients with intermittent catheterization.
Effect of early-ongoing continued behavior management on bladder function in patients with spinal cord injury
The results of Table 4 & 5 of this study show that the continuous behavior management carried out during the spinal shock period has a significant effect on improving the bladder function of patients. After the intervention, the bladder function of the test group was better than that of the control group at all stages. The control group received standardized treatment and management of bladder function during hospitalization, and bladder function recovered, but due to lack of continuous supervision after discharge, bladder capacity and compliance began to show a tendency toward spastic bladder. The improvement of the test group was significantly better than that of the control group in each stage, and the good bladder management effect could be maintained in the follow-up period after discharge.
Guidelines recommend that intermittent catheterization should be performed within 48 hours after vital signs stabilized in spinal cord injury patients with urination dysfunction if there are no contraindications for intermittent catheterization [11]. The natural recovery period is 1-3 months after the onset of injury, but the changes of neuroplasticity can occur as early as 3 days after the onset, so early neuroplasticity training is more important [17]. Early and correct intermittent catheterization is an effective rehabilitation training mode for the formation of “autonomous bladder”. In this mode, reinforcing remodeling by behavior management, intermittent catheterization as early as possible makes it easier to form an autonomous bladder.
The behavior management of knowledge-attitude-practice is a guide to improve the patient’s ability to perform, so that the patient can correctly perform intermittent catheterization and regularly empty the bladder. It is essential to implement effective bladder function training, which can make the bladder close to the normal state of diastole and contraction, maintain the safe volume of the bladder, reduce the residual urine volume of the bladder, increase the compliance of the bladder, protect the kidney function, reduce the occurrence of complications, and be beneficial to the recovery of bladder function.
The effect of continuous behavior management on pelvic floor function in patients with neurogenic bladder
Urination and storage disorders of neurogenic bladder are related to the coordination function of the detrusor and sphincter of the bladder itself. The regular contraction and support ability of the pelvic floor muscles and urethral sphincter are important factors for urination and storage [18]. The pelvic floor surface EMG can not only effectively evaluate the bladder muscle strength by recording the potential changes of the pelvic floor and urethral muscles, but also can be combined with other bladder function training methods for the pelvic floor muscle training. Cai Wenzhi [19,20] recommended that bladder function training is an effective way to promote neurogenic bladder function recovery, while bladder training alone is relatively boring, and patients are not highly involved, so that they have poor compliance and low acceptance, and often give up halfway. In this study, combined training of pelvic floor muscles, such as respiratory function training, pelvic floor electrical stimulation, and pelvic floor muscle manipulation, was used for bladder function rehabilitation training. Because this type of training requires patients to exercise for a long time, if they cannot persist in training, it will reduce the effect of treatment and increase the occurrence of adverse reactions such as urinary incontinence and defecation disorders. so, the patient’s adherence to treatment effect is very important.
The results of this study showed that the pelvic floor muscle function of patients in the two groups improved after rehabilitation training. Compared with the control group, the improvement was more obvious in the test group. Due to complete denervation of pelvic floor muscles during spinal shock, there was no significant difference between the two groups at the beginning of admission and the end of spinal shock. However, after behavioral management intervention during inpatient rehabilitation and discharge followup, the contractile ability of pelvic floor muscles in the experimental group was significantly better than that in the control group at three contractile stages (P<0.01). It showed that the patient’s urinary control ability and urinary leakage were better than those of the control group.
The implementation of our continuous knowledge-attitudepractice management program has greatly improved the compliance of patients with long-term bladder training. And through Kegel functional training and strong abdominal breathing, the levator ani muscles are trained for voluntary contraction and relaxation. Through repeated rhythmic independent exercise, not only can enhance the coordination of urethral sphincter, strengthen the strength and control of pelvic floor muscles, detrusor muscles and urethral sphincter, but also can improve the ligament tension of bladder, uterus, and other parts, so as to realize the recovery of pelvic floor function [21,22].
Conclusions
The establishment of the continuous knowledge-attitudepractice management plan provides a lifelong management program for spinal cord injury patients with neurogenic bladder, which can transform the management from the nurse-patient cooperation to self-behavior management. The application of this management mode can maximize the recovery of bladder function, improve the quality of life of patients, and accumulate experience and practical basis for the nationwide promotion of neurogenic bladder management after spinal cord injury.
References
- Romo PGB, Smith CP, Cox A, Averbeck MA, Dowling C, et al. (2018) non-surgical urologic management of neurogenic bladder after spinal cord injury. World J Urol 36(10): 1555-1568.
- Sripathi V, Mitra A (2017) Management of Neurogenic Bladder. Indian J Pediatr 84 (7): 545-554.
- Nseyo U, Santiago Lastra Y (2017) Long-Term Complications of the Neurogenic Bladder. Urol Clin North Am 44(3): 355-366.
- Hamid R, Averbeck MA, Chiang H, Garcia A, Al Mousa RT, et al. (2018) Epidemiology and pathophysiology of neurogenic bladder after spinal cord injury. World J Urol 36(10): 1517-1527.
- Tate DG, Wheeler T, Lane GI, Forchheimer M, Anderson KD, et al. (2020) Recommendations for evaluation of neurogenic bladder and bowel dysfunction after spinal cord injury and/or disease. J Spinal Cord Med 43(2): 141-164.
- Bragge P, Guy S, Boulet M, Ghafoori E, Goodwin, et al. (2019) A systematic review of the content and quality of clinical practice guidelines for management of the neurogenic bladder following spinal cord injury. Spinal Cord 57(7): 540-549.
- Groen J, Pannek J, Castro Diaz D, Del Popolo G, Gross, et al. (2016) Summary of European Association of Urology (EAU) Guidelines on Neuro-Urology. Eur Urol 69(2): 324-333.
- Craig A, Nicholson Perry K, Guest R, Tran Y, Dezarnaulds A, et al. (2015) study of the occurrence of psychological disorders and comorbidities after spinal cord injury. Arch Phys Med Rehabil 96(8): 1426-34.
- Zlatev DV, Shem K, Elliott CS (2016) How many spinal cord injury patients can catheterize their own bladder? The epidemiology of upper extremity function as it affects bladder management. Spinal Cord 54(4): 287-291.
- Mingliang Y, Jianjun L, Qiang L, Zhuoying Q, Chao C, et al. (2012) Clinic and Rehabilitation Pathway Recommendation for Spine and Spinal Cord Injury. Chin J Rehabil Theory Pract 18(8): 791-796.
- Kinnear N, Barnet D, O Callaghan M, Horsell K, Gani J, et al. (2020) The impact of catheter-based bladder drainage method on urinary tract infection risk in spinal cord injury and neurogenic bladder: A systematic review. Neurourol Urodyn 39(2): 854-862.
- Le Breton F, Guinet A, Verollet D, Jousse M, Amarenco G (2012) Therapeutic education and intermittent self-catheterization: recommendations for an educational program and a literature review. Ann Phys Rehabil Med 55(3): 201-212.
- CHEN Ling HY, CHEN Xiaomin, ZHANG Yan, WANG Laifu, CAI Wenzhi, (2021) Compilation and reliability and validity test of Clean Intermittent Self⁃Catheterization of Knowledge, Attitude,Practice Scale of patients with neurogenic bladder. Chinese nursing research 2(35): 210-215.
- Glazer HI (2005) Biofeedback vs electrophysiology. Rehab Manag 18(9): 32-34.
- Krassioukov A, Biering Sorensen F, Donovan W, Kennelly M, Kirshblum S, et al. (2012) Autonomic Standards Committee of the American Spinal Injury Association/International Spinal Cord, S., International standards to document remaining autonomic function after spinal cord injury. J Spinal Cord Med 35(4): 201-210.
- Bonniaud V, Lyxuchouky X, Bevalot J, Decavel P, Metton G, et al. (2008) [Inquiry among general practitioners' knowledge regarding clean intermittent self-catheterization]. Ann Readapt Med Phys 51(9): 729-733.
- Dinh A, Davido B, Duran C, Bouchand F, Gaillard JL, et al. (2019) Urinary tract infections in patients with neurogenic bladder. Med Mal Infect 49(7): 495-504.
- Allon EF (2019) The role of neuromuscular electrical stimulation in the rehabilitation of the pelvic floor muscles. Br J Nurs 28(15): 968-974.
- Wenzhi C, Sijing C (2011) Guidelines for Neurogenic Bladder Care (2011 edition) (ii). Chinese Journal of Nursing 46(02): 210-216.
- Wenzhi C, Sijing C (2011) Guidelines for Neurogenic Bladder Care (2011 edition) (i). Chinese Journal of Nursing 46(01): 104-108.
- Richardson DA, Miller KL, Siegel SW, Karram MM, Blackwood NB, et al. (1996) Pelvic floor electrical stimulation: a comparison of daily and every-other-day therapy for genuine stress incontinence. Urology 48(1): 110-118.
- Elmelund M, Biering Sorensen F, Due U, Klarskov N (2018) The effect of pelvic floor muscle training and intravaginal electrical stimulation on urinary incontinence in women with incomplete spinal cord injury: an investigator-blinded parallel randomized clinical trial. Int Urogynecol J 29(11): 1597-1606.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...

.png)