Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4722
Research Article(ISSN: 2637-4722) 
Prevalence and Determinants of Low Birth Weight in Burundi: An Investigation from The National Demographic and Health Survey Volume 3 - Issue 2
Nadine Misago*1, Desire Habonimana2, Leopold Ouedraogo3 and Patrick Bitangumutwenzi4
- 1Health Healing Network Burundi
- 2Research and Innovation Unit, Department of Community Medicine, Faculty of Medicine, University of Burundi
- 3Reproductive, Maternal Health and Ageing Team, World Health Organization, Regional Office for Africa, Brazzaville, Republic of the Congo
- 4Department of Paediatrics, Faculty of Medicine, University of Burundi, Bujumbura, Burundi.
Received: February 06, 2021 Published: March 15, 2021
Corresponding author: Nadine Misago, Health Healing Network Burundi. Nadine Misago ORCiD: https://orcid.org/0000-0003-4436-7448 Desire Habonimana ORCiD: https://orcid.org/0000-0003-0832-5558 Leopold Ouedraogo ORCiD: https://orcid.org/0000-0001-5842-1842
DOI: 10.32474/PAPN.2021.03.000157
Abstract
Background: Birth weight is an important determinant of neonatal and child health outcome. For instance, evidence has shown
that low birth weight (LBW) has a negative impact on the baby’s growth, cognitive development, and on neuro-motor development
and immune function. Underweight babies are prone to increased risk of infections and stunting. LBW remains prevalent worldwide
and is more pronounced in low- and middle-income countries. Several factors including mothers’ socio-economic characteristics,
maternal health behaviors and maternal and pregnancy health conditions determine birth weight outcome. This study sought to
determine the prevalence and investigate determinants of LBW among Burundian women of reproductive age.
Methods: This study used data extracted from the 2016-2017 National Demographic and Health Survey (DHS) conducted on
7047 women who reported a live birth history in the five years preceding the survey and whose birth weight was recorded at
childbirth. The study used linear regression to explore socio-economic, maternal, and pregnancy related factors that determine
birth weight and further employed a logistic model to unpack factors with higher likelihood of LBW.
Results: Of 7,047 babies born between 2012 and 2017, 660 (10%) were underweight. Findings suggested that birth weight
decreases with older women’s age, multiple pregnancies (twin or triplet), and female babies. Conversely, birth weight increases
with a diabetes condition, wealthier quintiles, and higher party orders. Results from the linear regression were supported by those
implemented in the discrete model. In fact, higher parity orders and wealthier women were more likely to deliver normal weight
babies. High blood pressure, smoking, multiple pregnancies, and female child’s sex were negative predictors of normal birth weight.
For instance, twin babies were twice more likely to be underweight compared to single pregnancies.
Conclusion: This study unpacked high prevalence of LBW in Burundi and further highlighted areas of improvement to deliver on global neonatal and child health targets.
Results: From this work could be used to implement targeted interventions to reduce poverty, tackle chronic conditions in pregnancy, and reduce tobacco use among pregnant women as the above predicted LBW. Other interventions include modern contraception through health educational programs.
Keywords: Low birth weight; Determinants; Burundi
Introduction
Normal birth weight, defined as live-born neonates weighing from 2500 g to 4000 g at birth, is an important determinant of better neonatal and child health. Evidence has established the impact of low birth weight (LBW) on increased neonatal deaths and child stunting [1,2]. Furthermore, low-birth babies experience perinatal growth failure, reduced cognitive and neuro-motor functioning, and poor school performance [3, 4]. There exists a widening negative correlation between birth weight and children’s better health with extreme low-birth-weight babies experiencing major health conditions [4, 5]. Most importantly, underweight babies who survive tend to have impaired immune function and increased risk of disease; they are likely to remain undernourished, with reduced muscle strength, cognitive abilities, and intelligence quotient (IQ) throughout their lives [6]. Despite efforts to improve pregnancy experience and combat LBW, many countries still report high numbers of underweight babies until today. In 2012, the World Health Assembly (WHA) resolution set the goal to achieve 30% reduction in the number of LBW newborns by 2025 [7]. This target was further reemphasized by the Sustainable Development Goals (SDGs) agenda by setting an aim to “end all forms of malnutrition” including among pregnant women to “reduce neonatal mortality to at least as low as 12 per 1,000 live births and under-5 mortality to at least as low as 25 per 1,000 live births” [8]. Global efforts did not yield expected results as some countries continue to experience high rates of LBW.
Of about 21 million low birth babies – representing nearly 15% of all live-births worldwide – 19 million of too small babies are from Africa and Asia (excluding Japan). Altogether, more developed regions namely Northern America, Europe, Japan and Australia, and New Zealand account for less than 10% of low births [5]. According to available data, the whole sub-Saharan Africa excluding Rwanda suffers from LBW. Countries with higher LBW rates (15 to 20% of all live births) include Angola, Benin, Burundi, Botswana, Cote d’Ivoire, Guinea Equatorial, Madagascar, Namibia, Togo, and Western Sahara. Guinea Bissau exceeds 25% of LBW rate and is among the highest worldwide [5]. Despite Burundi having declined LBW from 17.4% [CI: 11.9–22.9] in the year 2000 to 15.1% [10.9– 19.4] in 2015; the country remains above the global average and is further top-ranked LBW rates [5, 9]. To better tackle LBW and deliver on maternal and children global targets, countries need to invest into evidence-based interventions that have been found to undermine childbearing and fraught with child growth among pregnant women.
An amounting evidence has established a causal link between a woman’s characteristics, maternal and pregnancy health conditions, and maternal health behaviors with birth weight outcome. For instance, WHO developed a framework that explains causal pathways for an increased risk of LBW. The framework comprises distal and proximal or immediate factors leading to small babies. Among distal determinants of LBW include
a) maternal characteristics such as extreme age, multiple
parity, poor birth spacing, and wealth index.
b) maternal health conditions namely chronic diseases
which have been found to increase maternal risk (i.e. high blood
pressure and diabetes).
c) maternal malnutrition characterized by anemia and
extreme maternal weight.
d) and other risk behavioral factors such as increased alcohol and tobacco consumption [5]. During the course of the pregnancy,
LBW can result from a premature birth (a birth occurring before 37
weeks of pregnancy) and/or the growth faltering in the mother’s
womb [5]. Other researchers of whom Alfred Kwesi Manyeh in
Ghana [10] and Getaneh Baye Mulu in Ethiopia [11] found similar
evidence. They both established the effect of the mother’s age,
wealth, parity, gestational hypertension, maternal height, antenatal
care (ANC), mother’s education attainment and the child’s sex
on birth weight [10, 11]. Furthermore, a study conducted on 10
developing countries incriminated the place of the woman’s age,
ANC, literacy level, body max index, and wealth on babies weight
at birth [12]. Despite the topic being of national focus today, little
has been done to explore factors leading to LBW in Burundi. The
aim of this study was to determine the prevalence and investigate
determinants of LBW in Burundi. Results of this study inform the
design of maternal and neonatal policies with an aim to deliver on
global and national targets by 2030.
Methods
Source of data
This study is a secondary data analysis using the Burundi Demographic and Health Surveys (DHS) 2017 datasets. To better understand predictors of birth weight, the study used women’s individual recorde dataset. This study used a sample of 7,047 women who reported a birth history during five years prior to the survey and whose information on birth weight was included in the dataset.
Outcome and explanatory variables
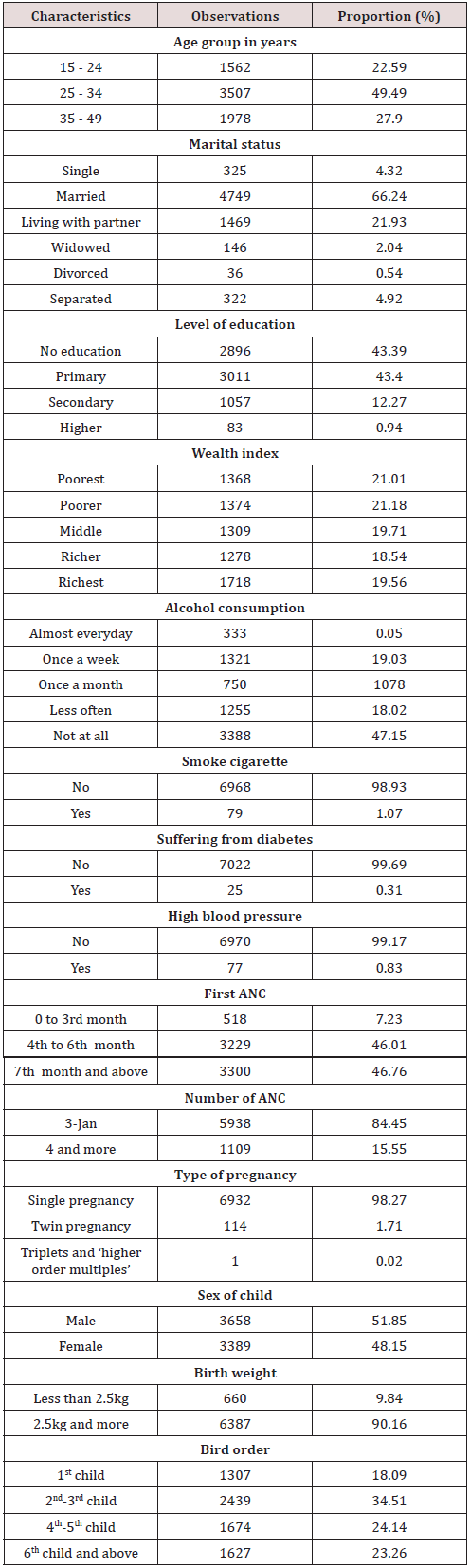
This study used “birth weight” as the dependent variable which was considered as continuous first to allow a linear regression analysis and again as dichotomous to enable the discrete model. We based on WHO guidelines to define cut-offs of the dichotomous “birth weight” outcome [13]. A dummy variable was generated taking value 0 for babies weighing less than 2,500 g at birth and value 1, otherwise. Selection of independent variables was informed by the literature search and by the understating of local context. We included individual woman’s characteristics, behaviors and underlying health conditions as well as factors related to pregnancy health. With an aim to better grasp the effect of coefficients on birth weight, all explanatory variables were categorized as summarized in Table 1.
Data management and models specification
In the first instance, owing to DHS study design which used multiple sampling stages, the dataset was survey set before analysis. In the second stage, we constructed the linear and logistic models as specified below:

In the above linear estimation, Yi is the outcome variable (i.e. birth weight). The model includes an intercept and a random error term. Independent variables are represented by a vector of covariates Xi and B1 captures the magnitude of change in birth weight corresponding to a unit change in explanatory variables. Significance of linear coefficients was ascertained based on p-value at α = 0.05.

Equation 2 is the logistic specification model. In this model, the dependent variable is the log odds that a woman i delivers a normal weight baby (i.e. a baby weighing at least 2,500 g) relative to those giving birth to underweight babies (i.e. babies with less than 2,500 g). 0 β captures fixed effects and 1 β detects random effects on the probabilities of giving birth to normal weight babies. The vector of covariates Xi includes independent variables described in Table 1. For the logistic model, significance of explanatory factors was determined based on a corresponding 95% confidence interval that does not contain value 1.
Results
Results of this study are sectioned into three main subheadings. In the first instance, we describe socio-demographic characteristics of study participants. In the second time, we summarize findings from the linear model of socio-economic and maternal health factors on birth weight. In the final stage, we present results of the logistic model on the probability of low versus normal birth weight.
Socio-economic characteristics
Table 1 summarizes socio-economic characteristics of participants. Of 7047 women of reproductive age, half were aged between 25 and 34 years old. Overall, majority of women did not achieve university education. Further, the prevalence of tobacco and alcohol consumption as well as the prevalence of health conditions with evidence to complicate pregnancy or childbirth was considerably low. Results also showed that mothers delayed in attending ANC as only about 7% attended their first ANC in the first trimester and only about 16% achieved recommended four or more ANC visits during the course of the pregnancy. More than half of surveyed women were married, and majority had a parity of two to three. Surveyed women were evenly scattered across the wealth quintiles. Low birth weight babies represented the vast minority (less than 10%) and male babies constituted a slightly higher proportion.
Determinants of birth weight
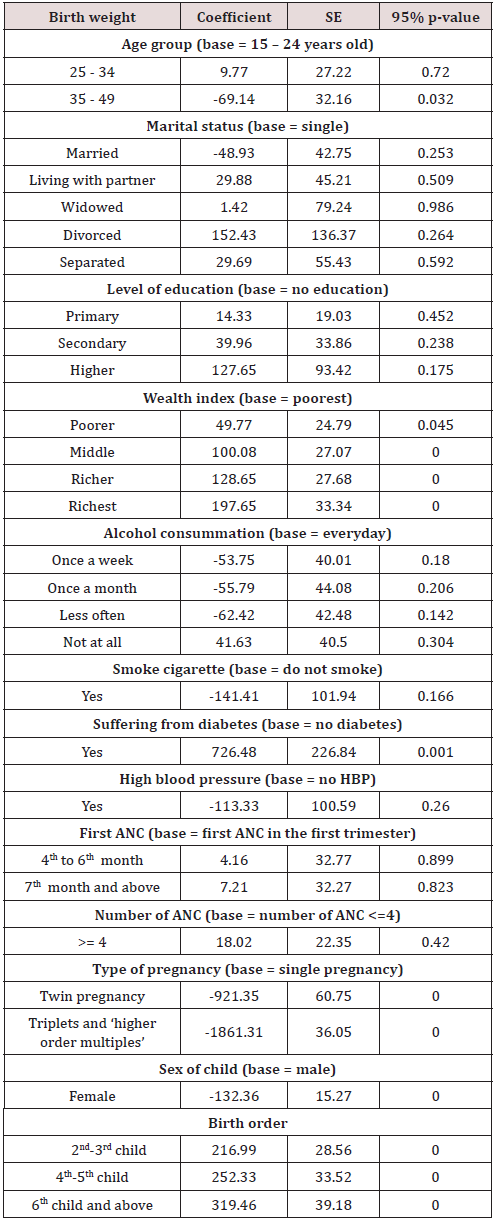
As can be viewed in Table 2 below, birth weight significantly decreases with older women’s age and increases with a diabetes condition. Also, there was evidence of a sharp increase in birth weight with wealthier quintiles. For instance, women who belong to the richer and richest quantiles gave birth to babies with almost 130 grams and 200 grams more; respectively. Moreover, there was a significant increase of birth weight with party. Mothers who had four to five and six and more parity gave birth to babies with 253grams and 320 grams more respectively. Most importantly, diabetic women gave birth to babies with 750 grams more compared to women without diabetes condition. The effect of a woman’s age on birth weight is linearly negative with a 70 g decrease for women above the age of 35 years. In contrary to the above, multiple pregnancies and female babies are associated with low birth weights. The decrease in birth weight is more evident for triplet pregnancies; reaching nearly 1800 grams lower compared to single pregnancies. The decrease in birth weight halves from triplet to twin pregnancies (1800 versus 900 grams). In the same perspective, female births tended to yield lower birth weights up to 130 grams less compared to male babies.
Determinants of low birth weight
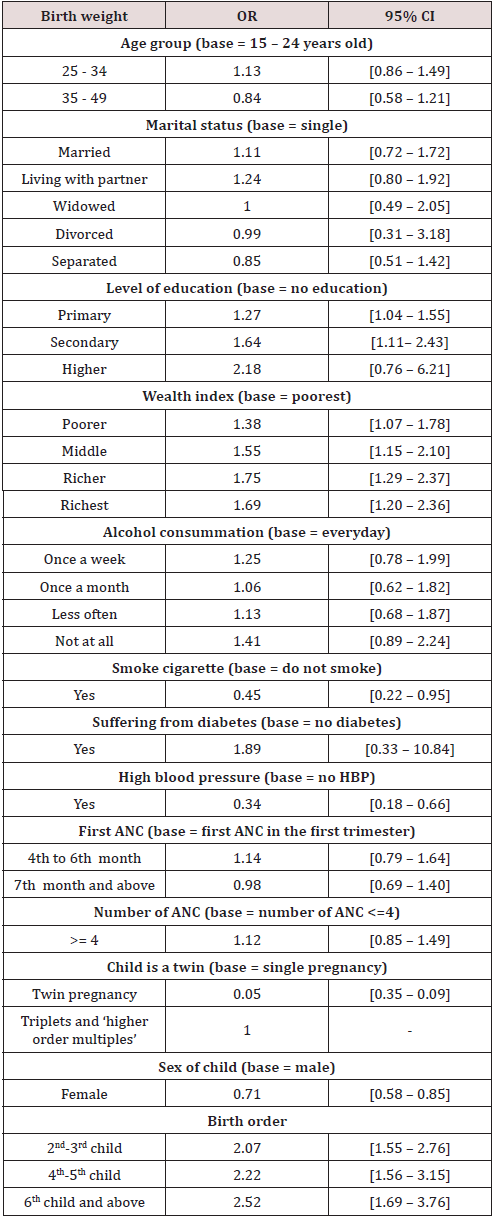
On the one hand, women’s education attainment, parity, and wealth index were predictors of higher likelihood of normal birth weight. With reference to poorest women, the likelihood that a woman gives birth to a normal weight baby increases with wealth quintiles to nearly double for women belonging to richer quantiles. Similarly, higher education level predicted higher likelihood of normal birth weight. For instance, women who attained tertiary education were about twice more likely to deliver normal weight babies compared to their counterparts who did not attend schooling. Furthermore, compare to women with one parity, the likelihood that a woman gives birth to a normal weight baby increases with high parity to become two times more and nearly three times for women with four to five and six and more parity respectively. On the other hand, high blood pressure, multiple pregnancies, smoking cigarette, and bearing a female child were negative predictors of normal birth weight. In other words, chances of low birth weight among women who reported smoking cigarette and those with high blood pressure were more than twice likely compared to women without the above conditions. Furthermore, the likelihood that women give birth to underweight babies was nearly double among women bearing female children or multiple pregnancies. Results of the logistic model are summarized in Table 3.
Discussion
This study used secondary data from the national Demographic and Health Survey 2017 to determine LBW prevalence and explore socioeconomic and demographic factors that predict LBW among Burundian women. LBW in Burundi was found to be close to other low- and middle-income countries namely Ethiopia and Iran. In Burundi, LBW is nearly 10% against 10% and 9.4% in Ethiopia [14] and Iran [15]; respectively. Conversely, LBW was found to be much higher in other countries such as India with one fifth of live births weighing less than 2,5 kilograms [16]. In our study, significant determinants of birth weights included wealth, parity, chronic health condition, pregnancy type (single versus multiple), woman’s age, and child’s sex. On the one hand, birth weight consistently increases with higher wealth quintiles, higher parity levels, and having diabetes. Compared to poorest women, birth weight increases of 50 grams for women belonging to poorer families. This increase doubles (100 grams) for women from middle class and again doubles for richest women who gave birth to babies weighing 200 grams more. Similarly, second and third order newborns weighed 220 grams more compared to first order babies. The increase in birth weight was consistent with higher birth orders and reached more than 300 grams for babies born to multiparous women from sixth pregnancy going forward. Diabetes was associated with an increase of more than 700 grams. On the other hand, multiple pregnancies, older age, and female babies were significant predictors of decreased birth weight. The most appealing evidence concerns multiple pregnancies which cause birth weight to decrease of about 1900 grams for triplet babies and about 920 grams for twin babies. Women older than 35 years gave birth to babies lower of 70 grams weigh and female newborns weighed 130 grams less compared to their male counterparts. Results from the linear model corroborate with those implemented using the logistic regression. Wealth index and higher parity determined the likelihood of giving normal weight babies while smoking, multiple pregnancies, child’s sex, and a woman’s chronic condition were significant predictors of the likelihood of LBW. Higher birth orders were associated with more than twice likelihood of bearing a normweight baby compared to first pregnancies.
In the same perspective, wealthier mothers and those highly educated were nearly two times more likely to give birth to normal weight babies. However, similar to the linear model results, twin pregnancies and female babies were nearly twice more likely to be underweight. Additionally, there was a double chance of giving birth to underweight babies among women who smoke cigarettes during the course of pregnancy were and those who had high blood pressure. Determinants of birth weight in Burundi corroborate with evidence from other settings. In Sri Lanka for instance, wealthier women and higher educated women were more likely to give birth to normal weight babies [17]. In this study, other significant determinants of birth weight were mother’s age at childbirth, newborn’s sex, and parity level. Contrary to the context of Burundi where antenatal care did not predict birth weight, Indian women who completed at least four recommended ANC visits were more likely to deliver normal weight babies [17]. Similar evidence has also been found in India [18]. Furthermore, similar to our findings, a wealth evidence has established the correlation between women with chronic health conditions such as diabetes with macrosomia [19, 20]. Multiple pregnancies were significant predictors of LBW in Burundi and in other similar settings. The example is the study by Taywade et. Al [21] in India where women bearing multiple pregnancies were 21 more likely to give birth to underweight babies [21]. Additionally, male sex was found to be a protective predictor of LBW in India and Ghana [18, 22]. Smoking was also a negative predictor as women who reported having smoked cigarette during pregnancy were at high risk of LBW in Ethiopia [23] and in India [21].
Conclusion
This study which used a nationally representative sample of Burundian women of reproductive age yielded evidence on LBW prevalence and factors affecting it. The prevalence of LBW was considerable when compared to many countries around the world (10%). Among important predictors affecting birth weight included a women’s age, wealth, education, parity, chronic health condition, smoking, pregnancy type (single versus multiple) and child’s sex. Markedly, LBW was highly associated with multiple pregnancies, female babies, the history of smoking over the course of the pregnancy, and high blood pressure. Despite considerable efforts put in place by the government to improve maternal and child health, LBW remains a public health concern. This study suggests the need for the implementation of targeted innovative interventions to tackle identified LBW risk factors among women of reproductive age. For instance, socio-economic interventions targeting poor household may help to improve economic status of women with an aim to reduce LBW prevalence among poorer women. Our study used secondary data analysis which has limit in establishing causal inference between predictors and the study outcome. This shortcoming could be addressed by cohort studies of pregnant women which have the possibility to unpack factors determining LBW with a much stronger evidence than cross-sectional surveys. Therefore, this study provides important evidence and a threshold for further research works in the field.
References
- Bernstein IM, Horbar JD, Badger GJ, Ohlsson A, Golan A, Network VO (2000) Morbidity and mortality among very-low-birth-weight neonates with intrauterine growth restriction. American journal of obstetrics and gynecology 182(1): 198-206.
- Mila H, Grellet A, Feugier A, Chastant Maillard S (2015) Differential impact of birth weight and early growth on neonatal mortality in puppies. Journal of animal science 93(9): 4436-442.
- Hack M, Breslau N, Weissman B, Aram D, Klein N, Borawski E (1991) Effect of very low birth weight and subnormal head size on cognitive abilities at school age. New England Journal of Medicine. 1991;325(4): 231-237.
- Hack M, Klein NK, Taylor HG (1995) Long-term developmental outcomes of low birth weight infants. The future of children 5(1):176-196.
- Organization WH (2019) UNICEF-WHO low birthweight estimates: levels and trends 2000-2015. World Health Organization.
- Christian P, Lee SE, Donahue Angel M, Adair LS, Arifeen SE, et al. (2013) Risk of childhood undernutrition related to small-for-gestational age and preterm birth in low-and middle-income countries. International journal of epidemiology 42(5):1340-1355.
- WHA65R6 (2012) Comprehensive implementation plan on maternal, infant and young child nutrition. Sixty-fifth World Health Assembly Geneva pp.21-26.
- Colglazier W (2015) Sustainable development agenda: 2030. Science 349(6252):1048-1050.
- Kamble V (2021) Health Returns to Birth Weight: Evidence from Developing Countries.
- Manyeh AK, Kukula V, Odonkor G, Ekey RA, Adjei A, et al. (2016) Socioeconomic and demographic determinants of birth weight in southern rural Ghana: evidence from Dodowa Health and Demographic Surveillance System. BMC Pregnancy and Childbirth 16(1):160.
- Mulu GB, Gebremichael B, Desta KW, Kebede MA, Aynalem YA, Getahun MB (2020) Determinants of low birth weight among newborns delivered in public hospitals in Addis Ababa, Ethiopia: Case-control study. Pediatric health, medicine and therapeutics 11:119-126.
- Mahumud RA, Sultana M, Sarker AR (2017) Distribution and determinants of low birth weight in developing countries. Journal of preventive medicine and public health 50(1): 18-28.
- Hughes MM, Black RE, Katz J (2017) 2500-g low birth weight cutoff: history and implications for future research and policy. Maternal and child health journal 21(2): 283-289.
- Gebregzabiherher Y, Haftu A, Weldemariam S, Gebrehiwet H (2017) The prevalence and risk factors for low birth weight among term newborns in Adwa General Hospital, Northern Ethiopia. Obstetrics and gynecology international pp.1-7.
- Momeni M, Danaei M, Kermani AJN, Bakhshandeh M, Foroodnia S, et al. (2017) Prevalence and risk factors of low birth weight in the Southeast of Iran. International journal of preventive medicine 8: pp.12.
- Bharati P, Pal M, Bandyopadhyay M, Bhakta A, Chakraborty S (2011) Prevalence and causes of low birth weight in India. Malaysian journal of nutrition 17(3): 301-313.
- de Mel S (2020) Determinants of Low Birth Weight in Sri Lanka. International Journal of Multidisciplinary Research and Publications 3(6): 80-87
- Kader M, Perera NKP (2014) Socio-economic and nutritional determinants of low birth weight in India. North American journal of medical sciences 6(7): 302-308.
- Ehrenberg HM, Mercer BM, Catalano PM (2004) The influence of obesity and diabetes on the prevalence of macrosomia. American journal of obstetrics and gynecology 191(3): 964-968.
- Kamana K, Shakya S, Zhang H (2015) Gestational diabetes mellitus and macrosomia: a literature review. Annals of Nutrition and Metabolism 66(Suppl. 2): 14-20.
- Taywade M, Pisudde P (2017) Study of sociodemographic determinants of low birth weight in Wardha district, India. Clinical Epidemiology and Global Health 5(1): 14-20.
- Agorinya IA, Kanmiki EW, Nonterah EA, Tediosi F, Akazili J, Welaga P, et al. (2018) Socio-demographic determinants of low birth weight: Evidence from the Kassena-Nankana districts of the Upper East Region of Ghana. PloS one 13(11):e0206207.
- Sema A, Tesfaye F, Belay Y, Amsalu B, Bekele D, Desalew A (2019) Associated Factors with Low Birth Weight in Dire Dawa City, Eastern Ethiopia: A Cross-Sectional Study. BioMed research international pp.1-8.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...