Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6679
Review Article(ISSN: 2637-6679) 
Co-Sleeping: Benefits for Mothers and Infants Volume 6 - Issue 4
Antigoni Sarantaki*
- Department of Midwifery, Faculty of Health & Caring Sciences, University of West Attica, Greece
Received:August 11, 2021 Published: August 31, 2021
Corresponding author:Antigoni Sarantaki PhD, Department of Midwifery, Faculty of Health & Caring Sciences, University of West Attica, Athens, Greece
DOI: 10.32474/RRHOAJ.2021.06.000245
Abstract
Bed sharing is gaining popularity, although the sleeping positions of mothers and infants have been questioned because of reported worries regarding the possibility of infant death. This study aimed to investigate infant sleeping location and the association between co-sleeping and parameters such as breastfeeding, infant–mother attachment, and infant death. A systematic search of five electronic databases (Medline, Cochrane, CINAHL, EMBASE, and Scopus) was undertaken to identify related studies. Additional searches conducted were based on the references of the selected studies. Initially,147 articles were located. Titles and abstracts were examined for relevance to the review objective. Studies that met the inclusion criteria were then evaluated for methodological quality. Our study investigated the existence of a correlation between co-sleeping and breastfeeding, infant–mother attachment, maternal depression, infant sleep patterns, and infant death, as well as the possibility of other associated factors.
Keywords: Co- Sleeping; Bed Sharing; Sleep, Place; Breastfeeding; Location; Infant
Introduction
An increasing percentage of parents are choosing to share their bed with their infants [1]. In the United Kingdom, nearly half of parents share, at some time, their bed with their newborns; a fifth of parents bring their infants to bed frequently during the first year of life [2,3]. In the US, co-sleeping peaks in early childhood and decreases with age [3-6]. Lately, it was reported that 21% of mothers in the US and, in particular, 25% of mothers of Hispanic origin, bed share with their infants [7]. The physiology of infant sleep depends on biological and sociocultural variables [8]. The terms “co-sleeping” and “bed sharing” are often used interchangeably in the medical literature. It is important, however, to understand the differences between the two terms, as they relate to the risks and benefits of infant sleep environments. Co-sleeping is a broad term, encompassing the sharing of any sleep surface (e.g., mats, floors, futons, beds, couches, and sofas) with an infant and another person. Bed sharing, in contrast, is one form of co-sleeping that usually refers to the sharing of beds such as those commonly used in most Western European countries, New Zealand, Australia, and the US.
Worldwide, in many non-western societies, bed sharing is viewed as the culturally acceptable practice for ensuring infant safety and comfortable sleep for both mother and baby [9,10]. Similar to other mammals, human mothers used to sleep closely to their infants throughout human evolution [11]. In western or industrialized societies, there has been an increasing emphasis on individuality and independence, which has resulted to recent practices of solitary sleeping areas for babies, and the use of human milk substitutes [12-14]. There is neurological basis for infants seeking parental contact; moreover, parents are biologically designed to react to their infants’ needs [10,15]. Humans create defenseless babies who need extended maternal care and breastfeeding. This is, in particular, a human infant trait, since they are born with the least neurological maturity and are completely dependent on their caregiver for a longer period compared to other mammals [2]. Bed sharing may assist in calming an upset baby, improving sleep for mothers and babies, and contribute to nighttime breastfeeding [9].
Sudden Infant Death Syndrome (SIDS)
The place of sleep for the mother and the infant has been ambivalent due to reported worries regarding infant deaths [2,16]. Epidemiological studies have observed a strong association with infant sleep position and stressed the need to inform parents about the safety of the supine position [2,17]. Other practices related to infant care, such as the use of a dummy, soft mattress and infant head protective coverings were examined [2]. In a recent study, it was exhibited that SIDS occurred in poor communities [18]; they exhibited increased risk factors as prematurity, low prenatal care, smoking and alcohol use, sleeping position, low likelihood to exclusively breastfeed, and co-sleeping. In this study, medium to high co-sleeping rates were observed in more wealthy groups, but high percentages of infant-mother bed sharing were not related to SIDS [9]. The best manner of resolving safety worries is to provide parents, especially mothers, with excellent knowledge about safe bed sharing [10]. These recommendations include not sleeping on a sofa and sleeping on a flat surface, abstaining from alcohol, drugs or smoking [19]. The risk among infants sharing a bed with a smoker-mother was more than 4-fold (OR = 4.55; 95% CI [2.63– 7.88]), compared to nonsmoking mothers, whom exhibited no risk (OR = 0.98; 95% CI [0.44–2.18]) [20]. Significant correlations have been found between bed sharing and use of alcohol or drugs before sleeping, or co-sleeping in a sofa [21]. Recently, observational casecontrol studies showed that half of SIDS cases took place when infants slept next to parent [22]. This increase of deaths outside the crib, has led some countries to discourage bed sharing, including the American Academy of Pediatrics (AAP) since 2015 [23,24]. In particular, the only instance when SIDS deaths took place, during the last 20 years, was co-sleeping on a sofa [2]. Breastfeeding has been linked with decreased risk of SIDS and is also highly correlated with co-sleeping, as it facilitates lactation [25,26]. Studies showed that infants sleeping solitarily, were more likely to sleep in prone position, compared with co-sleeping infants. This may partly elucidate the protective properties of breastfeeding against SIDS, during which infants are more probable to be placed in the supine position. Αn 18-fold raise in SIDS deaths while sleeping alongside an adult who consumed more than two units of alcohol or co-sleeping on a sofa was observed [27]. The AAP, in order to advocate for their 2016 guidelines [28], assumed that the data from the analyses do not lead to a reliable inference that bed sharing is safe, even under less dangerous conditions. In contrast, a review of the National Institute for Health and Care Excellence (NICE) [29] concluded that bed sharing itself, is not causal for SIDS and that there in a necessity of providing guidance to parents regarding specific dangerous circumstances of co-sleeping.
Breastfeeding
Researchers have proposed that breastfeeding has a strong correlation with bed sharing [11], showing that “Never Bed- Share” may impede breastfeeding [30,31]. Breastfeeding occurring throughout the night while co-sleeping has been recently coined as “breast sleeping” [32]. Dedication to breastfeeding may also affect infant sleep place decision-making [10]. Many studies assumed breastfeeding as the key reason for co-sleeping [15]. Co-sleeping makes night breastfeeding easier and is related to more regular night feeds (which boosts milk production) and more months of breastfeeding [33]. Breastfeeding mothers reportedly use bed sharing in order to mitigate the toll of extended breastfeeding, such as sleep disturbance [34]. Many studies have shown that breastfeeding co-sleeping mothers wake often to feed, but wake for a shorter time, resume sleep faster [35], and accomplish longer sleep duration [36], in comparison to non-bed sharing mothers [37,38].
Sleep quality
There is a small number of studies dealing with co-sleeping and maternal sleep quality. A recent study [39] showed that breastfeeding women had circadian differences in sleep–wake pattern. They tended to wake up earlier and showed decreased daytime physical activity compared to non-breastfeeding participants, but breastfeeding was not reported to affect sleep duration. An important percentage of non-breastfeeding cosleepers exhibited a decrease in sleep quality [32]. Many studies showed that co-sleepers demonstrated a reduction in total sleep duration and sleep effectiveness [40]. On the contrary, other studies showed that bed sharing makes night pass easier, contributes to baby monitoring, promotes convenience, and helps gaining sleep [30,38,41]. It is interesting that in several studies, co-sleepers do not exhibit an increase in number or duration of daytime naps, in order to compensate for sleep deprivation [32,42-44]. In another study, it was found that breastfeeding co-sleeping participants slept more compared to bottle feeding participants [36]. Cross-cultural studies support that in traditional societies, infants having physical closeness with their mother day and night, have regular awakenings during sleep, and breastfeed on request, during their first year [45].
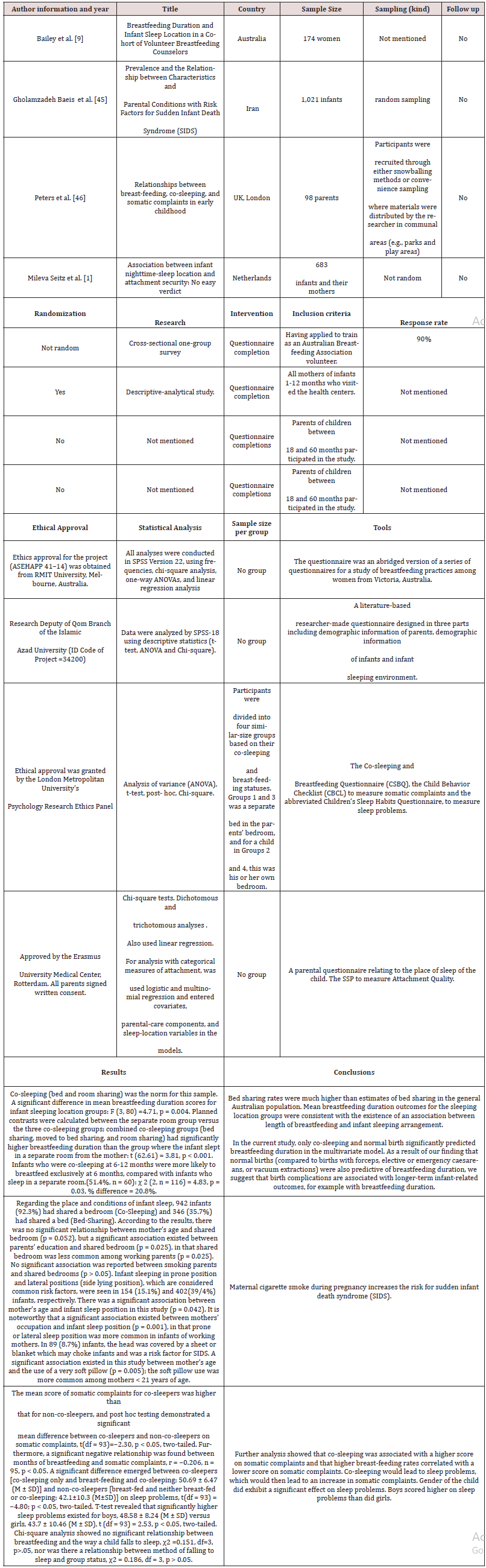
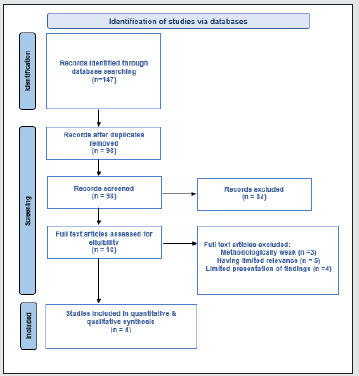
Search strategy
A systematic search of five electronic databases (Medline, Cochrane, CINAHL, EMBASE, and Scopus) was undertaken to identify related studies, using the terms “co- sleeping”, “bed sharing”, “sleep”, “place”, “breastfeeding”, “location”, “infant death”, “infant”. Additional searches that were conducted were based on the references of the selected studies. Initially, 147 articles were found. Titles and abstracts were examined for relevance to the review objective. Studies that met the inclusion criteria were then evaluated for methodological quality. Inclusion criteria were: 1) English language, 2) Quantitate studies, and 3) Studies conducted between 2015-2020.Table 1 presents the methodological characteristics of the included studies. Questionnaires were used as tools for collecting demographic information and data regarding sleeping environment, breastfeeding status, sleeping place, attachment quality and other factors Figure 1.
Figure 1: PRISMA 2020 flow diagram for new systematic reviews which included searches of databases and registers only.
Discussion
This review investigated the safety of co-sleeping and highlighted how cautious parents should be. Moreover, the factors that led to room or bed sharing with an infant and the benefits for infant-parent and their relationship were analyzed. Infants are seemingly social beings; they seek parental contact, while parents are biologically designed to respond and there is a neurological basis that explains it [10,15]. Co-sleeping is based on various grounds, such as making breastfeeding easier and more comfortable, relieving child’s anxiety or sickness, parental willfulness and belief, sleep experiences of parents, fear, infant safety, parental and infant emotional needs, improved infant sleep, the rest of the beds at home are occupied, and improved care [41,46-50]. Co-sleeping affects breastfeeding highly. It was found that breastfeeding duration increases with cosleeping compared to sleeping in a separate room [9]. This finding confirms those of [33]. Another issue that was investigated, was the risk of SIDS, while co-sleeping with an infant. It was found that the risk of SIDS was more common in infants of mothers < 21 years, due to young age and lack of experience in infant care [51]. Moreover, boys were more susceptible to SIDS; families with male neonates should be more careful regarding other risk factors. Parental smoking is the main cause of SIDS. Maternal smoking during pregnancy raises the risk for SIDS [20,51]. It was observed that the third or following neonate in the family has increased risk of SIDS. The lack of breastfeeding is also one more important risk factor for SIDS [25,26,51]. Conclusively, the best way to reduce worries of cosleeping is to assert that parents are aware of SIDS’s risk factors and learn how to alleviate them during infant care.10 The main risk factors are smoking, alcohol and drug use, sleep position and sleeping on a sofa and lack of breastfeeding [19].
Moreover, an association between infant sleep location and secure attachment was reported. The relative risk of developing insecure attachment (combining resistant and avoidant groups) in solitary sleepers was 1.21, 95% CI = 1.05–1.40; they exhibit a lower continuous attachment security in contrast to co-sleepers [t (553) =-3.14, p = 0.002] [1]. More specifically, solitary sleeping in the first 2 months was associated with significantly lower attachment security (insecure attachment) at 14 months (β = -0.12, t (495) =-2.61, p = 0.009), and presented greater odds of developing resistant attachment at 14 months. In conclusion, being in contact with a parent during the night is a protective factor and leads to a secure attachment with the parent. Another link was found between bed sharing and somatic complaints. Bed sharing increases the mean score of somatic complaints compared to non-co-sleeping, [t (df = 93) =-2.30, p < 0.05, two-tailed] which is consistent with the study of [32] reporting, that co-sleeping decreases sleep quality. Furthermore, a significant negative correlation between months of breastfeeding and somatic complaints was observed (r = -0.206, n = 95, p < 0.05). The results of this study showed that co-sleeping is a very common part of child nurturing, as many parents choose to share their bed with their infant during its first months of life. Children are social beings and seek contact with an adult on a neurodevelopmental basis [10,15] and need to be cared for in a way that promotes their ability to thrive. Health-care professionals should advise and educate parents on how to bed-share with safety, inform them about SIDS and how to protect their infants.
Conclusion
Parenting is multidimensional. To respond to the varied needs of their children, parents must develop both depth and breadth of knowledge, ranging from being aware of developmental milestones and norms that help in keeping children safe and healthy to understanding the role and advice of professionals that interact with families and support parenting. Given the small number of chosen studies analyzed in the present study, conclusions for the general public cannot be drawn. However, this review provides a basis for future studies and potentially can stimulate similar studies by other researchers which will help health-care professionals as well as parents. Evidence based data on infant sleep will eventually lead to infant sleep scientists, pediatricians, midwives and parents becoming more informed about the consequences of caring for human infants in ways that are not congruent with their evolutionary biology.
References
- Mileva Seitz VR, Luijk MP, van Ijzendoorn MH (2016) Association between infant nighttime-sleep location and attachment security: no easy verdict. Infant Ment Health J 37(1): 5-16.
- Marinelli KA, Ball HL, McKenna JJ, Blair PS (2019) An integrated analysis of maternal-infant sleep, breastfeeding, and sudden infant death syndrome research supporting a balanced discourse. J Hum Lact 35(3): 510-520.
- Blair PS, Ball HL (2004) The prevalence and characteristics associated with parent-infant bed-sharing in England. Arch Dis Child 89(12): 1106-1110.
- Blair PS, Heron J, Fleming PJ (2010) Relationship between bed sharing and breastfeeding: longitudinal, population-based analysis. Pediatrics 126(5): e1119-e1126.
- Colson ER, Willinger M, Rybin D (2013) Trends and factors associated with infant bed sharing, 1993-2010: The National Infant Sleep Position Study. JAMA Pediatr 167(11): 1032-1037.
- McCoy RC, Hunt CE, Lesko SM (2004) Frequency of bed sharing and its relationship to breastfeeding. J Dev Behav Pediatr 25(3): 141-149.
- Smith LA, Geller NL, Kellams AL (2016) Infant Sleep location and breastfeeding practices in the United States, 2011-2014. Acad Pediatr 16(6): 540-549.
- Barry ES (2021) What is "normal" infant sleep? Why we still do not know. Psychol Rep 124(2): 651-692.
- Bailey C, Tawia S, McGuire E (2020) Breastfeeding duration and infant sleep location in a cohort of volunteer breastfeeding counselors. J Hum Lact 36(2): 354-364.
- Ball HL, Howel D, Bryant A, Best E, Russell C, et al. (2016) Bed-sharing by breastfeeding mothers: who bed-shares and what is the relationship with breastfeeding duration? Acta Paediatr 105(6): 628-634.
- Mileva Seitz VR, Bakermans Kranenburg MJ, Battaini C, Luijk MP (2017) Parent-child bed-sharing: the good, the bad, and the burden of evidence. Sleep Med Rev 32: 4-27.
- Brown A, Arnott B (2014) Breastfeeding duration and early parenting behaviour: the importance of an infant-led, responsive style. PLoS One 9(2): e83893.
- McKenna JJ, Ball HL, Gettler LT (2007) Mother-infant cosleeping, breastfeeding and sudden infant death syndrome: what biological anthropology has discovered about normal infant sleep and pediatric sleep medicine. Am J Phys Anthropol Suppl 45: 133-161.
- Ward TC (2015) Reasons for mother-infant bed-sharing: a systematic narrative synthesis of the literature and implications for future research. Matern Child Health J 19(3): 675-690.
- McKenna J J, Gettler L (2012) Perspective 7: “It’s dangerous to be and infant”: ongoing relevant of John Bowlby’s environment of evolutionary adaptedness in promoting healthier births, safer maternal-infant sleep and breastfeeding in a contemporary western industrial context. In: Narvaez D, Panksepp J, Schore AN, Gleason TR, eds. Evolution, Early Experience and Human Development: From Research to Practice and Policy. 1st Oxford University Press pp. 439-454.
- Gilbert R, Salanti G, Harden M, See S (2005) Infant sleeping position and the sudden infant death syndrome: systematic review of observational studies and historical review of recommendations from 1940 to 2002. Int J Epidemiol 34(4):874-887.
- Bartick M, Tomori C (2019) Sudden infant death and social justice: a syndemics approach. Matern Child Nutr 15(1): e12652.
- (2021) Raising Children Network. Safe Sleeping: 11 tips.
- Mitchell EA, Thompson JM, Zuccollo J (2017) The combination of bed sharing, and maternal smoking leads to a greatly increased risk of sudden unexpected death in infancy: the New Zealand SUDI Nationwide Case Control Study. N Z Med J 130(1456): 52-64.
- Blair PS, Sidebotham P, Evason Coombe C, Edmonds M, Heckstall Smith EM, et al.(2009) Hazardous cosleeping environments and risk factors amenable to change: case-control study of SIDS in southwest England. BMJ 339: b3666.
- Vennemann MM, Hense HW, Bajanowski T (2012) Bed sharing and the risk of sudden infant death syndrome: can we resolve the debate? J Pediatr 160(1): 44-48.
- American Academy of Pediatrics Task Force on Sudden Infant Death Syndrome (2005) The changing concept of sudden infant death syndrome: diagnostic coding shifts, controversies regarding the sleeping environment, and new variables to consider in reducing risk. Pediatrics 116(5): 1245-1255.
- Task Force on Sudden Infant Death Syndrome (2016) SIDS and other sleep-related infant deaths: updated 2016 recommendations for a safe infant sleeping environment. Pediatrics 138(5): e20162938.
- Hauck FR, Thompson JM, Tanabe KO, Moon RY, Vennemann MM (2011) Breastfeeding and reduced risk of sudden infant death syndrome: a meta-analysis. Pediatrics 128(1):103-110.
- Thompson JMD, Tanabe K, Moon RY (2017) Duration of breastfeeding and risk of SIDS: an individual participant data meta-analysis. Pediatrics 140(5): e20171324.
- Blair PS, Sidebotham P, Pease A, Fleming PJ (2014) Bed-sharing in the absence of hazardous circumstances: is there a risk of sudden infant death syndrome? An analysis from two case-control studies conducted in the UK. PLoS One 9(9): e107799.
- Moon RY Task Force on Sudden Infant Death Syndrome (2016) SIDS and other sleep related infant deaths: evidence base for 2016 updated recommendations for a safe infant sleeping environment. Pediatrics. 138(5): e20162940.
- (2021) National Institute for Health and Care Excellence. Addendum to clinical guideline 37, postnatal care 2014.
- Ball HL (2003) Breastfeeding, bed-sharing, and infant sleep. Birth 30(3): 181-188.
- Bartick M, Smith LJ (2014) Speaking out on safe sleep: evidence-based infant sleep recommendations. Breastfeed Med 9(9): 417-422.
- Crittenden AN, Samson DR, Herlosky KN, Mabulla IA, Mabulla AZP, McKenna JJ (2018) Infant co-sleeping patterns and maternal sleep quality among Hadza hunter-gatherers. Sleep Health 4(6): 527-534.
- Santos IS, Mota DM, Matijasevich A, Barros AJ, Barros FC (2009) Bed-sharing at 3 months and breast-feeding at 1 year in southern Brazil. J Pediatr 155(4): 505-509.
- Tully KP, Ball HL (2013) Trade-offs underlying maternal breastfeeding decisions: a conceptual model. Matern Child Nutr 9(1): 90-98.
- Mosko S, Richard C, McKenna J (1997) Maternal sleep and arousals during bedsharing with infants. Sleep 20(2): 142-150.
- Quillin SI, Glenn LL (2004) Interaction between feeding method and co-sleeping on maternal-newborn sleep. J Obstet Gynecol Neonatal Nurs 33(5): 580-588.
- Ateah CA, Hamelin KJ (2008) Maternal bedsharing practices, experiences, and awareness of risks. J Obstet Gynecol Neonatal Nurs 37(3): 274-281.
- Rudzik AEF, Ball HL (2016) Exploring maternal perceptions of infant sleep and feeding method among mothers in the United Kingdom: a qualitative focus group study. Matern Child Health J 20(1): 33-40.
- Thomas KA, Burr RL, Spieker S, Lee J, Chen J (2014) Mother-infant circadian rhythm: development of individual patterns and dyadic synchrony. Early Hum Dev 90(12): 885-890.
- Lee KA, Zaffke ME, McEnany G (2000) Parity and sleep patterns during and after pregnancy. Obstet Gynecol 95(1): 14-18.
- Ball HL (2002) Reasons to bed-share: why parents sleep with their infants. J Reprod Infant Psychol 20(4): 207-221.
- Gay CL, Lee KA, Lee SY (2004) Sleep patterns and fatigue in new mothers and fathers. Biol Res Nurs. 5(4): 311-318.
- Quillin SI (1997) Infant and mother sleep patterns during 4th postpartum week. Issues Compr Pediatr Nurs 20(2): 115-123.
- Matsumoto K, Shinkoda H, Kang MJ, Seo YJ (2003) Longitudinal Study of mothers' sleep-wake behaviors and circadian time patterns from late pregnancy to postpartum: monitoring of wrist actigraphy and sleep logs. Biol Rhythm Res 34(3): 265-278.
- Ball HL (2007) Bed-sharing practices of initially breastfed infants in the first 6 months of life. Infant Child Dev 16(4): 387-401.
- Chianese J, Ploof D, Trovato C, Chang JC (2009) Inner-city caregivers' perspectives on bed sharing with their infants. Acad Pediatr 9(1): 26-32.
- Glover M, Waldon J, Manaena Biddle H, Holdaway M, Cunningham C (2009) Barriers to best outcomes in breastfeeding for Māori: mothers' perceptions, whānau perceptions, and services. J Hum Lact. 25(3): 307-316.
- Hutchison L, Stewart A, Mitchell E (2007) Infant sleep position, head shape concerns, and sleep positioning devices. J Paediatr Child Health 43(4): 243-248.
- Oden RP, Joyner BL, Ajao TI, Moon RY (2010) Factors influencing African American mothers' decisions about sleep position: a qualitative study. J Natl Med Assoc 102(10): 870-880.
- Tikotzky L, Sharabany R, Hirsch I, Sadeh A (2010) "Ghosts in the nursery:" infant sleep and sleep-related cognitions of parents raised under communal sleeping arrangements. Infant Ment Health J 31(3): 312-334.
- Gholamzadeh Baeis M, Miladinia M, Talayian M, Vahedi M, Vafayi S, et al. (2015) Prevalence and the relationship between characteristics and parental conditions with risk factors for Sudden Infant Death Syndrome (SIDS). Int J Pediatr 3(6.2): 1135-1143.
- Peters EM, Lusher JM, Banbury S, Chandler C (2016) Relationships between breast-feeding, co-sleeping, and somatic complaints in early childhood. Infant Ment Health J 37(5): 574-583.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...

.png)