
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1644
Research ArticleOpen Access
Anomalies Associated with Gastroschisis and Omphalocele in Villa Clara, Cuba: a 30-year series from 1990 to 2019 Volume 3 - Issue 1
Noel Taboada Lugo1, Ana E. Algora Hernández1, Manuela Herrera Martínez1, Gisela Noche González1, María E de la Torre Santos1, Lorna González Herrera2, Eliecer Anoceto Armiñana3 and Ismary Oliva Machado1
- 1Department of Medical Genetics, Villa Clara Medical University, Cuba
- 2Department of Radiology, Villa Clara Medical University, Cuba
- 3Department of Pathology, Villa Clara Medical University, Cuba
Received:August 17, 2020; Published: September 11, 2020
Corresponding author: Noel Taboada Lugo, Department of Medical Genetics, Villa Clara Medical University 18th Libertadoresst, Santa Clara city, Cuba.
DOI: 10.32474/OAJRSD.2020.03.000151
Abstract
Background: Gastroschisis and omphalocele are the most common anterior abdominal walldefects. The aims of our study were to describe the prevalence trends of congenital anterior abdominal wall defectsand to determine the frequency and type of associated congenital anomalies in gastroschisis and omphalocele cases.
Methods: A retrospective, observational study, with data obtained by theCuban Registries of Congenital Malformations; was conducted in the Cuban province of Villa Clara from 1990 to 2019.
Results: A total of 158 cases with anterior abdominal wall defect were identified, 93 of them (59%) with gastroschisis and 53 with omphalocele. There was an increasing trend in the prevalence rate of the anterior abdominal wall defects during the study timeframe, mainly in gastroschisis prevalence. The prevalence rate of gastroschisis (per 10,000 live births) during the study time frame was two fold those of omphalocele (4.8 and 2.7 respectively). The majority of GS cases did not have additional anomalies (80/93 [86%]). There was a statistically significant difference between the proportions of isolated and associated cases. (p= 2, 2E- 08). Omphalocele cases were more likely to be diagnosed with at least one other CD than those with GS (25/53 [47%] vs. 12/93 [13%].
Conclusions: Arisein anterior abdominal wall defects prevalence has been noted in recent decades in Villa Clara province. The present study revealed that omphalocele cases were more likely to have other congenital anomalies, predominantly in musculoskeletal and cardiovascular systems.
Keywords: Abdominal wall defects; Gastroschisis; Omphalocele; Anomalies; Cuba
Introduction
Anterior abdominal wall defects are a common cause of morbidity and even mortality. These include the most common congenital anterior abdominal wall defects (AWD): gastroschisis (GS) and omphalocele (OM) or exomphalos.GS is a congenital defect (CD) where the small intestine, part of the large intestine and occasionally other abdominal organs protrude through a lateral defect in the ventral abdomen without any protective membrane, whereas OM is an amnion covered sac enclosing a range of viscera from a few loops of midgut to the entire midgut, liver and spleen. GS usually is an isolated defect, whereas OM is often seen in association with chromosomal and other systemic congenital defects (CD) (1-3). Villa Clara province is located in the central region of the Cuban archipelago, with a superficial extension of 8 411, 81 square kilometres, occupying the fourth place among the fifteen Cuban provinces and representing the 7.6% of the total area of the country (4). With this study we aimed to describe the prevalence trends of AWD and to determine the associated anomalies that have been identified in GS and OM cases and to provide an insight into the more affected system of organs.
Patients and Methods
This retrospective, observational study was performed from January 1, 1990, to December 31, 2019 with data obtained by theCuban Registry of Congenital Malformations and by the Cuban Prenatal Congenital Malformations Registry (RECUMAC and RECUPREMAC respectively, for their names in Spanish), a multicenter, hospital and community-based registers, which recorded all pre- and postnatally detected congenital defects. Data about associated congenital defects were obtained besides the US and post-mortem reports, from the Pathology Department of the Provincial Maternity Hospital “Mariana Grajales”, where all anatomopathological macroscopic and microscopic studies were performed. We evaluated data from all cases diagnosed with either GS or OM. All cases were classified in isolated when no other congenital defects were observed neither by US, physical examination nor autopsies. The associated congenital defects were counted in each affected system. All cases of other AWD rather than GS or OM were not included. The prevalence rate at birth of AWD was calculated by dividing the numerator (registered cases of live birth (LB), stillbirth or elective pregnancy terminations) by the denominator (total number of live births in the studied period). The prevalence rate was expressed as the number of cases per 10,000 LB. We conduct a statistical hypothesis test on the basis of the results of the Z test to compare proportions. P value <0.05 was considered statistically significant. Statistical analysis was done using SPSS Version 22software. This study is based on an analysis of existing registered data, which were anonymously collected, according the ethical issues on human investigations. It was approved by the Ethical Committee of the Biomedical Research Unit of the Villa Clara Medical University, following the World Medical Association Declaration of Helsinki.
Results
A total of 158 cases of AWD were recorded, of these, 93(58.9%) were GS, 53(33.5%) were OM, whereas 12/158 (7.6%) where other AWD not included in the present study. The cases were ascertained from 193 916LB. The overall prevalence of AWD (per 10,000 LB) was 8.15, meanwhile the prevalence of GS and OM was 4.80and 2.73, respectively. That is, one case of GS in 2085 LB, whereas OM was found in 1: 3658 LB.
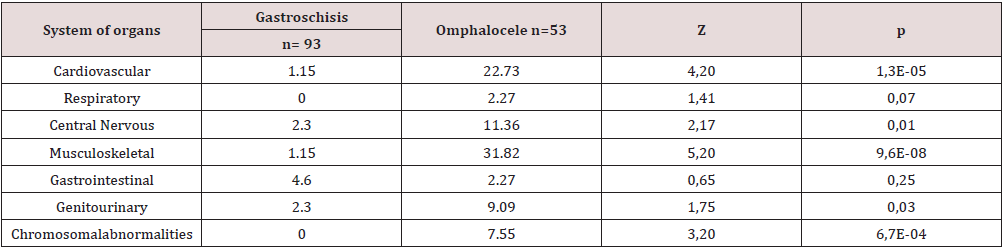
(Figure 1) shows an increasing trend in the prevalence rate (per 10,000 LB) of AWS over the thirty studied years in Villa Clara, from 3.83 in 1990 to 7.47 in 2019. The GS prevalence was over the OM prevalence most years during the study timeframe. A temporal cluster of GS was observed in year 2006 (8 GS cases, and the highest prevalence rate: 17.92per 10,000 LB). The majority of GS cases did not have additional anomalies (80/93 [86%]). There was a statistically significant difference between the proportions of isolated and associated cases. (p= 2, 2E-08). Meanwhile, (30/53 [57%]) of OM cases had associated CD, although, there were not statistically significant differences between these proportions (p=0, 18). We identified 71 associated CD in 43/146 [49%]) cases of GS and OM. In 13/93 [14%]) of GS cases and in 30/53 [57%]) of OM cases at least one associated CD was observed. (Tables 1). Of the 43cases with associated CD, 13 (30%) had more than one CD. OM cases were more likely to be diagnosed with at least one other CD than those with GS (25/53 [47%] vs. 12/93 [13%]. This was true for most categories of involved system of organs, which all shown statistically significant differences, but respiratory and gastrointestinal (Table 2). One-half of cases with associated CD affecting Central Nervous System had Neural tube defects (5/10) and most of three quarters of them (4/5 [80%] were identified among OM cases and interestingly, all cases with chromosomal abnormalities were observed among OM cases (4/53[8%], including three cases with Trisomy 13 and another with Triploid.
Figure 1. Prevalence trends of gastroschisis, omphalocele and the total of congenital abdominal wall defects in Villa Clara, Cuba. 1990- 2019.

Table 1: Distribution of gastroschisis and omphalocele cases according the presence or not of associated congenital defects. Villa Clara, Cuba.1990- 2019.
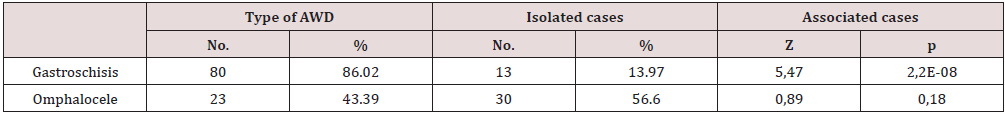
Table 2: Proportion of associated congenital defectsobserved per system of organs in gastroschisis vs. omphalocele cases. Villa Clara, Cuba.1990- 2019.
Discussion
The prevalence rate of GS (per 10,000 live births) during the study time frame was two fold those of OM (4.8 and 2.7 respectively). It is consistent with trends widely described in the literature, where is stated that prevalence of GS in recent decades shows worldwide remarkable and worrying increasing trend, suggesting role of environmental factors (1, 5- 7). From an incidence of 0.06–0.8per 10,000 in the 1960s, GS has become more prevalent over the last few decades to its current rates of 4.5–5.13 per 10,000 pregnancies (5). The prevalence rates (per 10,000 LB) of GS and OM in our series are consistent with Schmieding (8) who reported 4–5 for GS and 2 for OM, and almost the same prevalence as Stalling (9) found for a larger series in the USA (4.3 for GS and 2.1 for OM). Otherwise, the lowest prevalence rates (per 10,000 LB) of GS worldwide had been described in Asian countries. In the Liaoning province in China, the prevalence of GS was 2.30 in a series of ten years of study and 0.50 in Taiwan and Japan, respectively (10-12). In our series, 86% of GS were isolated and the remaining 14% had associated CD; this is also consistent with other series, where the incidence of associated anomalies in GS varies from 5 to over20% (13- 15) Reported associations include cardiac abnormalities and increased prevalence of central nervous system anomalies(amyoplasia), and limb and kidney anomalies and may influence the prognosis of the child with GS significantly (13) In a study conducted by Given, et al. (16) using data from 18 European congenital anomaly registries, they identified 1577 GS cases, 83.0% of which were isolated. The higher frequency of isolated GS cases than of those with associated CD has been shown in other series as well. (17) However, in a study conducted in a Mexican hospital, 52/108 (48%) of infants with GS had one or more associated anomalies, for 1.4 associated defects per case (18). We found the most frequent associated CD in GS cases affecting the gastrointestinal system. Intestinal atresia has been reported in up to 25% of GS cases in some series, and especially when the bowel was thickened and coated (15) Similar to prior reports, we observed that OM cases were more frequently diagnosed with associated CD compared with those with GS. Musculoskeletal and cardiac anomalies were the most prevalent associated CD found in OM cases in our study, which is consistent with the literature, where its claimed that neonates with OM have higher rates of death compared to neonates with GS, this difference in mortality is thought to be related to the high incidence of associated CD and specifically, cardiac abnormalities among neonates with OM (19). In our series, 57% of OM cases had associated CD. These findings are consistent with other reports of prenatal diagnosis and management of OM where is stated that about 40–80% of all OM cases would have at least one concurrent anomaly. Associated anomalies include cardiac (7-47%), gastrointestinal (3-20%), genitourinary (6–20%), chromosomal (3-20%), musculoskeletal (4-25%) and central nervous system (4- 30%) (2). There is a known association between genetic disease and OM. We found 8% of chromosomal abnormalities among OM cases. This frequency is lower than the reported in a singlecenter study of AWD prenatally diagnosed, where chromosomal abnormalities were found by karyotype in 8/29 (28%) fetuses with OM (20). To the best of our knowledge this is the first study conducted in Cuba including a large series of years to determine the frequency and type of associated congenital anomalies in GS and OM cases. Limitations of our study include lack of data regarding number of stillbirths during the study timeframe, for that reason when prevalence rate was estimated; in the denominator only live births were included, and the limited number of chromosomal studies performed to the AWD cases. In conclusion, a rise in AWD prevalence has been noted in recent decades in Villa Clara province. The present study revealed that OM cases were more likely to have other congenital anomalies, predominantly in musculoskeletal and cardiovascular systems.
Conflict of Interest Statement
The authors declare no potential conflict of interest.
Funding statement
Authors received no economical support.
Acknowledgments
We thank all those who contributed to the RECUMAC and RECUPREMAC registers from 1994 to 2019. The authors are grateful for the valuable comments and statistical assistance provided by Dr. Roberto LardoeytFerrer from the Habana Medical University.
References
- FeldkampML, ArnoldKE, KrikovS, ReefhuisJ, AlmliLM, et al. (2019)Riskof gastroschisis with maternalgenitourinary infections: the USNational birth defects prevention study 1997–2011. BMJ Open 9(3):
- VerlaMA, StyleCC,OlutoyeOO (2019) Prenatal diagnosis and management of omphalocele.SemPed Surgery 28(2): 84-88.
- KelayA, DurkinN, DavenportM (2016) Congenital anterior abdominal defects. Paediat Surgery 34 (12): 621- 627.
- Villa Clara Statistical Year book. National Office of Statistic and Information.ONEI 2018.
- MelovSJ, TsangI, CohenR, BadawiN, WalkerK,et al. (2018) Complexity of gastroschisis predictsoutcome: epidemiology and experience inan Australian tertiary centre. Pregnancy and Childbirth p.18:222.
- WissanjiH, PuligandlaPS (2018) Risk stratification and outcome determinants in gastroschisis. SemPed Surgery27(5): 300-303.
- MarshallNSG, FearonKM, GillMI, DeSouzaCJ, FearonIC, et al. (2017)Mortality-related factors in gastroschisis – a Jamaican perspective.JPed Surgery 52(4): 530-533.
- SchmeddingA, WittekindB, Salzmann-ManriqueE,SchloesserR, RolleU (2020) Decentralized surgery of abdominal wall defects in Germany. PediatSurgInternat36:569-578.
- StallingEB, IsenburgJL, ShortTD, HeinkeD, KirbyRS, et al. (2019) Population-based birth defects data in the United States, 2012–2016: A focus on abdominal wall defects. Birth Defects Res 111(18): 1436-1447.
- ChenMC, ChenJH, ChenY, TsaiYH, LeeCH (2019) Low and decreased prevalence of congenital abdominal wall defect in Taiwan. J Pediat Surg54(9):1958-1964.
- LiN, ChenYL, LiJ, LiLL, JiangCZ, et al. (2016) Decreasing prevalence and timetrend of gastroschisis in 14 cities ofLiaoning Province: 2006-2015. Scient Reports 6:33333.
- SuitaS, OkamatsuT, YamamotoT (2000) Changing profile of abdominal wall defects in Japan: results of a national survey. J PediatrSurg35(1):66–71.
- LapCC, BrizotML, PistoriusLR, KramerWL, TeeuwenIB,et al. (2016) Outcome of isolated gastroschisis; an international study, systematic review and meta-analysis. Early Human Develop 103: 209-218.
- TadepallyK, GattuV, VellankiS (2018) Gastroschisis and spine abnormality in fetus. Med J DY PatilVidyapeeth11:75-7.
- BeaudoinS (2018) Insights into the etiology and embryology of gastroschisis. SemPed Surgery 27(5):283-288.
- GivenJE, LoaneM, GarneE, NelenV, BarisicI, et al. (2017) Gastroschisis in Europe-A case-malformed-control study of medication and maternal illness during pregnancy as risk factors. Paed Perinatal Epidemiol, 39(6): 549-559.
- CoreyKM, HornikCP, LaughonMM, McHutchisonK, ClarkRH, (2014) Frequency of anomalies and hospital outcomes in infants with gastroschisis and omphalocele. Early Hum Dev 90(8): 421-424.
- CoronaRJR, NietGR, LópezME, MarureE, CárdenasRJJ, et al. (2016)Associated congenitalanomalies in infants with isolated gastroschisis: A single-institutionalexperience.Am J Med Genet Part A 170(2):316-321.
- RaymondSL, DownardCD, StPeterSD, BaergJ, QureshiFG, et al. (2019) Outcomesinomphalocelecorrelatewithsizeofdefect. SemPed Surgery 54(8):1546–1550.
- HidakaN, MurataM, YumotoY, HojoS, FujitaY, et al. (2009)Characteristics andperinatal course of prenatally diagnosed fetal abdominal wall defects managed in a tertiary centerin Japan. J ObstetGynaecol Res 35(1):40-47.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...



