Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1644
Research ArticleOpen Access
Sexual Assaults at The Saint-Louis Regional Hospital Center in Northern Senegal Volume 2 - Issue 5
Aliou Diouf1,2, Ousmane Thiam1, Mamour Guèye2, Mame Diarra Guèye2, Djibril Bahaid Sow1, Cherif Tourad Sarr1 and Magatte Mbaye3
- 1Regional Hospital Center of Saint-Louis, Senegal
- 2Gynecological and Obstetric Clinic, Senegal
- 3Gaston Berger University, Senegal
Received:June 24, 2020; Published: July 16, 2020
Corresponding author: Aliou DIOUF, Gynecological and Obstetric Clinic, EPS Aristide Le Dantec Regional Hospital Center of Saint- Louis, Senegal
DOI: 10.32474/OAJRSD.2020.02.000149
Abstract
Objectives: Specify the epidemiological characteristics and evaluate the management of victims of alleged sexual assault.
Patients and methods: This is a retrospective study of all cases of suspected sexual assault received at the Saint-Louis regional hospital center in the period from December 1, 2015 to November 30, 2005.
Results: The number of patients was 95, or 1.8% of admissions. 92.6% of the victims were received with a judicial requisition. The average consultation time after the assault was 10 days. The victim’s epidemiological profile was that of an adolescent girl, on average 14 years old, without any pregnancy in 86.2% of cases. The perpetrator’s profile was that of a 32-year- old man, belonging to the victim’s entourage in 75% of the cases (spiritual guide, roommate, family friend...). The mode of sexual abuse was genitogenital contact in 72.7% of cases and unprotected (97.6%). Clinically, 40% of the patients had signs of recent genital trauma and 60% of the hymenal lesions were old. HIV serology returned positive in two cases. During the follow-up, three pregnancies had occurred and only 9.1% of the victims had benefited from psychological assistance.
Conclusion: Sexual abuse is currently a real socio-cultural drama. Preventing them involves raising public awareness. Their management must be early and appropriate in order to prevent sexually transmitted infections and psychological consequences.
Keywords: Sexual Abuse; Genital Trauma; Saint-Louis
Introduction
Sexual abuse or sexual assault is defined by the French penal code in its article 222-22 as being any sexual attack committed with violence, coercion, threat, or surprise on the person of others [1]. Senegal’s penal code rather deals with rape, which is part of sexual assault. It is article 320 of the penal code which defines rape: “Any act of sexual penetration, of whatever nature, committed on the person of others by violence, coercion, threat or surprise is rape” WHO in its World Report on Violence and Health defines sexual violence in these terms “any sexual act, attempt to obtain a sexual act, comments or advances of a sexual nature, or acts aimed at trafficking or otherwise directed against sexuality of a person using coercion, committed by a person regardless of their relationship to the victim, in any context including, but not limited to, home and work. ” This definition therefore includes rape or attempted rape whether outside marriage or not; also included sexual harassment, forced marriage, denial of the right to use contraception or to protect oneself from sexually transmitted infections, forced abortion, or forced prostitution without restriction of age or sex. Mainly two criteria come out of this definition of sexual violence: on the one hand the type of sexual relationship which can be contact, attempts, touch, penetration; on the other hand the degree of coercion such as unwanted or forced sexual expressions [2]. Sexual abuse remains a major public health problem; thus, in the world on average one woman in five would be victim of rape or attempted rape during her existence after a study conducted by Marie José Alcala in 2005 [3]. According to the “RAINN (Rape, Abuse, Incest, National, Network)” and the “Justice Bureau Statistical Bulletin” in the United States in 2004-2005, 64,080 people were victims of rape, 51,500 of attempted rape, one person every two and a half minutes [4, 5]. LESERMAN J of the University of North Carolina reports that 15% to 25% of the general female population have a history of sexual violence in the United States [6]. In Europe, mainly in France during the year 2000, a national statistical survey carried out by the INED (National Institute for Demographic Studies) reported that out of 6,970 women aged 20 to 59 and 1.2% declared that they had suffered during the year 1999 at least once sexual touching, an attempted rape or non-rape, the latter would concern 0.3% of women declared to the general population which represented 48,000 rapes per year in France in this segment of age [7]. In 2007, the Research, Studies, Evaluation and Statistics Department (DREES) reported 1% to 2% of rape cases in France [8].Sexual abuse seemed more frequent in Europe than in Africa, but in recent years, cases of sexual abuse are more and more reported in Africa but are characterized by the difficulty of their cost in charge because of the scarcity of structures specialized in this field. Despite the fact that attendance at a large mediation of sexual abuse, most of the available data underestimate the extent of the phenomenon due to the scarcity of hospital studies on the subject. The purpose of this study was to clarify the epidemiological, clinical, paraclinical and medico-legal aspects of sexual abuse in the Saint-Louis region and to propose recommendations with a view to improving the cost of care for victims.
Patient and Method
This study took place over a period of 3 years, from December 1, 2015 to November 30, 2018 at the Regional Hospital Center of Saint-Louis which is a reference center in the northern area of Senegal. It was a descriptive study with retrospective recruitment of any patient admitted on the grounds of sexual abuse.
For each case, the following parameters were analyzed:
• epidemiological characteristics (age, number of
pregnancies);
• parity and place of residence;
• the circumstances of the assault and the characteristics of
the assailant
• the type of sexual contact;
• any lesions found during the physical examination;
• psychological impact;
• the results of the paraclinical assessment;
• the treatments administered;
• the judicial outcome.
The photographs of the lesions observed in the victims were used as a forensic document. The data was collected using a survey sheet and analyzed first on Microsoft Excel 2016 and then using SPSS 24 Mac version software.
Results
Frequency
We collected 95 cases of sexual abuse among the 5,412 patients admitted to gynecological emergencies during the study period, a frequency of 1.8%.
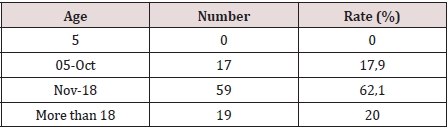
Sociodemographic Data Age
The average age of our patients was 26 years with extremes of 6 and 31 years (Table 1). Girls under the age of ten were 15% represented. Patients between ten and 20 years of age were the most represented (68%) and only one patient was over 30 years of age. More than half of the patients (54.4%) were in the pre-pubertal period and 45.5% in the period of genital activity.The victims were mostly single (92.6%), 7.4% of whom were divorced and 1.8% were widows. Married women and victims of sexual abuse were 7.4%.
Gravidity and Parity of the Victims
Women without any pregnancy represented almost all of our patients (86.3%). There were 2 victims with one to three pregnancies (2.1%). The distribution of patients according to parity showed a large majority of nulliparous women (98.2%). Only one patient had 2 deliveries.
Place of Residence
More than half of the patients (58.2%) lived in the city of Saint- Louis and the surrounding area. The rest (27.4%) came from other departments in the region.
Circumstances of the Aggression Time and Place
More than half of the victims (58.2%) had been assaulted between 7 a.m. and 7 p.m., therefore during working hours. Ten patients (10.5%) were attacked between 6 p.m. and 9 p.m. and 11 (11.57%) between 9 p.m. and midnight. In more than three-quarters of the cases (78.2%), the sexual abuse was committed in a place familiar to the victim (school, grocery store and beach).
Type of Sexual Contact
The most frequent type of sexual abuse was genito-genital contact with penetration for 72.7% of the workforce and with ejaculation in 9.3%. The other victims had suffered sexual touching (32.7%). The notion of wearing a condom was only found in one patient. Characteristics of the aggressor and links with the victim. The sexual assault was perpetrated by a single individual in the vast majority of cases (92.4%), while it was collective for eight patients (7.6%). In the majority of cases (60.3%), the abuser had no connection to the patient. However, in 24.3% of the cases, he was part of the family circle or considered as a friend (14.1%) or as a spiritual guide (1.3%).
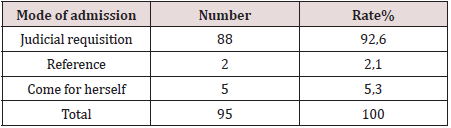
Clinical and Paraclinical Aspects Mode Of Admission
The majority of victims were subject to a judicial requisition (92.6%). 5 patients (5.3%) came on their own and 2 were referred to our structure (2.1%) (Table 2).
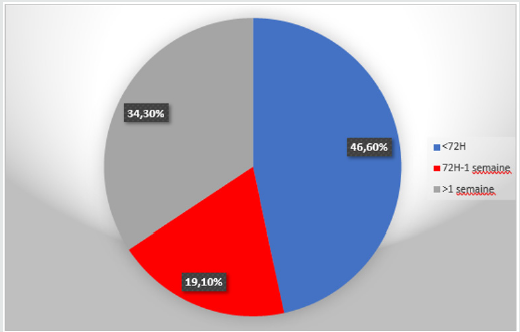
Consultation Period
The average consultation time was 10 days with extremes of two hours and two years. The majority of victims were received within 72 hours of the incident (46.6%). Similarly, more than a third of patients (34.3%) had seen more than a week after the sexual abuse (Figure 1).
Psychological State
On admission, patients displayed either aggression (5.5%), fear (5.5%), mutism (23.6%) or indifference (27.2%). In 38.2% of cases, the patient’s psychological state had not been assessed.
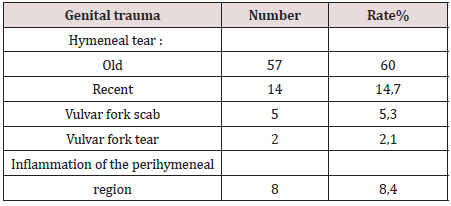
Genital Trauma
15 patients (15.8%) had signs of genital trauma, including tears in the vulval fork (2 cases), scrapes (5 cases) or inflammation (8 cases). The hymen was found to be intact in 25.3% of the cases. Hymeneal lesions were found in 74.7% of our patients and these were mainly old lesions (60%) (Table 3).
Bacteriology and Serologies
Bacteriological examinations of vaginal swabs returned
positive in 27.3% of cases. The main germs encountered were
Escherichia coli (33.3%), Candida albicans (26.7%) or Gardnerella
vaginalis (20%) alone or in combination. 2 cases of HIV infection
were diagnosed (2.1%).
They were two girls, 10 and 12 years old. They were not able
to benefit from a serological check three months after the first
samples. The HbS antigen was found in 2 patients (2.1%).
Therapeutic aspects
Half of the patients (50%) had received antibiotic prophylaxis. Emergency contraception was introduced in 29.2% of the cases, with one failure, however, which motivated a clandestine induced abortion. Two patients admitted with a full-term pregnancy had undergone a cesarean section for an immature pelvis and a third patient had been referred to us in the postpartum for infanticide. 8 patients (8.4%) had received surgical treatment mainly represented by sutures of perineal, vulvoperineal or vaginal tears. All the victims had been referred to a psychiatrist, but only 6 of them were able to receive adequate psychological care (6.3%).
Judicial aspects
In the majority of cases (60%), there had been no legal proceedings and the families of the victims had settled out of court. Among the other patients (40%) who had filed a complaint, we noted a sentence of four years’ imprisonment in 6 cases.
Discussion
Analysis of our results shows that the incidence of sexual assault (1.8%) is relatively low in our hospital practice compared to that reported by other African authors [7]. In Mali, Traoré reported a rate of 2.4%. Marsaud reports, in a study carried out in a large South African center specializing in the care of victims of sexual abuse, that 53% of the country’s female population has suffered at least one sexual abuse [6]. The same observation was made in Uganda where a study carried out by “Women Vision” in 1999 estimated this rate at 12% [7]. It should be noted that South Africa is the country in the world with the highest number of reports of sexual abuse. The lack of awareness of our populations for reporting cases and for early consultation and the influence of religion and socio-cultural principles make sexual abuse a taboo subject. In developed countries, the data reported in the literature comes mainly from specialized centers, judicial sources and population research centers. This is how Lisak and Miller [9], in the United States, reported a frequency of 39% of sexual abuse in 2002 on the whole population; in France the rate would have gone from 0.8 to 1.2% from 1997 to 2000 [3]. The young middle age in our study is comparable to that found in an earlier Dakar study [10]. It is similar to that found in the American series [11,12]. and that of Daligaud and Gonin [10] in France. Patients were older in the Hilde and Sylla series whose study populationwas represented by victims of domestic violence and sex workers. Our study thus confirms that sexual abuse concerns significant proportions of children and adolescents [6-13]. Most of our patients lived in and around the city of Saint-Louis, which reflects a low socioeconomic level, a low level of education and a situation of promiscuity. This promiscuity probably explains that 39.7% of the patients knew their attacker, who was either a member of their entourage, a family friend or considered a spiritual guideThe precariousness in which families live often justifies the lack of education and the exercise of small trades such as that of saleswoman or domestic worker who expose them to sexual abuse [13]. Thus, most authors have identified as risk factors for sexual abuse the lack of communication between parents and their children on sexuality which is often considered taboo, poor socio-economic conditions and family disorganization (divorce, parents singles). Other factors, such as family stability, parental experience and good socioeconomic status have been classified as “protective” [8]. This notion of familiar links between victims and their aggressors, which is frequently found, contributes to an underestimation of the frequency and complexity of the care of young victims whose parents often prefer not to have recourse to health and judicial structures in order to preserve the “family fabric”. As we have noted, many authors report that sexual assault often takes place during working hours, particularly in schools [8]. Unlike the South African [6] and Ugandan [7] series, which report respective rates of 25, 39 and 75%, collective abuse is less frequent in our context (7.6%). As for the type of sexual contact, we find like Traore that it is most often genito-genital (72.7%) with vaginal penetration. We found 5.5% of genito-anal contact and 3.6% of genito-oral contact against 1.7 and 0.9% respectively in Traoré. This trend is different from that found in the western environment, where touching and raping generally have an equal distribution [13,14]. During these sexual assaults, the use of condoms was rare (1%) as noted also in Cameroon with 1.3% [13]. This underscores the need to systematically prevent the occurrence of STIs and HIV infection in victims through appropriate and early drug prophylaxis as well as emergency contraception. On the clinical level, the interrogation made it possible to find that more than a third of the patients had been systematically referred to the referral hospital without a referral slip after a first consultation in a private structure or a health center. Most providers preferred to refer victims of sexual abuse often out of reluctance or incompetence. This contributes to delaying care and highlights the importance of training staff. Thus, the average consultation time after the sexual assault was 10 days, and only 29.6% of the patients had come in the first 24 hours. This low rate of early consultation is comparable to that of Traore which was 32.7%. On the other hand, in France, the average consultation time is estimated at 48 hours [1]. The delay in consultation seen in Africa and particularly in West African series, is partly justified by the socio-cultural realities of our society which still considers sexual abuse as a dishonor. Victims and their families therefore often hesitate, out of shame or indecency, to resort to health facilities and the judicial authorities for the sake of preserving the honor of the family. On the other hand, in Europe, the victims can be treated with discretion in specialized structures [14]. These structures, outside of South Africa and Cameroon, are almost nonexistent in Africa.On gynecological examination, old hymeneal lesions ranked first (60%) contrary to the data in the literature according to which recent lesions are the most common, between 60 and 76.9% of cases [6,15]. This difference seems to be linked to the fact that the consultation period was much longer in our series, knowing that the hymenal lesions heal quickly in five to seven days after the attack [16]. Regarding the psychological aspect, the reactions observed in the victims are similar to those usually described by other authors like Marsaud [17] who noted psychological disorders in65% of victims of sexual abuse. These figures show that sexual abuse can be the cause of more or less serious psychological disorders. It is to be deplored that in Africa, there are very few studies which give information on the psychological repercussions of sexual abuse. The absence of specialized centers for victims results in a weak integration of the psychological component in a more general framework of multidisciplinary care. Our low rate of psychological care (9.1%) of cases, joins the data of the African literature with 7.9% [13]. On the other hand, it is systematic for South African and Western authors, because it makes it possible to significantly reduce the posttraumatic sequelae of the sexual assault and to guarantee the victim’s long-term recovery [6-19]. This disparity is due to the nonexistence in our developing countries of care and assistance units reserved only for victims of sexual abuse where psychologist or psychiatrist, gynecologist, forensic expert and laboratory team collaborate in a multidisciplinary way. We have identified two cases of HIV infection in two girls, 10 and 12 years old, respectively, whose infection was probably prior to the attack, since the test was taken three days after the sexual abuse. This poses the problem of repeated and chronic sexual assault among young victims. Many cases of HIV / AIDS infection after rape have been reported, notably in South Africa (78%) and Cameroon 33.8% [5-13]. This underscores the value of instituting prophylaxis of HIV infection by triple therapy within 72 hours of the sexual assault, all the more so since access to these ARVs has been improved. However, a limitation in our study was the lack of reassessment of the patients’ HIV status three months after the sexual abuse. Concerning the prevention of pregnancy, which must be systematic in any victim during the period of genital activity, only 25.5% of our patients had been able to benefit from emergency contraception because the majority of our study population was represented by pubescent subjects. Regarding legal proceedings, we found, like Sylla in Mali, that in almost half of the cases (40.8%), the parents opposed legal proceedings. Indeed, they most often withdrew their complaint after an amicable settlement. In contrast, in Uganda [7], court complaints are frequent (85%), but judicial investigations rarely result in the arrest of the attacker (s).
Improving care in our country should also go through better administrative and psychological support for victims and their families.
Conclusion
Sexual assault is currently a real scourge, but its real prevalence remains underestimated in our country. This work shows that they mainly concern children and adolescents living in disadvantaged areas who are thus exposed to a sexually transmitted infection and in particular to HIV / AIDS. The quality of their care in Senegal also suffers from many shortcomings. Improving the treatment of victims of sexual assault necessarily involves training staff, midwives and doctors, the full assessment of patients, the drafting of medical reports and the creation of centers reception, information, orientation and care for victims of sexual abuse and their families in a multidisciplinary framework. At the same time, information and awareness campaigns for people in disadvantaged areas should be organized in order to promote systematic reporting of cases and early consultation. Better quality of care also involves promoting schooling and education for girls in order to prevent them from becoming precarious, revising the medico-legal framework for the termination of pregnancy and increasing the criminal sanctions imposed on perpetrators. Finally, a national survey is needed to estimate the real prevalence of sexual assault in Senegal.
References
- AciernoR,ResnickH, KilpatrickDG(1999) Risk factor for rape, physical assault, and post-traumatic stress disorder in women examination of differential multivariate relationships. J Anxiety Disord13(6):541-563.
- AdamsJA, WellR(1993) Normal versus abnormal genital findings in children: how well do examinants agree ? World Health Organ17(5):663-75.
- BarretP (2004) Agressionssexuelles. In: Mises à jour en gyné- cologie obstétrique ;Collègenational des gynécologues et obstétriciens fran ais. Paris: Éditions Vigot p. 275-281.
- BasileK, SaltzmanL (2002) Sexual violence surveillance: uniform definitions andrecommended data elements version 1.0 Atlanta: centers for diseases control and prevention. J Natl Cent InjPrev Control11:532-540.
- BergerD (2000)Violencessexuelles: conduiteà tenir en pré- sence d’une victime d’agression sexuelle. In: Mises à jour en gynécologie obstétrique; Collège national des gynéco- loguesetobstétriciens fran ais. Paris: Éditions Vigot p. 282-284.
- BugsS (2000)Contraception, IVG, grossesse: question de l’IVG et les nouveaux croisés de l’ordre moral. Grenoble: Édition Thotp.242.
- Cazanave-RobertA, MillotC (2003)Réflexion et mise en place d’un cadre d’accueil pour enfants victimes d’abus sexuels à l’hôpital St-Vincent-de-Paul. Ann Fr Psycholp. 105-10.
- Code de procédure pénale du Sénégal : ministère de la Justice duSéné
- LisakD, MillerP(2002) Repeat rape and multiple offending among undetected rapists:violence and victims. Am J Obstet Gynecol17(1):73-84.
- DaligaudL, GoninB(1999) Les violencessexuelles. J Androl Lille9:519-527.
- DioufA, GayeA, SangareM, PM Moreira, JCMoreau, et al.(1995)Priseen charge des présuméesvictimesd’agressionsexuelleà Contracept Fertil Sex23:267-270.
- ElliotD, BriereJ(2004) Adult sexual assault: prevalence, symptoma- tology and sexdifferences in the general population. J Trauma Stress17(3):203-211.
- JaspardM (2001)Nommer et compter les violences envers les femmes : une première enquête nationale en France. Popul Soc364:1-4.
- HolmesM (1999) Sexual transmitted infections in female rape vic- tims. J AIDS Patient Care STDS13(12):703-708.
- MbassaM, NgohF (2003) Séroprévalence de l’infection à VIH chez les enfants victimesd’abus sexuels au Cameroun. Med Trop63(2):155-158.
- RickertV, WiemannC, VaughanR(2004) Rates and risk fac- tor for sexual violence among an ethnically diverse sample of adolescents. Arch PediatrAdolesc Med158(12) 1132-9.
- MarsaudO (2001) Les viols, plaies des écoles sud-africaines. OMS, Avrilp.222-230.
- SoutoulJ, FrogeE (1980) Traumatisme de l’appareilgénital et du périnée chez la femme. EMC (Elsevier, Paris), gyné4.
- TjadenP, ThoennesN (2000) Full report of the prevalence, inci- dence, and consequences of violence against women: findings from the national violence against women survey Washington (DC): National Institute of Justice, NCJ183721.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...