
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6679
Review Article(ISSN: 2637-6679) 
A Practical Approach to Adolescent Obesity Treatment and Maintenance, Suggestion: AIM Model, Review of Current Studies Volume 7 - Issue 2
Mohammad Hossein Sharifi1*, Masood Karimi2, Vahid Keshtkar3 and Hossein Molavi Vardanjani4
- 1Assistant Professor in nutrition, Research Center for Traditional Medicine and History of Medicine, Shiraz University of Medical Sciences, Iran
- 2Assistant Professor of Health Education and Promotion, Department of Health Promotion and Education, School of Health, Shiraz University of Medical Sciences. Iran
- 3Instructor of Healthcare Services Management, Department of Community Medicine, School of Medicine, Shiraz University of Medical Sciences, Iran
- 4Research Center for Traditional Medicine and History of Medicine, Shiraz University of Medical Sciences, Iran
Received: January 04, 2022 Published: January 25, 2022
Corresponding author: Mohammad Hossein Sharifi, Assistant Professor in nutrition, Research Center for Traditional Medicine and History of Medicine, Shiraz University of Medical Sciences, Iran
DOI: 10.32474/RRHOAJ.2022.07.000262
Abstract
Adolescent obesity is one of the most serious public health problems. The most common obesity treatments include built-in of diet, exercise, and behavior therapy has not great success in adolescent obesity treatment. Thus, clinicians should take to effective and practical interventions to manage the adolescent obesity. There are multi-approaches in obesity treatment, but most available forms of treatment are complex, not specific for adolescent age group, and ineffective in long term. Moreover, there had had less attention to psychological issues such as, emotional problems, cognitive intervention, motivation interview, self-monitoring, selfhelp and body image in pediatric obesity management. On the other side, best practical approach to the treatment of adolescent obesity and maintenance is still under controversy. With reference to these concerns, we studied the approaches in recent published papers on adolescent obesity treatment, and subsequently, in this work, a new simple and practical model for adolescent obesity treatment and maintenance as “AIM” model (Assessment, Intervention, and Maintenance model) is suggested. “AIM” model offers an innovative approach for clinical care.
Keywords: Adolescent obesity; Treatment; Maintenance
Introduction
Obesity in adolescents is one of the most serious public health problems. Nearly 20%-25% of children and adolescents are overweight or obese [1]. The worldwide prevalence of obesity was more than doubled between 1980 and 2014 [2]. More than 40% of children in eastern Mediterranean WHO regions, 38% in Europe, 27% in the western Pacific, and 22% in Southeast Asia were predicted to be overweight or obese. Pediatric obesity prevalence in Iranian children is alarming and should be planned by providers at national and local levels [3,4]. The most common treatments in obesity include built-in of diet, exercise, and behavior therapy, which are often referred to as lifestyle modifications [5,6]. A greater number of weight-loss efforts have been repeatedly demonstrated to be a negative prognostic indicator of weight-loss success in the current treatment [7]. A Cochrane systematic review of 55 published interventions to manage obesity has found that the small effects during the intervention period and further weight reduction by longer interventions are unknown [8,9]. Besides, evidence reveals that systemic review analysis regarding childhood obesity interventions provide limited information in policy and best approach. Thus, clinicians are seeking the take to effective and practical interventions to manage the youth obesity [10]. There are multi-approaches in treatment of obesity. Most available forms of treatment are complex, not specific for adolescent age group, and ineffective in long term. Moreover, there has been less attention paid to psychological issues [11] such as emotional problems, cognitive intervention, motivation interview, self-monitoring, self-help and body image in Pediatric obesity management. On the other hand, best applicable approach to the treatment of adolescent obesity and maintenance is still under controversy. Therefore, it is essential to improve the knowledge of obesity treatment and implementation of practical approach [12]. With reference to these concerns, we studied the approaches in recent published papers on teenage obesity, and, subsequently, in this work, a new simple and practical model for adolescent obesity treatment and maintenance as “AIM” Model (Assessment, Intervention, and Maintenance Model) is suggested.
Method
The electronic databases (Pub Med, Scopus and Google scholar) in October of 2000 were searched using simple or a combination of keywords such as “adolescent obesity treatment”, “body image”, “family base therapy”, “obesity and behavioral therapy”, “obesity and cognitive therapy”, and “obesity and self-help and motivation interview”. Although the intended sample for this review was adolescents (ages 13-18), some studies included participants with the age of 10 -18 years. We considered randomized controlled trials, reviews, and observational studies. Adolescent obesity treatment associated to behavioral intervention, cognitive therapy, familial base and school base intervention, self-help, motivation counseling, and body image were included in the review. A total of 40 studies met the inclusion criteria.
Result
Studies were included in this review and shared similar overall
goals and objectives. However, there were multiple differences in
study design, approach, quality, sample size, and power, and it is
not possible to collect studies in the same table for comparison.
As a matter of fact, almost all approaches have paid less attention
to long term adolescent obesity treatment. After review of data, it
was found that there are different approaches to children’s obesity
intervention or maintenance including:
a) School base intervention
b) Family base intervention
c) Education intervention
d) Lifestyle modification
e) Behavioral intervention
f) Cognitive behavioral intervention
g) Dietary intervention
h) Self-help intervention
i) Group self-help intervention
j) Motivation interview
k) Seven-Steps Model and Immersion Treatments
l) Self-monitoring
m) Stimulus control and reinforcement
All the expert committees recommend using intensive dietary, physical activity, and behavioral counseling in adolescent obesity treatment [13,14] and families should be encouraged to take added steps to increase promising results and significant progresses in the management of obesity adolescence periods. However, longterm effect is controversial. Therefore, experts seek to find ways for the best result for long term intervention. There are multimodels in approaches to children obesity treatment. Some of these models are: 2007 health care organizations’ four-stage model, 2007 Canadian clinical practice guidelines, 2008 Endocrine Society recommendations, and 2009 seven-step model [15]. Although these models are clear, simple, and -oriented directions, it seems that they are not especially designed for adolescent age groups. Also, less attention has been paid to maintenance and they are not suitable for practice in clinics. In fact, there is not any single agreement practical model as well. Seemingly, there is a lack of data in practical approach to children’s obesity treatment and maintenance. Therefore, we recommend a simple and practical model to be used for adolescent obesity treatment and maintenance. We found seven important steps in children’s obesity treatment, which may be classified into three parts: assessment, intervention, and maintenance. This comprehensive approach suggests one new model as “AIM” (Assessment, Intervention, and Maintenance Model) (Figure 1).
Figure 1: schematic of “AIM” (Assessment, Intervention, and Maintenance Model) to approach adolescent obesity.
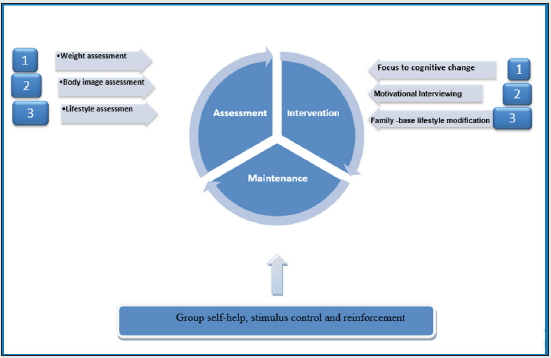
Assessment
a) Weight assessment
b) Body image assessment
c) Lifestyle assessment
Intervention
a) Focus to cognitive-behavioral therapy (CBT)
b) Motivational interviewing
c) Modification of family-base lifestyle
Maintenance
a) Group self-help, stimulus control and reinforcement
Discussion
Although the prevalence of adolescent obesity in developed and developing country is alarming, there is not any particular and practical remedy for adolescent obesity management for long term. Therefore, this study will discuss different approaches in adolescents’ obesity treatment with emphasis on the long-term effect in three parts: “Assessment”, “Intervention”, and “Monitoring”.
Assessment
obesity Assessment: Body mass index (BMI) percentile is wellknown
as simple means to define or diagnose overweight and
obesity in adolescents. Waist circumference percentile has no
significant advantage over BMI percentile for the diagnosis of
obesity in adolescent [16-19]. BMI percentiles are specific for age
and gender, and explain underweight, healthy weight, overweight,
and obesity in adolescent [20]. [16] The BMI percentile assessment
is the first step in this suggestion model; however, some specialists
believed that BMI percentile is not a perfect tool and clinicians
should discover better tools to evaluate the obesity and overweight
in adolescence [21,22].
Body image assessment: Perceived body image was calculated
using the Stunkard scale, which consisted of figure drawings,
ranging from 1 to 9 with step-by-step enhancement in more weight
percentage, where “1” is the leanest and “9” is the heaviest [23]. It is
essential to assess perceived body image plus body mass index (BMI).
Correction of perceived body image has been associated to advance
the motivation for modifying lifestyle behavior. Adolescents may be
less likely to perceive themselves as overweight or obese [24] since
a great number of adolescents have had an improper self-perceived
weight and that weight perception was linked with lack of weightcontrol
behavior [25]. Body image and weight are also influenced by
social norms and customs. In this respect, plumpness seems to be
a symbol of good looks and pleasant appearance in some cultures.
However, attitudes towards body weight may change over time, and
a desire for a thinner body image is detected among adolescents in
some developing countries [25,26]. Among overweight students, a
considerable proportion of them does not judge to be overweight
(i.e. they mistakenly considered themselves as either “right weight”
or “underweight”), and this proportion was almost twice as much
among boys (46% versus 26% in girls, P = .004). We have also
found some unsuitable weight-related behaviors: a considerable
proportion of the normal-weight students was demanding to gain
weight, and a substantial proportion of the overweight students
was not demanding to lose weight. This finding highlights the
fact that there is a growth in overweight trend [25]. Body image
problems are vastly prevalent in overweight and obese adolescents.
Boys and girls perceive their body image in a different way. Many
overweight boys were satisfied with their body image while most
overweight girls wanted a thinner body [23]. Studies show a direct
link between body image problems with eating behaviors and
eating disorders [27]. Therefore, improving body image might be
a possible technique in modifiable eating behaviors and obesity
treatment. In addition, it might play a vital role in the improvement
of eating self-regulation during weight control.
Lifestyle assessment
Lifestyle assessment and intervention are helpful in weight management. The HABITS questionnaire can be reliably used in an adolescent setting to quickly assess the key dietary and physical activity, sedentary behaviors, and to help modify behaviors for weight management [28,29]. The meta-analyses indicate that lifestyle assessment and interventions incorporating a dietary component may lead to significant weight loss in long-term and to weight control maintenance provided that the modification period is over 6- to 12-months [30,31].
Intervention
Focus from behavior therapy to cognitive-behavioral therapy (CBT):
The classical behavior change process consists of selfmonitoring, goal setting, and problem solving. Self-monitoring is the central part of behavioral weight loss intervention programs. The most recent systematic literature review has pointed to the effectiveness of behavioral weight management interventions. However, evidence is more limited for long-term maintenance weight improvement beyond 12 months after treatment [32,33]. Cognitive change process is facilitated through the use of two skills as problem-solving and cognitive restructuring. The question of whether the cognitive changes precedes and causes behavior change has been the subject of theoretical debate for several decades [34]. CBT for weight loss certainly influences the lifestyle habits of family members. Cognitive change can reduce energy intake and promote a more positive attitude toward physical activity [35]. Thus, cognitive processes influenced during obesity treatment may be related to long-term success [34].
*Problem-Solving:
In standard behavior therapy programs, problem-solving has multi-steps. The first step is to recognize the problem in detail. It is also useful to identify the chain of events that preceded the problem behavior. In the second step, potential solutions are generated.
*Cognitive Restructuring:
Non-positive thoughts can block the desired behavior change. Thus, in standard behavior therapy, patients’ thoughts that interfere with their ability to meet behavioral goals are monitored; then, distortions in those thoughts are identified and the dysfunctional thoughts are replaced with more rational thoughts [34]. Although behavior therapy constantly induces mean weight losses of just about 10% of initial weight, these reductions are difficult to maintain. Some experts argue that an alteration in focus from behavior change to cognitive change will progress towards longterm results of lifestyle modification programs [34].
Motivational Interviewing:
Although motivational interviewing was first started in adult health addiction services 20 years ago, attention has rotated to the potential of motivational interviewing in the children’s setting [35]. An addition of motivational interviewing approach to behavioral family-based pediatric obesity treatment is a practical alternative to usual intervention approaches [36]. Motivational interviewing is a person-centered approach designed to explore disbelief and make active motivation to change behavior. Some sets of rules which are planned to consider how motivational interviewing can effect behavior change in pediatric obesity have been reported [35]. Several studies have indicated that children motivated for lifestyle modification had difficulty in maintaining motivation and adaptation with healthy modification after 1–2 months. However, with the constant use of motivational interviewing techniques, there was a trend toward better obesity management and maintenance [37,38]. Standard motivational interviewing techniques and familybased education regarding healthy lifestyle choices can have a great impact on the pediatric motivation ability to build maintenance change. Focus on individual motivation for changing and involving the family are essential to improve the child’s ability to make healthy choices and maintain motivation for change [39].
Family-based lifestyle modification:
Parents’ involvement in treatment of childhood and adolescence obesity is largely supported. Evidence showed that almost effective interventions (particularly in studies that register 12-year-old children,) have included a family part training session [30,40,41]. The roles of parents in arrangement of a healthy home condition and handling children in eating habits and lifestyle are very important. Studies have confirmed a correlation between families and child obesity, especially among mothers and their children. Strength of family involvement and eating habit changes are important factors in the success of long-term childhood weight control interventions [42-44]. Furthermore, there are data of strong associations between parenting lifestyle and children’s food habits, level of physical activity, and weight control. These relations suggest that family is critical in treatment of obesity. Both parents and children have reported the need for continuing support to keep up the eating behavioral changes made during treatment. These strategies are vital to build the parents’ confidence in their ability to maintain their recently acquired health behaviors independent of health providers’ help [43]. Diet and dietary composition are major elements in treatment strategies. These strategies include the lowcalorie diets and other dietary approaches, along with exercise as another key component of weight loss strategies [45]. But the most efficacious and reliable way to treat obesity in adolescents is a dietary plan plus lifestyle modification component in the family [46]. Family-based behavioral weight loss treatment is associated with more reductions in child weight compared with a decrease in child energy intake alone [47,48]. In addition, there is insufficient evidence to draw conclusions about the effectiveness of schoolbased nutrition education interventions alone [49]. So, Parentchild treatment program in the family health care setting would result in significant child weight loss relative to common childhood weight loss program and this relative weight loss can be constant for more than 2 years [43].
Maintenance: Group self-help, stimulus control and reinforcement
Self – help is an action to improve yourself or to solve your problems without the help of others [28,50]. If self-help is combined with lifestyle modification, it will have a better outcome [51]. Self-help for obesity can be a helpful treatment opportunity, with special advantages such as encouragement, back up, and leadership. Individuals who practice self-help may have a more self-control decision. Self-help has a less formal structure program, but group self-help has a more formal structure and is less independent. Individuals who use the most independent strategies can significantly improve the cost-effectiveness of treatment and maintenance [52]. Group self-help subjects may benefit from the repeated weight-loss attempts regardless of prior failures [7]. The long-term maintenance of obesity treatment will probably require continuing care. Continuing care may be economically feasible when it uses self-help or group self-help treatment modalities [53]. Although self-monitoring and weight self-record may affect the adolescent obesity treatment, environment stimulus control and reinforcement appear to be more effective than decreasing sedentary behaviors and eating disorder in maintenance weight control [54,55].
Conclusion
The growing prevalence of adolescent obesity has led to a specific attention to new modelling management and maintenance. These demands for treatment cannot often be met by available professional guidelines, and clients and professionals are looking for other alternatives. A rising body of research literature on body image, behavior therapy, cognitive behavior therapy, familybased intervention, and group self-help has studied the subject, and it is possible for clinicians and clients to evaluate the relative efficacy of different treatment approaches in Pediatric obesity treatment. We suggest that multi-component interventions and practical approaches that seem to have greater impacts than diet and behavioural interventions alone be applied. As a result, this suggestion as “AIM” consists of three parts of assessment, intervention, and maintenance. Future research should also evaluate the role of stressed clients, level of family support, and social factors such as peer support in prediction and maintenance of weight loss and maintenance.
References
- Batch JA, LA Baur (2015) Management and prevention of obesity and its complications in children and adolescents. The Lancet.
- WHO (2015) Obesity and overweight. Fact sheet N 311.
- Kelishadi R (2014) Trend in the prevalence of obesity and overweight among Iranian children and adolescents: A systematic review and meta-analysis. Nutrition 30(4): 393-400.
- Dorosty A, F Siassi, J Reilly (2002) Obesity in Iranian children. Archives of disease in childhood 87(5): 388-391.
- Rosnov DL (2011) Acceptability of weight-loss interventions among adolescents who are overweight and their caregivers. Children's Health Care 40(3): 179-196.
- Baygi F (2013) Dietary predictors of childhood obesity in a representative sample of children in north east of Iran. Chinese journal of contemporary pediatrics 15(7): 501-508.
- Latner JD and AC Ciao (2014) Weight-loss history as a predictor of obesity treatment outcome: Prospective, long-term results from behavioral, group self-help treatment. Journal of health psychology 19(2): 253-261.
- Lobstein T (2015) Child and adolescent obesity: part of a bigger picture. The Lancet 385(9986): 2510-2520.
- Wilfley DE (2007) Lifestyle interventions in the treatment of childhood overweight: a meta-analytic review of randomized controlled trials. Health Psychology 26(5): 521-532.
- Crume TL and CS Harrod (2013) Childhood obesity: is there effective treatment? JAMA pediatrics 167(8): 697-699.
- Bjornelv S, HM Nordahl, TL Holmen (2011) Psychological factors and weight problems in adolescents. The role of eating problems, emotional problems, and personality traits: the Young-HUNT study. Social psychiatry and psychiatric epidemiology 46(5): 353-362.
- Danese A, M Tan (2014) Childhood maltreatment and obesity: systematic review and meta-analysis. Molecular psychiatry 19(5): 544-554.
- Kirschenbaum DS, K Gierut (2013) Treatment of childhood and adolescent obesity: An integrative review of recent recommendations from five expert groups. Journal of consulting and clinical psychology 81(2): 347.
- Pretlow RA (2015) Treatment of Child/Adolescent Obesity Using the Addiction Model: A Smartphone App Pilot Study. Childhood Obesity.
- Kirschenbaum DS, KJ Gierut (2013) Five recent expert recommendations on the treatment of childhood and adolescent obesity: toward an emerging consensus-a stepped care approach. Childhood Obesity 9(5): 376-385.
- Javed A (2015) Diagnostic performance of body mass index to identify obesity as defined by body adiposity in children and adolescents: a systematic review and meta‐analysis. Pediatric obesity. 10(3): 234-244.
- Reilly JJ (2010) Comparison of waist circumference percentiles versus body mass index percentiles for diagnosis of obesity in a large cohort of children. International Journal of Pediatric Obesity 5(2): 151-156.
- Reilly J (2000) Identification of the obese child: adequacy of the body mass index for clinical practice and epidemiology. International journal of obesity 24(12): 1623-1627.
- Dorosty Motlagh A, B Mohammad pour Ahranjani, F Siassi (2009) Determination of the most relevant body mass index standard references to define obese Iranian school-age children. Iranian Journal of Nutrition Sciences & Food Technology 4(2): 71-80.
- Roberts KC (2012) Overweight and obesity in children and adolescents: results from the 2009 to 2011 Canadian Health Measures Survey. Health rep23(3): 37-41.
- Krebs NF (2007) Assessment of child and adolescent overweight and obesity. Pediatrics. 120(Supplement 4): S193-S228.
- Mei Z (2002) Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. The American journal of clinical nutrition 75(6): 978-985.
- del Mar Bibiloni, M., et al., Body image and eating patterns among adolescents. BMC Public Health, 2013. 13(1): p. 1104.
- Maximova K (2008) Do you see what I see? Weight status misperception and exposure to obesity among children and adolescents. International Journal of Obesity 32(6): p. 1008-1015.
- Alwan H (2011) Is accurate perception of body image associated with appropriate weight-control behavior among adolescents of the Seychelles. Journal of obesity.
- Wardle J, AM Haase, and A Steptoe (2006) Body image and weight control in young adults: international comparisons in university students from 22 countries. International journal of obesity 30(4): 644-651.
- Carraça EV (2011) Body image change and improved eating self-regulation in a weight management intervention in women. Int J Behav Nutr Phys Act 8: 75.
- Wright N (2011) A lifestyle assessment and intervention tool for pediatric weight management: the HABITS questionnaire. Journal of human nutrition and dietetics 24(1): 96-100.
- Kushner RF and DH Ryan (2014) Assessment and lifestyle management of patients with obesity: clinical recommendations from systematic reviews. JAMA 312(9): 943-952.
- Ho M (2012) Effectiveness of lifestyle interventions in child obesity: systematic review with meta-analysis. Pediatrics 130(6): e1647-1671.
- Baillot A (2015) Effects of Lifestyle Interventions That Include a Physical Activity Component in Class II and III Obese Individuals: A Systematic Review and Meta-Analysis. PloS one 10(4): e0119017.
- Wing RR (2014) 11 Behavioral Approaches to the Treatment of Obesity. Handbook of Obesity Clinical Applications 2: 131.
- Decaluwé V and C Braet (2005) The cognitive behavioural model for eating disorders: A direct evaluation in children and adolescents with obesity. Eating Behaviors 6(3): 211-220.
- Fabricatore AN (2007) Behavior therapy and cognitive-behavioral therapy of obesity: is there a difference? Journal of the American Dietetic Association 107(1): 92-99.
- Christie D and S Channon (2014) The potential for motivational interviewing to improve outcomes in the management of diabetes and obesity in paediatric and adult populations: a clinical review. Diabetes, Obesity and Metabolism16(5): 381-387.
- Saelens BE, P Lozano and K Scholz (2013) A randomized clinical trial comparing delivery of behavioral pediatric obesity treatment using standard and enhanced motivational approaches. Journal of pediatric psychology 2013: p. jst054.
- Rossini R (2011) Effects of cognitive-behavioral treatment for weight loss in family members. Journal of the American Dietetic Association 111(11): 1712-1719.
- Bohman B (2013) Motivation and health behavior in the prevention of childhood obesity.
- Tripp SB (2011) Providers as weight coaches: using practice guides and motivational interview to treat obesity in the pediatric office. Journal of pediatric nursing 26(5): 474-479.
- Niemeier BS, JM Hektner and KB Enger (2012) Parent participation in weight-related health interventions for children and adolescents: a systematic review and meta-analysis. Preventive medicine 55(1): 3-13.
- Tabatabaei M, A Dorosti, and S Keshavarz (2005) Family Related Obesity Risk Factors In Iranian Primary School Children.
- Kruk J (2013) Obesity: a systematic review on parental involvement in long‐term European childhood weight control interventions with a nutritional focus. obesity reviews 14(9): 745-760.
- Endevelt R (2014) An intensive family intervention clinic for reducing childhood obesity. The Journal of the American Board of Family Medicine 27(3): 321-328.
- Davison KK, HA Lawson and JD Coatsworth (2012) The family-centered action model of intervention layout and implementation (FAMILI) the example of childhood obesity. Health promotion practice 13(4): 454-461.
- Bray GA and C Bouchard (2014) Handbook of Obesity Clinical Applications 2.
- Trivedi S, A Burton, and J Oden (2014) Management of pediatric obesity: A lifestyle modification approach. The Indian Journal of Pediatrics 81(2): 152-157.
- Holland JC (2014) Modifications in parent feeding practices and child diet during family‐based behavioral treatment improve child zBMI. Obesity 22(5): E119-E126.
- David S Ludwig (2007) Recommendations for Treatment of Child and Adolescent Overweight and Obesity.
- Brown T and C Summerbell (2009) Systematic review of school‐based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: an update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obesity reviews 10(1): 110-141.
- Carels RA (2009) Successful weight loss with self-help: A stepped-care approach. Journal of behavioral medicine 32(6): 503-509.
- Berkowitz RI (2013) Treatment of adolescent obesity comparing self-guided and group lifestyle modification programs: A potential model for primary care. Journal of pediatric psychology 38(9): 978-986.
- Latner JD (2007) Self-help for obesity and binge eating. Nutrition Today 42(2): 81-85.
- Latner J (2001) Self‐help in the long‐term treatment of obesity. obesity reviews 2(2): 87-97.
- Mahoney MJ (1974) Self-reward and self-monitoring techniques for weight control. Behavior Therapy 5(1): 48-57.
- Epstein LH (2004) The effect of reinforcement or stimulus control to reduce sedentary behavior in the treatment of pediatric obesity. Health Psychology 23(4): 371-380.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...

.png)


