Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4722
Mini Review(ISSN: 2637-4722) 
Approach to Neurodegenerative Disease in Children: A Short Review Volume 1 - Issue 5
Shubhankar Mishra* and Ajit Prasad Mishra
- Department of Neurology, S C B Medical College, India
Received: July 13, 2018; Published: July 17, 2018
*Corresponding author: Shubhankar Mishra, Department of Neurology, S C B Medical College, India
DOI: 10.32474/PAPN.2018.01.000121
Abstract
Neurodegenerative disorders of childhood are complicated diseases with wide range of systematic involvement. These diseases often pose great challenge to clinicians in terms of diagnosis and management. The purpose of this article is to outline a systematic approach to a child presenting with suspected neurodevelopmental regression. Many inherited metabolic disorders present with neural regression. The clinical approach depends upon the age of presentation, site of involvement in brain. Sound clinical knowledge and better approach leads to early diagnosis, better management and above all genetic counselling. As the medical science is in the track of rapid progression several treatment modalities are in the pipeline for neurodegenerative syndromes, early diagnosis and referral to higher centres can bring a better future to the child.
Keywords: Neurodegenerative diseases; Hepatomegaly; White Matter; Grey Matter
Introduction
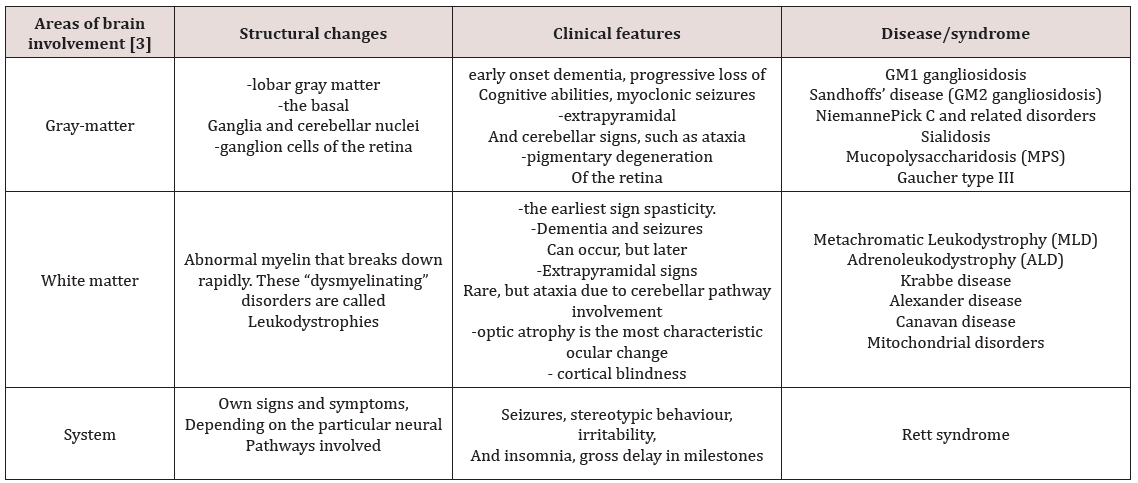
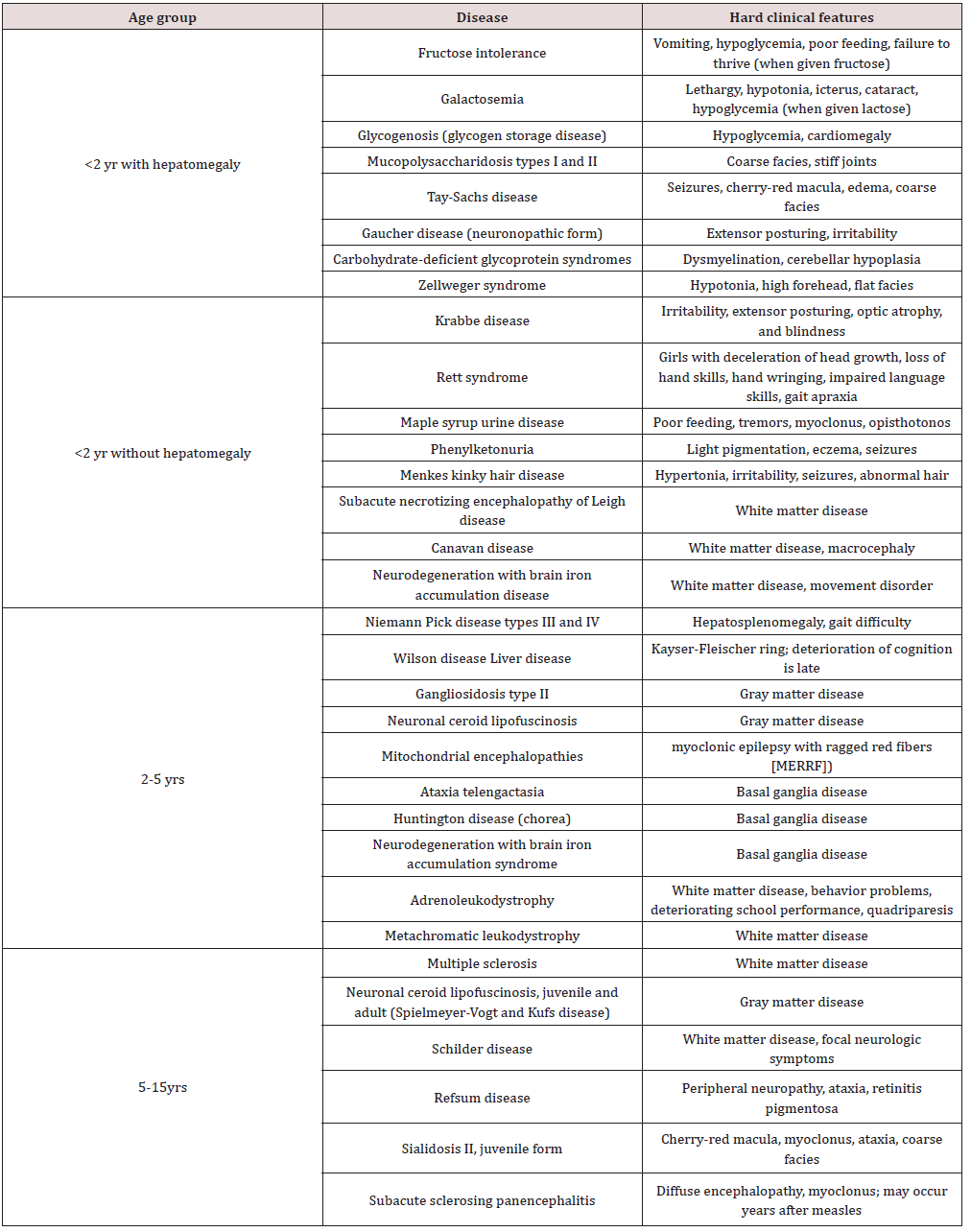
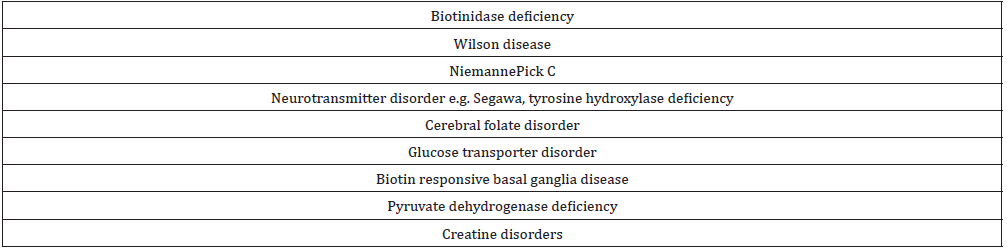
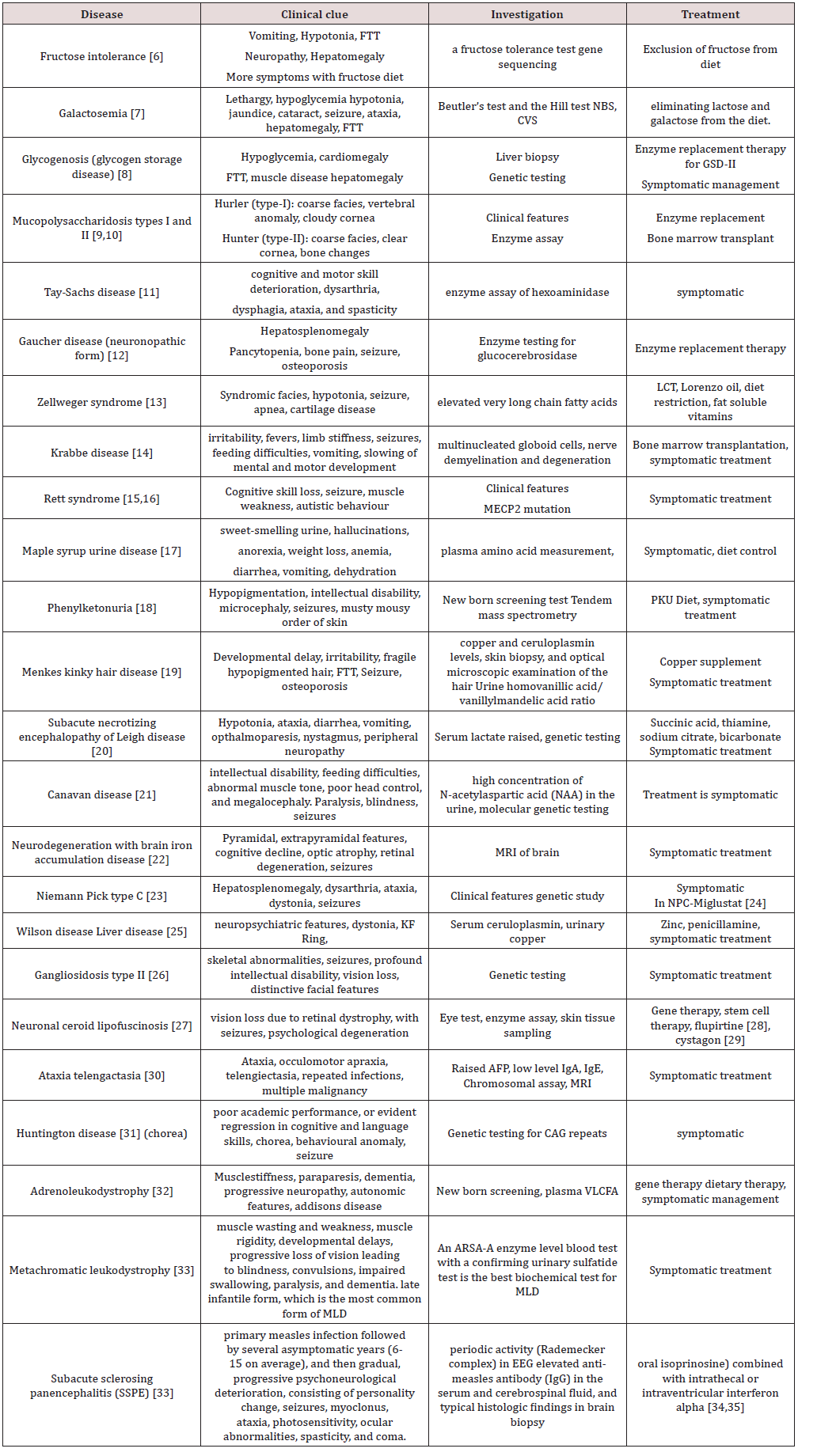
Neurodegenerative disorders of childhood include large, heterogeneous group of diseases that result from specific genetic and biochemical defects, chronic viral infections, and varied unknown causes. The hallmark of a neurodegenerative disease is regression and progressive deterioration of neurologic function with loss of speech, vision, hearing, or locomotion, often associated with seizures, feeding difficulties, and impairment of intellect [1]. The acquisition of new developmental milestones does not exclude the existence of a degenerative disorder. Most degenerative CNS disorders can be divided clinically into three groups: gray-matter diseases, white-matter diseases, and system diseases [1,2] (Tables 1-3).
Classification
Approach to Child with Marked Regression
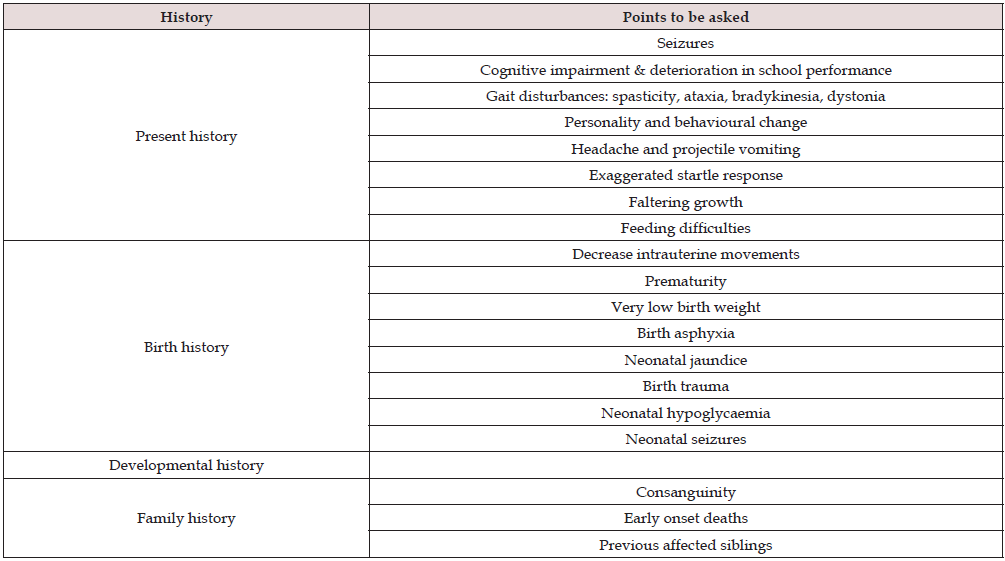
a) History: In a patient with developmental regression the history is very vital. Clues for diagnosis lie in the history. First step would be to ascertain the age of onset of regression and the acquisition of various milestones prior to that. Was the child completely normal before regression or was there a concern regarding development even prior to regression? Did the child attained milestones before losing it. Which milestones the child lost? In autism and other pervasive developmental disorders regression of language skills is noted first followed by loss of social skills (Tables 4 & 5).
References
- Johnston M (2016) Neurodegenerative disorders of childhood. In: Behrman RE, Kliegman RM, Jenson HB, (Eds.); Nelson textbook of pediatrics (20th edn.).
- Ellaway C, Christodoulou J (1987) Degenerative central nervous system (CNS) disease: In Workshop and Symposium. Percy 2: 82.
- Henry M Adam (2001) Degenerative Central Nervous System (CNS) Disease, Pediatrics in Review 22(5): 175-176
- Sreekantam S, Wassmer E (2013) An approach to developmental regression. Paediatrics and Child Health 23(6): 273-277.
- Pierre G (2013) Neurodegenerative disorders and metabolic disease. Archives of disease in childhood 98(8): 618-24.
- Maitre A, Maw A, Ramaswami U, Morley SL (2016) Relapsing Acute Axonal Neuropathy in Hereditary Fructose Intolerance. Pediatric neurology 64: 92-93.
- Goodin B (2006) An overview of expanded newborn screening for inborn errors of metabolism. Practical Gastroenterology 30(8): 34.
- Bembi B, Cerini E, Danesino C, Donati MA, Gasperini S, et al. (2008) Management and treatment of glycogenosis type II. Neurology 71(23- 2): S12-S36.
- Wraith JE, Scarpa M, Beck M, Bodamer OA, De Meirleir L, et al. (2008) Mucopolysaccharidosis type II (Hunter syndrome): A clinical review and recommendations for treatment in the era of enzyme replacement therapy. European journal of paediatrics 167(3): 267-277.
- Vellodi A, Young EP, Cooper A, Wraith JE, Winchester B, et al. (1997) Bone marrow transplantation for mucopolysaccharidosis type I: Experience of two British centres. Archives of disease in childhood 76(2): 92-99.
- Desnick RJ, Kaback MM (2001) Tay-Sachs disease. Academic Press, USA.
- Weinreb NJ, Charrow J, Andersson HC, Kaplan P, Kolodny EH, et al. (2002) Effectiveness of enzyme replacement therapy in 1028 patients with type 1 Gaucher disease after 2 to 5 years of treatment: a report from the Gaucher Registry. The American journal of medicine 113(2):112-119.
- Brown FR, McAdams AJ, Cummins JW, Konkol R, Singh I, et al. (1982) Cerebro-hepato-renal (Zellweger) syndrome and neonatal adrenoleukodystrophy: Similarities in phenotype and accumulation of very long chain fatty acids. The Johns Hopkins medical journal 151(6): 344-351.
- Suzuki K, Suzuki Y (1970) Globoid cell leucodystrophy (Krabbe’s disease): Deficiency of galactocerebroside β-galactosidase. Proceedings of the National Academy of Sciences 66(2): 302-309.
- Hagberg B, Goutières F, Hanefeld F, Rett A, Wilson J (1985) Rett syndrome: criteria for inclusion and exclusion. Brain and Development 7(3): 372-373.
- Amir RE, Van den Veyver IB, Wan M, Tran CQ, Francke U, et al. (1999) et.al Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2. Nature genetics 23(2): 185
- Strauss KA, Puffenberger EG, Morton DH (2006) Maple syrup urine disease.
- Blau N, van Spronsen FJ, Levy HL (2010) Phenylketonuria. The Lancet 376(9750): 1417-1427.
- Kaler SG, Holmes CS, Goldstein DS, Tang J, Godwin SC (2008) Neonatal diagnosis and treatment of Menkes disease. New England Journal of Medicine 358(6): 605-614.
- Pincus JH (1972) Subacute necrotizing encephalomyelopathy (Leigh’s disease): A consideration of clinical features and etiology. Developmental Medicine & Child Neurology 14(1): 87-101.
- Kumar S, Mattan NS, de Vellis J (2006) Canavan disease: A white matter disorder. Developmental Disabilities Research Reviews 12(2): 157-165.
- Gregory A, Hayflick SJ (2005) Neurodegeneration with brain iron accumulation. Folia Neuropathologica 43(4): 286-296.
- Sévin M, Lesca G, Baumann N, Millat G, Lyon-Caen O, et al. (2006) The adult form of Niemann-Pick disease type C. Brain130(1): 120-133.
- Patterson MC, Vecchio D, Prady H, Abel L, Wraith JE (2007) Miglustat for treatment of Niemann-Pick C disease: a randomised controlled study. The Lancet Neurology 6(9): 765-772.
- Brewer GJ, Yuzbasiyan-Gurkan V (1992) Wilson disease. Medicine 71(3): 139-164.
- Patel V, Goebel HH, Watanabe I, Zeman W (1974) Studies on G M1- gangliosidosis, type II. Acta neuropathologica 30(2): 155-173.
- Jalanko A, Braulke T (2009) Neuronal ceroid lipofuscinoses. Biochimica et Biophysica Acta (BBA)-Molecular Cell Research 1793(4): 697-709.
- Dhar S, Bitting RL, Rylova SN (2002) Flupirtine blocks apoptosis in batten patient lymphoblasts and in human postmitotic CLN3- and CLN2- deficient neurons. Annals of Neurology 51(4): 448-466.
- Levin SW, Baker EH, Zein WM, Zhang Z, Quezado ZM, et al. (2014) Oral cysteamine bitartrate and N-acetylcysteine for patients with infantile neuronal ceroid lipofuscinosis: A pilot study. The Lancet Neurology 13(8): 777-787.
- Lavin MF (2008) Ataxia-telangiectasia: From a rare disorder to a paradigm for cell signalling and cancer. Nature reviews Molecular cell biology 9(10): 759.
- Letort D, Gonzalez-Alegre P (2013) Huntington’s disease in children. In Handbook of clinical neurology 113: 1913-1917.
- Schaumburg HH, Powers JM, Raine CS, Suzuki K, Richardson EP (1975) Adrenoleukodystrophy: A clinical and pathological study of 17 cases. Archives of Neurology 32(9): 577-591.
- Gieselmann V, Krägeloh-Mann I (2010) Metachromatic leukodystrophy: An update. Neuropediatrics 41(01): 1-6.
- Nihei K (1997) Subacute sclerosing panencephalitis (SSPE): Nihon rinsho. Japanese journal of clinical medicine 55(4): 908-915.
- Yalaz K, Anlar B, Oktem F, Aysun S, Ustacelebi S, et al. (1992) Intraventricular interferon and oral inosiplex in the treatment of subacute sclerosing panencephalitis. Neurology 42(3): 488-491.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...