Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6679
Review Article(ISSN: 2637-6679) 
Atypical Parathyroid Adenomas as A Rare Cause of Primary Hyperparathyroidism in an Academic Institution Experience Volume 7 - Issue 4
Kowalski GJ*
- Unląski Uniwersytet Medyczny w Katowicach, Slaski Uniwersytet Medyczny w Katowicach, Poland
Received: April 18, 2022; Published: April 28, 2022
Corresponding author: Kowalski GJ, Unląski Uniwersytet Medyczny w Katowicach: Slaski Uniwersytet Medyczny w Katowicach, Poland
DOI: 10.32474/RRHOAJ.2022.07.000268
Abstract
Background: Primary hyperparathyroidism (pHPT) is caused by benign and malignant conditions. Most commonly by typical adenoma/single gland disease (PA) - this is 80-85% cases of pHPT. Parathyroid hyperplasia or multiple gland disease accounts for 10-15% of cases of PHPT. Atypical parathyroid adenoma (APA) and carcinoma (PC) - very rare conditions -are both responsible for pHPT in approximately 0,5 - 1,5% of cases.
Objectives: To estimate occurrence of atypical parathyroid adenoma, parathyroid carcinoma and parathyroid hyperplasia along with characterize them based on their etiology, clinical presentation, diagnosis and treatment.
Methods: We performed a retrospective study and enrolled 1,019 patients with primary hyperparathyroidism undergoing parathyroidectomy at academic Department of General and Endocrine Surgery between 1983 and 2018.
Results: Out of 1,019 cases of primary hyperparathyroidism, 850 (83.4%) cases were due to typical parathyroid adenoma (PA), 135 (13.2%) cases were due to parathyroid hyperplasia, 29 (2.8%) cases were due to parathyroid carcinoma (PC), and 5 (0.5%) cases were due to atypical parathyroid adenoma (APA).
Keywords: Primary Hyperparathyroidism; Atypical Parathyroid Adenoma; Parathyroid Hyperplasia; Parathyroid Carcinoma; Parathyroidectomy; Hypercalcemia
Introduction
Parathyroid conditions causing primary hyperparathyroidism (pHPT) can be divided into single gland disease and multi gland disease. pHPT most commonly caused by typical adenomas (PA) that are generally benign proliferations in one of the glands and hyperplasia that usually affects all four glands. Parathyroid carcinoma (PC) that is characterized by rapid and invasive growth and atypical parathyroid adenomas (APA) are very rare conditions [1,2-18]. Atypical parathyroid adenomas (APA) have features of adenomas and carcinoma, but they do not grow invasively [19-21]. Patients are often initially asymptomatic, but laboratory studies show increased levels of calcium and PTH, that are usually higher than in typical adenomas, but lower than in carcinoma [6,8,22]. In the case of APA histology shows incomplete invasion of the capsule, fibrous bands, pronounced trabecular growth, increased mitotic activity, tumor necrosis without signs of capsular or vascular invasion [7,14,23]. The diagnosis is similar to typical adenomas (PA), with differences in pathological evaluation, although further tests should be performed to exclude presence of malignancy. Therapeutic approach is surgical resection of the adenoma, and it is curative in most of the cases [24-27]. It is very hard to differentiate benign adenomas (PA) from atypical adenoma (APA) in some cases, not even histopathological evaluation is conclusive [28,29]. Additionally, malignant transformations can occur within atypical adenoma (APA) and can be missed if the sample for biopsy was not taken correctly [14,18-33]. APA is a lesion with suspected clinical and histological malignancies but does not fully meet the criteria for the diagnosis of PC according to the World Health Organization (WHO) [28]. The main purpose of this study is to identify clinical, laboratory and histological differences in patients with typical adenoma (PA) and APA, and to assess the risk of relapse of pHPT in patients with APA. Presentation of the differences between typical and atypical adenomas, hyperplasia and cancer and analyses the data about factors influencing treatment and its outcomes, differences in diagnostic approaches and clinical presentation.
Materials and Methods
We congregated medical data from group of 1,019 patients suffering from primary hyperparathyroidism (pHPT) who had been treated in our clinic. Histopathological changes suspected of being malignant were found in 71 patients, but the diagnosis of parathyroid cancer (PC) was confirmed in 29 patients and 5 (2 woman and 3 men) were finally diagnosed with atypical parathyroid adenomas (APA). The mean age of the total of 1,019 patients was 54 years (range 19 to 81 years), the parathyroid cancer (PC) group was 53 years (range 28 to 69 years) and 52 years (range 38 to 68 years) of atypical adenoma (APA). In the entire group of 1,019 patients, in 19 patients the recurrent or persistent hyperparathyroidism linked to hypercalcemia was found after initial parathyroidectomy - which was not a case in the study group with APA. Our team performed detailed investigation of clinical signs and symptoms, the preoperative and postoperative blood serum levels of calcium and parathyroid hormone. Additionally, we measured the success rate and result after performance of primary parathyroidectomy. We also compared the anatomical localization sites of patients with double parathyroid adenoma to those with single gland neoplasm (adenoma or hyperplasia). Every patient was diagnosed with primary hyperparathyroidism on the basis of biochemical results and radiological measures. Each of them had developed hypercalcemia which needed to be monitored, because 2 cases were in serious risk of hypercalcemic crisis occurrence. The signs and symptoms of each patient were established during the preoperative visit and directly during hospitalization period after the surgery. During the time of follow-up all patients had blood serum calcium levels monitored together with PTH.
Methods of Statistical Analysis
All of the collected data was included in a spreadsheet in Microsoft Office Excel 2019. The statistical analysis was performed in Statistica 12.5. After establishing and classifying the data using a Kolmogorow-Smirnow test, we used Student’s t-test to compare data with normal distribution, and for the non-normal distribution data, we used the Mann-Whitney U test. The results are presented as percentage changes, full numbers, means and standard deviations. The level of significance was calculated at p<0.05. Effect size - ES - was determined using: Youle’s Phi coefficient and Cramer’s V.
Results
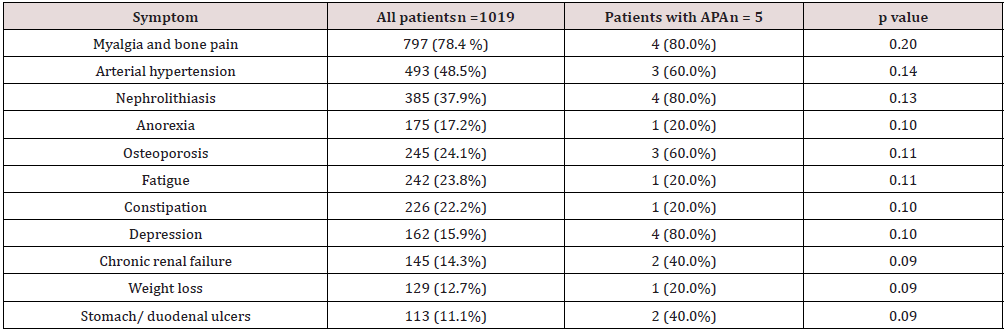
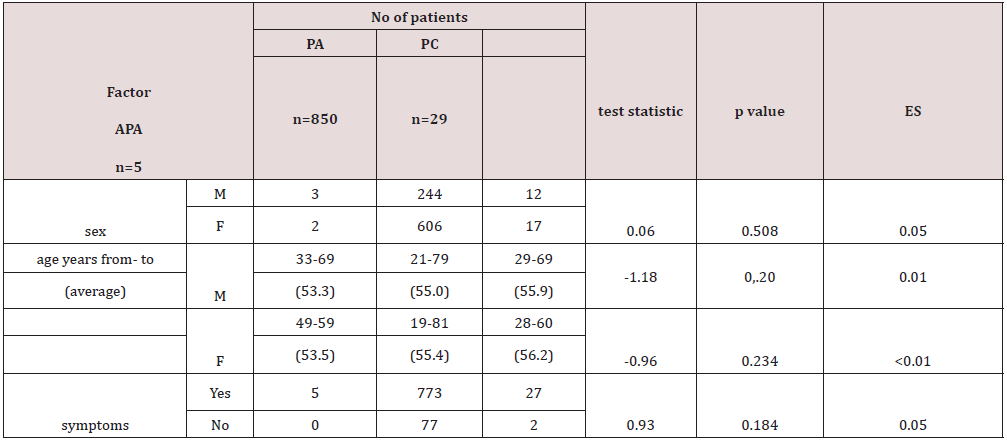
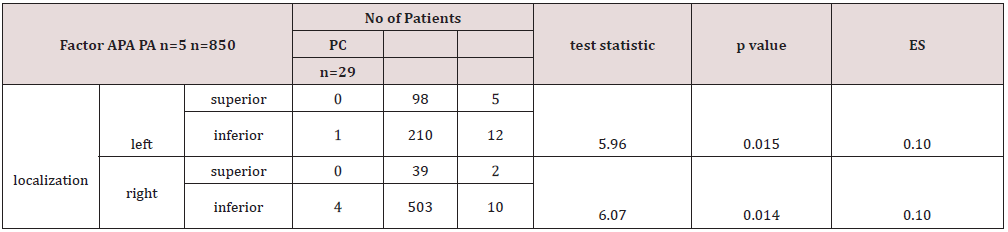
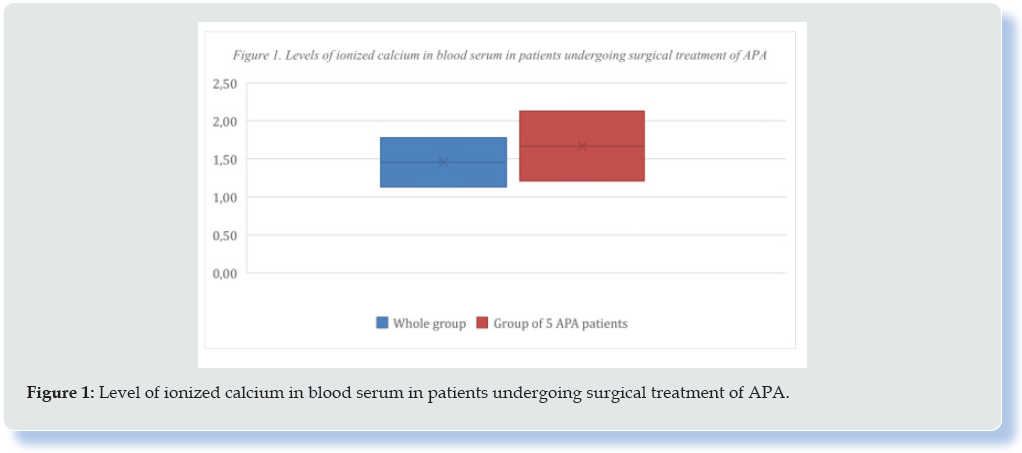
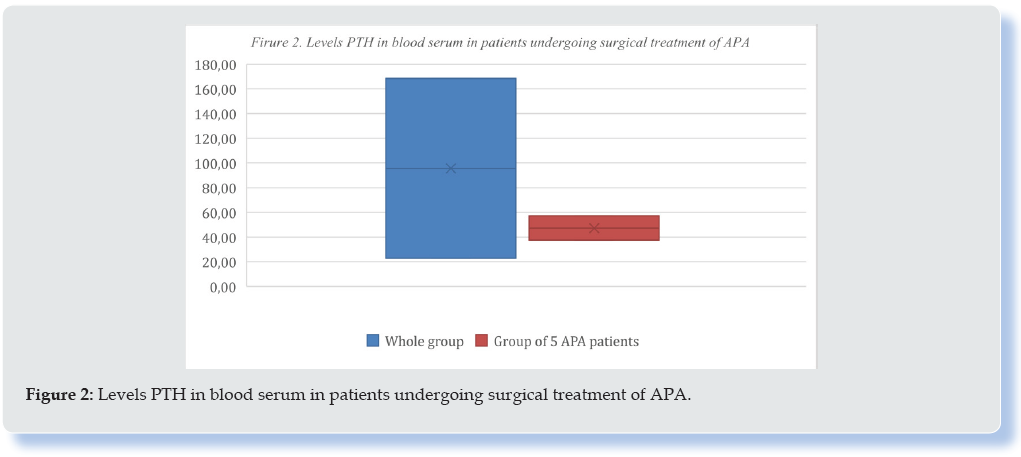
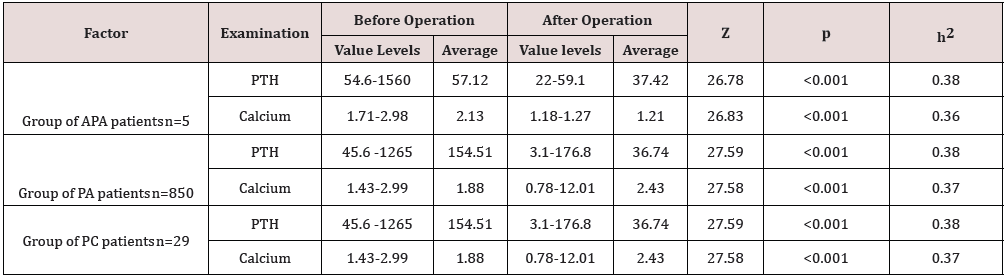
From the group of 1,01 9 patient’s APA were confirmed in 5 (2 woman and 3 men) between 38 to 68, av 52 years. No history of irradiation to the neck or familial HPT was reported. 90.6% of the cases - including all APA patients - were symptomatic at the time of admission, although symptoms were mostly due to hypercalcemia, in variety of fatigue, weakness, depressed mood, bone and muscle pain. Patients with APA were characterized by higher frequency of depression (80.0%), musculoskeletal symptoms (80.0%), nephrolithiasis (80.0%), osteoporosis (60.0%), and stomach/ duodenal ulcers (40.0%) (Table 1). Majority of tumors in a group of 1,019 patients were localized in the neck regions 93.5% and 6.5% were in the mediastinum. In the group of patients with APA, lesions were located once in the mediastinum. In 84% of patients - including all APA patients - the lesions were singular and 16% had multiple with predominance of 2 lesions, more than 3 lesions were also found sporadically. Characteristics of patients are presented in (Table 2). In a group of 1,019 patients operated for pHPT, the growths were almost equally distributed in the left or right parathyroid gland, but most were localized in the regions of inferior lobes of thyroid. In the group of patients with APA, all lesions were so localized. We also performed a comparison of neoplastic glands occurrence between patients with single gland changes and those with multiple abnormal glands. The exact comparison with total number of patients, by the means of localization and number of disordered glands with the group of patients treated for APA is shown in (Table 3). 3 patients had parathyroidectomy. 1 patient had parathyroidectomy with the removal of thyroid lobe and 1 patient had en bloc resection. There were no patients which were reoperated for recurrences of hypercalcemia. All of the patients were alive with no evidence of disease. In the group of 1,019 patients, postoperative patient monitoring showed that in most of the cases parathyroidectomy was successful. Approximately 96.2% of patients did not have symptoms after treatment and their calcium and parathyroid hormone levels stabilized. Patients weremonitored for 5 years and their symptoms did not reoccur and the levels of calcium and PTH stayed within normal ranges. In the group of APA patients, no signs of recurrence of hyperthyroidism were found during the follow-up. In the APA group, we observed slightly higher levels of ionized calcium and PTH in the blood serum compared to the group of patients with typical parathyroid adenomas (PA). Statistically, male group scored higher levels of calcium and PTH than women - similarly in patients with APA. After surgical management calcium and PTH levels dropped to normal values, as shown in (Table 4 & Figure 1) (Figure 2). Regardless of the cause of primary hyperparathyroidism, surgical therapy has a high curative rate. According to the study of 1,019 cases, 96.2% of patients - including patients with APA -after parathyroidectomy were cured and did not experience further episodes of hypercalcemia in the following 5 years. Surgical approach of treatment of hyperparathyroidism is very effective and even in the case of malignant cause of the hyperparathyroidism, the full resection of the tumor and fast diagnosis is a life saving measure with high survival rate.
Table 4: Levels of ionized calcium and PTH in blood serum in patients undergoing surgical treatment due to APA and PA, PC.
Discussion
In our study we presented patients that developed primary hyperparathyroidism, that could be caused by typical adenoma (PA), atypical adenoma (APA), hyperplasia and cancer (PC). According to our research, most cases suffered the symptoms of hypercalcemia due to hyperplasia and typical adenoma (PA) that are benign conditions. The therapeutic outcome for this patients’ group was very satisfactory with a very high rate of curability [1,3,28]. On the other hand, patients with atypical parathyroid adenomas (APA) are at higher risk of development of parathyroid carcinoma (PC), thus it is very important from a surgical point of view to resect all of the tumor to prevent development of malignancy [2,7,33]. Patients will develop symptoms due to hypercalcemia, that mostly include fatigue, malaise, constipation, bone and muscle pain, decreased concentration and depressive episodes [5,28]. After obtaining laboratory blood examination results, we can observe increased levels of calcium and PTH that is indicative of hyperparathyroidism [6,27]. Later we have to distinguish the cause of the disorder. Neck USG can be performed to identify if the gland is enlarged, although the results are usually not enough for diagnosis of hyperplasia [7,8]. The Tc (99 m)-sestamibi scintigraphycan help with a diagnosis, by localization of changed parathyroid gland with a sensitivity of 70-90%, unfortunately its use is limited in multiple lesions of the gland, [9,30]. Therefore, use of USG and scintigraphy could markedly increase sensitivity of the diagnosis. Unfortunately, recent studies showed that even this method is not very accurate and many patients cannot be diagnosed only upon the results of both of these examinations [10]. APA are extremely rare and have only been described 23 times in literature [12,27]. They lack specific criteria from histopathological point of view, it is not possible to differentiate them from benign adenomas and cancerous lesions neither by imaging methods nor macroscopically. Microscopically, they have some features of carcinoma - they adhere to contiguous structures, bends of fibrosis, solid trabecular growth, mitotic activity, but they do not invade the capsule, what is a hallmark of malignancy [12,13,26]. Although, the lack of specific criteria for histopathologic makes it extremely hard to always correctly diagnose the atypical adenoma (APA). The proposed criteria require the presence of at least 2 of those symptoms: intraoperative adherence, bands of fibrosis, pronounced trabecular growth, strong mitotic activity, necrosis, small cells with high nuclear/cytoplasmic ratio, cellular atypia in the absence of unequivocal signs of malignancy [13,14,24]. Use of imaging studies like USG or scintigraphy is limited, because it is not giving the definitive diagnosis. Clinical picture can be very varying, generally the hypercalcemia is slightly lower than seen in cancer, but higher than in typical adenoma (PA). All those similarities make it extremely difficult to distinguish atypical adenoma from carcinoma and benign lesion. The diagnosis of cancer should be supported if there is an invasion of capsule, vessels, neighbouring structures [14,25]. The treatment of choice of atypical parathyroid adenoma (APA) is parathyroidectomy. Without evidence of macroscopic local invasion, the value of en bloc resection at initial surgery remains debatable. The surgeon performing the operation has to be very vigilant and check surrounding tissues for necrosis or any other abnormalities. Also helpful is intraoperative histopathological evaluation in case of doubt. After performing the procedure, the patient should be closely monitored, especially in unclear cases [15]. From a histological point of view the parathyroid carcinoma (PC) can be misdiagnosed as an atypical adenoma (APA) - due to inadequate histopathological sample or other causes. Clinically, the physician should consider diagnosis of carcinoma when the patient presents with renal and bone symptoms simultaneously because dual presentation is quite rare in case of adenomas. Laboratory studies of very high levels of calcium and PTH also can indicate presence of malignancy. On physical examination and sonographic evaluation masses bigger than 3 cm should be considered to be malignant [17,23]. Histopathological studies and genetic analysis of lesions can help with diagnosis of cancerous lesions, but are not alwaysdefinitive. The diagnosis is confirmed if there is obvious sign of invasive growth of the tumor, either invasion of capsule, vessels, neighbouring structure or presence of metastasis at the time of presentation. Although metastatic progression of the tumor is very slow, usually cancer is in an earlier stage. Scintigraphy and USG studies are not very helpful because just upon them we cannot distinguish adenoma and carcinoma [15,17]. Additionally, adjacent lymph nodes should be resected as well [16,17]. If the diagnosis was confirmed based on the result of pathological studies of tumor resected during primary surgery, the treatment becomes more complex. Reoperation is advised in cases in which the surgery did not restore levels of calcium and PTH. In cases where primary surgery resolved the symptoms, patients should be strictly monitored and the levels of calcium and PTH should be measured regularly for surveillance of cancer return [17-29]. Primary hyperparathyroidism is a clinical manifestation of benign and malignant conditions. Quick and precise diagnosis followed by surgical resection of hyperfunctioning tissue is the only curative approach [21,22,32]. Multidisciplinary approach should always be preferred in patients with this condition due to difficult differential diagnosis and not clear criteria [23].
Conclusion
Primary hyperparathyroidism can be a manifestation of growing adenoma, hyperplasia of the gland, carcinoma or atypical parathyroid adenoma. In case of diagnosis of atypical adenoma, patients after parathyroidectomy should be closely monitored for any evidence of malignant proliferation. Although, vast majority are caused by benign lesions, the malignancies can present very similarly making it very difficult to quickly diagnose and treat - especially in the case of atypical adenoma. The laboratory examinations can be helpful, especially if very high levels of calcium and PTH are noted. The PTH and ionized calcium levels can be a good prognostic factor but are not definitive in the differential diagnosis between atypical adenoma, cancer or parathyroid adenoma. Some clinical features and histopathological evaluation of the lesion in many cases can be very helpful in the differential diagnosis, but not always is enough for formation of conclusive diagnosis. In cases that are very suspicious for malignancy, aggressive surgical approach is preferred and cautious monitoring of a patient after surgery is extremely important for establishing a good prognosis.
References
- Wieneke JA, Smith A (2008) Parathyroid Adenoma. Head and Neck Pathology 2(4): 305- 308.
- Baj J, Sitarz R, Łokaj M, Forma A, Czeczelewski M, Maani A, et al. (2020) Preoperative and Intraoperative Methods of Parathyroid Gland Localization and the Diagnosis of Parathyroid Adenomas. Molecules 25(7): 1724.
- Ramaswamy AS, Vijitha T, Kumaraguru BN, Mahalingashetty PB (2017) Atypical parathyroid adenoma. Indian J Pathol Microbiol 60: 99-101.
- Institute NC, National Cancer Institute (2020) Parathyroid Hyperplasia. Definitions.
- Institute NC, National Cancer Institute (2020) Parathyroid Chief Cell Hyperplasia. Definitions.
- Marcocci C, Cetani F, Rubin MR, Silverberg SJ, Pinchera A, Bilezikian JP (2008) Parathyroid carcinoma. J Bone Miner Res 23: 1869-1880.
- Chen JD, Morrison C, Zhang C, Kahnoski K, Carpten JD, Teh BT (2003) Hyperparathyroidism- jaw tumour syndrome. J Intern Med 253: 634-642.
- DeLellis RA (2005) Parathyroid carcinoma: an overview. Adv Anat Pathol 12: 53-61.
- Lo CY, Lang BH, Chan WF, Kung AWC, Lam KSL (2007) A prospective evaluation of preoperative localization by technetium-99m sestamibi scintigraphy and ultrasonography in primary hyperparathyroidism. Am J Surg 193: 155-159.
- Kasai ETP, da Silva JWE, Mandarim de Lacerda CA, Boasquevisque E (2008) Parathyroid glands: combination of sestamibi-(99m) Tc scintigraphy and ultrasonography for demonstration of hyperplasic parathyroid glands. Rev Esp Med Nucl 27: 8-12.
- Thompson LDR (2013) Benign neoplasms of the parathyroid gland. Head and Neck Pathology pp. 644-652.
- Raj R, Amine A, Herodotou D (2020) Postoperative hypocalcemia following parathyroidectomy for giant parathyroid adenoma. AACE Clin Case Rep 6(6): e352-e356.
- Cetani F, Marcocci C, Torregrossa L, Pardi E (2019) Atypical parathyroid adenomas: challenging lesions in the differential diagnosis of endocrine tumors. Endocrine-Related Cancer 26(7): R441-R464.
- Husniye Baser, Ali Karagoz, Ahmet Okus, Mustafa Cayci, Meryem Ilkay Eren Karanis, et al. (2013) Differential Diagnosis of Atypical Parathyroid Adenoma and Parathyroid Carcinoma in a Case with Severe Hypercalcemia. Journal of Medical Cases.
- McCoy KL, Seethala RR, Armstrong MJ, Nikiforova MN, Stang MT, Carty SE, et al. (2015) The clinical importance of parathyroid atypia: Is long-term surveillance necessary? Surgery 158(4): 929-936.
- Shane E (2001) Parathyroid Carcinoma. The Journal of Clinical Endocrinology & Metabolism pp. 485-493.
- Kebebew E (2008) Parathyroid carcinoma, a rare but important disorder for endocrinologists, primary care physicians, and endocrine surgeons. Thyroid 18: 385-386.
- Yamamoto T (2001) Comment on “Clinical Review 122: Parathyroid Carcinoma”a. Journal of Clinical Endocrinology & Metabolism pp. 5091-5091.
- Rawat N, Khetan N, Williams DW (2005) Baxter JN Parathyroid carcinoma. Br J Surg 92: 1345-1353.
- Lee PK, Jarosek SL, Virnig BA, Evasovich M, Tuttle TM (2007) Trends in the incidence and treatment of parathyroid cancer in the United States. Cancer 109: 1736-1741.
- Kowalski G, Bula G, Zadlo D, Gawrychowska A, Gawrychowski J (2020) Primary hyperparathyroidism. Endokrynologia Polska 71(3): 260- 270.
- Al-Sobhi S, Clark OH (1997) Parathyroid hyperplasia; Parathyroidectomy. In: Clark OH, Duh QY, editors. Textbook of Endocrine Surgery. 1st ed. Philadelphia: WB Saunders Company pp. 372-379.
- Mehmet Uludağ, Nurcihan Aygün, Adnan İşgör (2019) Main Surgical Principles and Methods in Surgical Treatment of Primary Hyperparathyroidism. Sisli Etfal Hastan Tip Bul 53(4): 337-352.
- Bilezikian JP, Marcus R, Levine MA (2001) Preface to the Second Edition. The Parathyroids pp. 15-16.
- Amit Agarwal, Roma Pradhan, Niraj Kumari, Narendra Krishnani, Pooja Shukla, et al. (2016) Molecular Characteristics of Large Parathyroid Adenomas. World J Surg 40(3): 607-614.
- Bilezikian JP, Bandeira L, Khan A, Cusano NE (2018) Hyperparathyroidism. Lancet 391(10116): 168-178.
- DeLellis R, Larsson C, Arnold A, Lloy R, Bilezikian J, Mete O (2017) Tumors of the parathyroid glands. In WHO Classification of Tumors of Endocrine Organs, 4th ed. Eds Lloyd R, Osamura R, Kloppel G & Rosai J. Lyon, IARC Press, France.
- Hu Y, Liao Q, Cao S, Gao X, Zhao Y (2016) Diagnostic performance of parafibromin immunohistochemical staining for sporadic parathyroid carcinoma: a meta- analysis. Endocrine 54(3):612-619.
- Hu Y, Cui M, Xia Y, Su Z, Zhang X, Liao Q, Jiang Y, Zhao Y (2018) The clinical features of cystic parathyroid adenoma in Chinese population: a single-center experience. International Journal of Endocrinology pp.374523.
- Katz L, Abdel Khalek M, Crawford B & Kandil E (2012) Robotic-assisted transaxillary parathyroidectomy of an atypical adenoma. Minimally Invasive Therapy and Allied Technologies 21(3): 201-205.
- Ozolins A, Narbuts Z, Vanags A, Simtniece Z, Visnevska Z, AkcaA (2015) Evaluation of malignant parathyroid tumours in two European cohorts of patients with sporadic primary hyperparathyroidism. Langenbeck's Archives of Surgery 401(7): 943-951.
- Al Hassan MS, Mekhaimar M, El Ansari W, Darweesh A, Abdelaal A (2019) Giant parathyroid adenoma: a case report and review of the literature. J Med Case Rep 13(1): 332.
- Quinn CE, Healy J, Lebastchi AH et al. (2015) Modern experience with aggressive parathyroid tumors in a high-volume New England referral center. J Am Coll Surg 220: 1054-1062.

.png)