Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4722
Review Article(ISSN: 2637-4722) 
Improvement of body composition in 8- to 11-year-old male school children: Effects of a 6-months lifestyle intervention Volume 3 - Issue 4
Julia Matjazic1, Paula Moliterno2 and Kurt Widhalm1*
- 1Austrian Academic Institute for Clinical Nutrition and Medical University of Vienna
- 2Austrian Academic Institute for Clinical Nutrition and Escuela de Nutricion, Universidad de la Republica, Uruguay
Received: March 04, 2022 Published: March 16, 2022
Corresponding author: Kurt Widhalm, Head of Austrian Academic Institute for Clinical Nutrition and Medical University of Vienna, Austria
DOI: 10.32474/PAPN.2022.03.000166
Abstract
Background: Gastroenteritis, caused by either bacteria, virus, or parasites, is a gastrointestinal inflammatory illness known by many. Lactoferrin (Lf), a protein primary found in human milk, is released from activated polymorphonuclear leucocytes during an inflammatory response. As such, Lf could be suggested as an indicator for the degree of inflammation in gastroenteritis.
Objective: We aimed to investigate the degree of inflammation by the level of fecal Lf compared to the culture of well-known bacterial enteric pathogens in toddlers and adults, and in toddlers to examine if the intake of breast milk was associated with higher levels of fecal Lf when compared to non-breastfed toddlers.
Methods: Levels of fecal Lf and fecal bacterial culture were analyzed in 512 consecutive fecal samples from patients with diarrhea where physicians found sampling indicated. Further, to assess the number of toddlers who had breast milk, the medical records were obtained from the National Diagnostic Register.
Results: 477 out of 512 patients (93%) with gastrointestinal symptoms had positive fecal cultures with the most common bacteria being Clostridum difficile 263 (51%). In patients between 3 and 94 years of age, all Shigella sonnii and shiga-toxin producing Escherichia coli indicated severe inflammation with fecal Lf levels >10,000 pg/ml, although only Shigella was significant when compared with normal young adults with fecal Lf levels < 100 pg/ml and without gastrointestinal symptoms (controls) (p = 0.0002). All other bacteria-positive feces cultures were associated to increased levels of fecal Lf > 1,000 pg/ml when compared with controls (p < .05). In patients between 3 weeks and less than 3 years of age, all pathogenic bacteria cultured, apart from Salmonella enteritidis and Clostridium perfringens (enterotoxin positive), were significantly associated with fecal Lf levels > 1,000 pg/ml when compared with controls (p <.05). The severity of gastrointestinal symptoms and levels of fecal Lf were not significantly associated (p-value 1.0). Breast-milk (partially and fully) vs formula-milk and fecal Lf levels in toddlers < 6 months of age revealed no significant differences (p = 0.29) Conclusion: High levels of fecal Lf were associated with positive cultures of feces, and the more aggressive the bacteria cultured was, the higher level of fecal Lf was observed, when compared with normal levels of Lf in young healthy men and women without gastrointestinal symptoms. In an unmatched association-analysis, no significant differences between breast milk and formula milk concerning fecal Lf levels were observed in our study.
Keywords: Lactoferrin; Bacterial Enteric Pathogens; Gastroenteritis; Necrotizing Enterocolitis; Diarrhea
Introduction
The global prevalence of people with overweight and obesity increased dramatically in adults and children between 1980 and 2013 [1]. Abarca-Gómez et al. showed an increase in worldwide prevalence of overweight and obesity among children between 1975 and 2016. Among girls, the proportion of obese people rose from 0.7 % to 5.6 % and among boys from 0.9 % to 7.8 % [2]. In Austria, 30% of the boys and 22% of the girls between 6 and 9 years old are overweight and/or obese [3]. Childhood obesity, as excessive fat accumulation can lead to short- and longterm physical, social, or emotional health problems. Overweight or obese children are much more likely to suffer from asthma, diabetes, high blood pressure, skeletal disorders, mental health problems, and other illnesses in adulthood [4]. Excessive weight gain during childhood is a complex phenomenon in which multiple risk factors are involved, including the combination of genetics, behavior, and inadequate environment that leads to overweight and obesity [5]. The two main factors that possibly contribute to gain weight are the increased consumption of energy-rich foods that have a high fat and sugar content and decreased physical activity [6]. Therefore, approaches aiming at increasing physical activity and healthy eating have been identified as efficient means to prevent excessive weight gain during childhood [7], particulary evidence supports the effectiveness of school-based interventions [8]. Besides physical inactivity and unhealthy diet two main determinants, other risk factors such as weight at birth, parents’ nutritional status, social factors, and timing of maturation play also a major role [9]. The simplest way to measure overweight and obesity is through the body mass index (weight in kilograms [kg] divided by squared height [m] - BMI). Although this anthropometric method can be used to assess body fat in children [10], it does not necessarily identify distribution of fat. Moreover, body fat in the pediatric population varies between sex, race and maduration stage [11,12], and the location of adipose deposits implies different risk of health complications. Thus, assessment of body composition through bioelectrical impedance analysis is also used.
The WHO recommends as strategies to battling overweight and obesity the promotion of increased consumption of fruits, vegetables, whole grain products, pulses, and nuts, limiting intake of energy-dense nutrient-poor foods, as well as regular physical activity and adequate sleep [6]. Thus, schoolsare ideal settings to promote healthy lifestyle behaviors [8]. The EDDY study is an evaluated prevention project carried out at a Viennese elementary school for several years aiming to prevent childhood obesity and progressive excessive weight gain through nutrition and physical activity lifestyle intervention. Previous results from the EDDY project have shown an overall trend for a less increase in body fat and a reduced consumption of sweets after the intervention [13,14]. Although important sex differences regarding body composition and food intake choices usually are not evident until after the onset of puberty, it has been reported through a longitudinal analysis a more accentuated increase in fat mass percentage in boys aged 6-11 years old when compared to girls [15]. Moreover, the first Atlas of Childhood Obesity [16], recently reported that in Austria, the prevalence of obesity in boys almost doubled the prevalence in girls when comparing within age group. Sugary beverages are associated with overweight, because the sugar in drinks does not lead to a feeling of satiety. Hence there is no reduction in food intake, leading to a higher weight gain [17-19]. The aim of this study was to assess changes in body fat, BMI and consumption of sugary drinks and sweets of a sample of 69, 8 – 11 years old Viennese male pupils after a 6-month intervention with nutritional training and physicial activity program.
Subjects and Methods
The EDDY prevention project was developed to avoid childhood obesity by nutrition training and physical activity. The intervention took place at a Viennese elementary school (Haebergasse) in the school year 2018/2019. The intervention phase lasted half a school year (January 2019 – June 2019). Overall, a total of 146 pupils aged 8-11 years participated in the study. The kids were devided into an intervention group (3rd grade) and a control group (4th grade). Only male participants (n = 69) were considered for the statistical analysis. A total of n = 36 boys were assigned to the intervention group and n = 33 pupils were assigned to the control group.
Inclusion and exclusion criteria
All male students between the ages of 8 and 11, in the 3rd and 4th grade of the Haebergasse elementary school in the school year (2018/2019), were included. In addition, a declaration of consent from the participant and his or her legal guardian had to be available for participation. All the data from the students who took part in both tests (t0 = December 2018 and t1 = June 2019) were used. Students who joined during the school year were not included. The intervention group received, as part of school lessons, nutrition lessons once a week (50 minutes) and two physicial activity units a week (each 50 minutes). The practical and interactive nutrition lessons were organized and conducted by trained members of the EDDY team. The objective of the nutrition lessons was to teach the students the basics of a balanced and healthy diet and the sensible use of food. Therefore, different foods and food components were studied. Physicial activity lessons were organized and held by sports students from the University of Vienna. The primary goal was to improve endurance performance through various exercises and to build up physicial strength in students. The intent of the multidisciplinary intervention was to take preventive measures to counteract the further spread of obesity and prevent possible secondary diseases.
The children were tested twice as part of the study. Once, before the start of the intervention (t0 = December 2018) and 6 months later after the intervention phase (t1 = June 2019). The students of the control group did not receive any intervention and were not involved in the intervention process. During testing points, anthropometric and body composition data from all children (control an intervention group) were obtained by trained technicians. Body height, weight and body fat percentage were measured, and BMI calculated. The height of the subjects was measured using a stadiometer (SECA, Germany), with the kid standing without shoes. Body weight and body fat percentages were determined by bioelectric impedance analysis using a multi frequency segmental body composition analyser (TANITA MC 780 MA). Information such as age, sex and height were entered by the investigator and once body weight was assessed by the scale, a full segmental analysis was performed in less than 20 seconds. Total fat, total fat-free mass, water and visceral adiposity index was reported. In the control group, along with the anthropometric and body composition data, nutritional behaviour and habits and physical performance were additionally assessed. Frequency of sugary drinks (such as Soda, Coke, Lemonade, Iced Tea etc.) and sweets consumption (such as gummy sweets, chocolate etc.) was assessed through a questionnaire [20]. A positive ethical approval for the EDDY-Study was obtained from the Ethical Committee of the Sigmund Freud University, Vienna (PAFGRW9O@EFQV885378). Written informed consent was obtained from each child and one of their legal guardians prior to participation in the study. The programs IBM SPSS Statistics 26 was used for statistical analysis of the data. Changes in body fat and BMI were measured using a t-test. Statistical tests were two-sided. P values smaller than 0.05 were considered statistically significant.
Results
Overall changes in outcomes variables after 6-month intervention
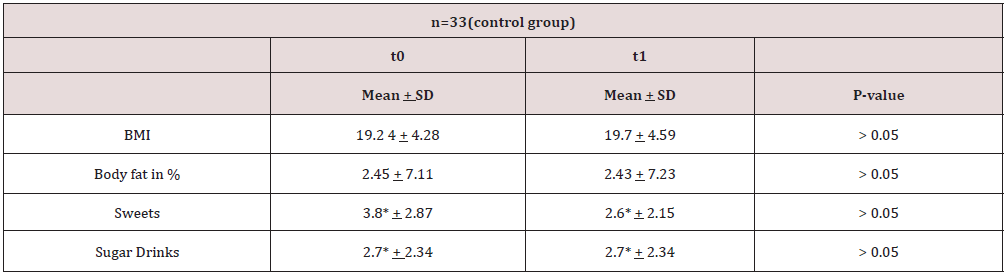
Changes in BMI, body fat in percentage, sweets and sugary drinks among the control and intervention group are summarized in Tables 1 & 2.
* = frequency of weekly intake.
Table 2: changes in BMI, body fat in %, sweets, and sugary drinks in the intervention group at t0 and t1.
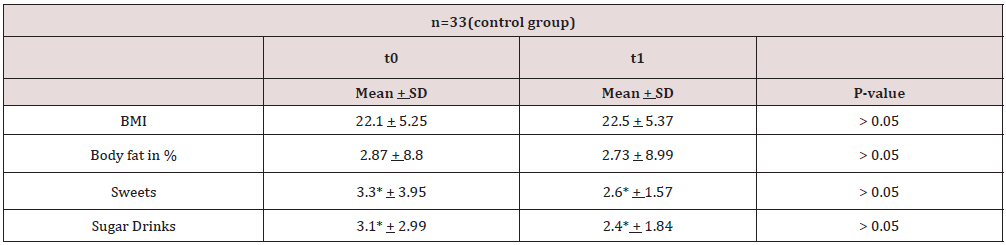
* = frequency of weekly intake.
BMI and bodyfat
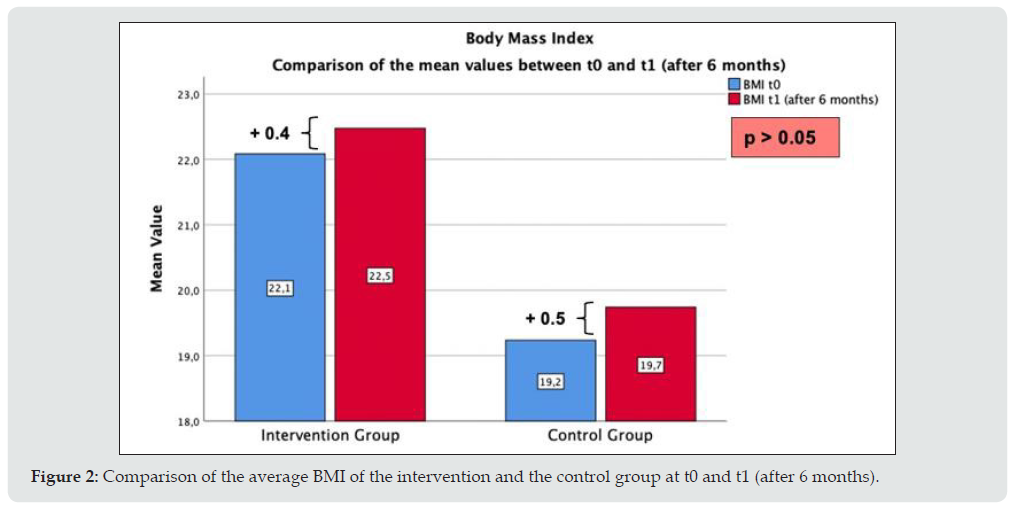
At baseline, the intervention group (n = 36) showed a mean value of 28.7 ± 8.8 % body fat. At the time of the first data collection, the control group showed a mean value of 24,5 ± 7,1 % body fat. In the follow-up measurement after a 6-month period, a significant difference between the intervention and control group could be identified (p < 0,05). The following bar diagram (Figure 1) shows that the mean body fat percentage in both groups (n = 69) decreased between t0 and t1 (after 6 months). However, the reduction in percentage of body fat in the intervention group (n = 36) was significantly higher (p < 0,05) than in the control group (n = 33). The average body fat percentage in the intervention group decreased from 28.74 % to 27.34 %. The body fat percentage in the control group was on average 24.5 % at time t0 and 24.27 % at time t1. Regarding BMI, no significant change could be identified. The following bar diagram (Figure 2) shows the change in the average BMI in both groups (n = 69) between t0 and t1 (after 6 months). A slight increase in BMI was observed both in the intervention and control group. The average BMI in the intervention group (n = 36) rose from 22.1 to 22.5 kg/m2. The BMI in the control group (n = 33) averaged 19.2 kg/m2 at time t0 and 19.7 kg/m2 at time t1.
Figure 1: Comparison of the average body fat percentage of the intervention and the control group at t0 and t1 (after 6 months).

Figure 2: Comparison of the average BMI of the intervention and the control group at t0 and t1 (after 6 months).
Sugary drinks and sweets consumption
Figure 3 shows that the mean consumption of sweets per week in both the intervention group and the control group decreased over a period of 6 months (p > 0.05). At the start of the study, participants in the intervention (n = 36) ate in an average frequency of 3.3 times a week, while six months later, it was 2.6 times a week. In the control group (n = 33), the average consumption of sweets was 3.8 times per week at the beginning of the intervention and 2.6 times per week after 6 months. Overall, the consumption of sugary drinks fell in the intervention and the control group (p > 0.05). Figure 4 shows that the reduction in the mean intake after 6 months is more significant than the one of the control groups. While at the beginning of the study, the children in the intervention group (n = 36) consumed sugary drinks 3.1 times a week, 6 months later, it was only 2.4 times a week. The consumption in the control group (n = 33) remained almost constant on average. At the start of the study as well as 6 months later, the mean consumption of sugary drinks was 2.7 times a week.
Figure 3: Comparison of the average consumption of sweets of the intervention and the control group at t0 and t1 (after 6 months).
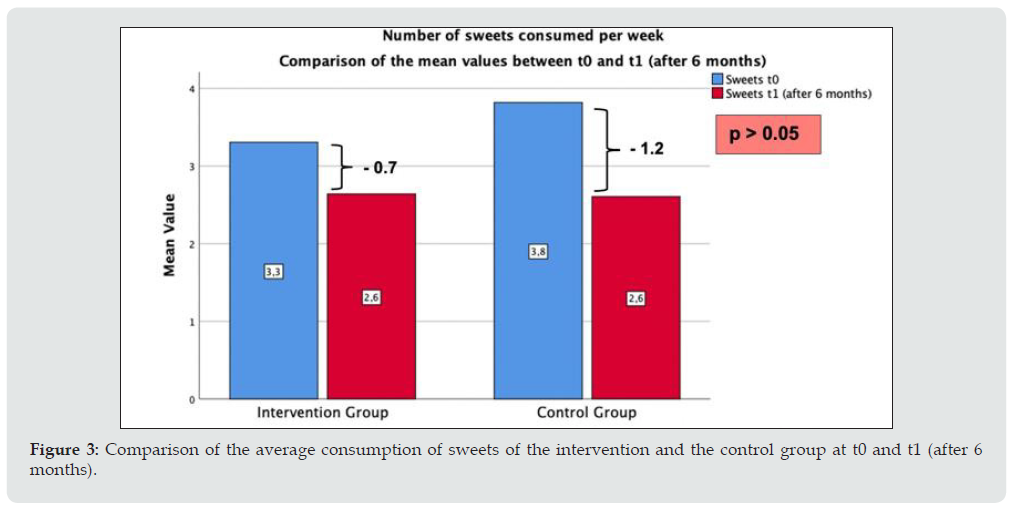
Figure 4: Comparison of the average consumption of sugary drinks of the intervention and the control group at t0 and t1 (after 6 months).

Discussion
The goal of the study was to increase physical activity and promote a healthy diet by nutrition lessons and physical education in school children. Furthermore, the intention was to prevent the occurrence of obesity and diseases associated with obesity. The study results show that the body fat percentage in both groups decreased on average. These results show a significant difference between the two groups and indicate that the intervention had a positive effect on body fat. At baseline, the control group subjects had a lower body fat percentage than those assigned to the intervention group. Third-grade students are approximately one year younger than fourth-grade students; this could explain the lower body fat percentage at the first data collection. It can be noted that the pupils who participated at baseline as well as 6 months later are classified in the upper range of the percentiles named overfat and obese according to Mc Carthy et al. Normal body fat percentage is ranked between the 2nd and 85th percentile. That means the normal body fat percentage of a 10- year-old boy is between 12.8 % and 22.8 % [16]. The results of those study participants who already had a body fat percentage above the 98th percentile according to Mc Carthy et al. (4 of 36 participants in the intervention group) at the start of the study (t0) also revealed a remarkably increased body fat percentage after 6 months of intervention [21]. It is possible that children with such a high percentage of body fat cannot benefit from the prevention project; for this group, probably a special program should be implemented, that is specifically tailored to children with a body fat percentage above the 98th percentile.
At baseline, 28 out of 69 school children were overweight or obese according to BMI-Percentiles by Kromeyer-Hauschild et al. [22]. This means the weight of 41 % of the male study participants was significantly above normal weight at the beginning of the project. One of the reasons for the high prevalence of overweight and obesity could be the high number of children with a migration background. The percentage of children with migration background wasdetermined by using questionnaires. Two trials in Germany showed that the prevalence of overweight and obesity in children with a migration background is higher than in children with German roots. It is suggested that the higher prevalence of overweight and obesity among immigrant children is related to socio-economic status [23,24]. Segna et al. also examined the prevalence of extreme obesity in relation to the children’s mother tongue in a Viennese sample of almost 25.000 children and adolescents. It could have been shown that non-German-nativespeaking participants have a higher prevalence of overweigth or obesity, which may be an indicator for migration background [25]. Nutritional behaviour was also examined as part of the study. This was assessed by the number of sweets and sugary drinks consumed per week, which the participants reported using a questionnaire. The results show that the average consumption of both – sweets and sugary drinks – in the intervention group was reduced over the 6-month period. In the control group, the mean value of the intake of sweets and sugary drinks also decreased throughout the study. However, compared with the control group, the reduction of the intake was higher in the intervention group. It is conceivable that the children in the intervention group will talk to their siblings or friends in the control group about it outside of school and that this will also lead to a reduction in consumption of sweets within the control group. The EDDY study has several strengths and weaknesses. The main limitation of the study is its small number of participants. The study population consists of Viennese pupils and the data may not be representative for the Austrian population in total. Strengths of the EDDY project is the large variety in BMI and body fat among the study population as well as the evaluation of the effect of the intervention on body composition using BIA. Furthermore direct measurements were be carried out by trained staff.
Conclusion
The results of the prevention study inidicate that a combined intervention (nutrition education and physical activity) has a positive effect on body composition. There was a significant difference between intervention- and control group in regards to bodyfat. Whereas the bodyfat percentage in the intervention grouwas reduced by -1.4 %, bodyfat percentage in the control group was only reduced by 0.23 % (p < 0.05). An effect on the BMI could not be shown. However, other studies with a combination of nutritional training and physical activity show that the BMI can be reduced with a multidisciplinary intervention [26,27]. It would be important for future prevention programs to involve parents and school doctors more fully in the project. One possibility would be to inform the legal guardians regularly through a newsletter, containing healthy recipes and/or useful leisure time tips. In this way, one could try to positively influence the children’s lifestyle outside of school and encourage them to eat predominantly healthy and encourage more physical activity. As pupils are examined by their school doctors on a regular basis, they could play a key role regarding to obesity prevention. Due to their medical knowledge, school doctors are able to detect overweight very soon and take the first preventive steps. Additionally, it would be important that nutrition lessons become part of regular school lessons. In this way, it would be possible to teach children what a healthy diet should contain and why it is so essential for human health and physical wellbeing. Apart from the above, it would be equally important to arrange unlimited access to drinking water in schools, whereas there should be a ban implemented for the sale of sugar contained beverages. Overall, the results show that an improvement in healthy nutritional behaviour and a reduction of body fat through combined nutritional and exercise training within a school-based prevention program is possible. It can, therefore, improve both the health behaviour and the health status of the subjects. The present study undoubtedly contributes to the WHO recommendations to reduce the pandemic spread of overweight and obesity in our children. Further investigation on the subject is recommended, whereby more intensive involvement of the family environment and special care for obese children would be desirable.
References
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C (2014) Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384(9945): 766-781.
- Abarca Gómez L, Abdeen ZA, Hamid ZA, Abu Rmeileh NM, Acosta Cazares B, Acuin C (2017) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. The Lancet 390(10113): 2627-2642.
- (2018) Childhood Obesity Surveillance Initiative (COSI) Factsheet. Highlights 2015-17 (2018).
- Fang X, Zuo J, Zhou J, Cai J, Chen C (2019) Childhood obesity leads to adult type 2 diabetes and coronary artery diseases: A 2-sample mendelian randomization study. Medicine (Baltimore) 98(32): e16825.
- Kohat, Robbins J, Panganiban J. Update on Childhood/Adolescent Obesity and Its Sequela. Current Opinion in Pediatrics 31(5): 645-653.
- World Health Organization (2004) Global Strategy on Diet, Physical Activity and Health - 2004
- Fornari E, Brusati M, Maffeis C (2021) Nutritional Strategies for Childhood Obesity Prevention. Life (Basel) 11(6): 532.
- Wang Y, Cai L, Wu Y, Wilson RF, Weston C (2015) What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes Rev 16(7): 547-565.
- Parsons TJ, Power C, Logan S, Summerbell CD (1999) Childhood predictors of adult obesity: a systematic review. Int J Obes Relat Metab Disord 23 Suppl 8: S1-107.
- Alves Junior CA, Mocellin MC, Gonçalves ECA, Silva DA, Trindade EB (2017) Anthropometric Indicators as Body Fat Discriminators in Children and Adolescents: A Systematic Review and Meta-Analysis. Adv Nutr 8(5): 718-727.
- Daniels SR, Khoury PR, Morrison JA (1997) The utility of body mass index as a measure of body fatness in children and adolescents: differences by race and gender. Pediatrics 99(6): 804-807.
- Kyle UG, Earthman CP, Pichard C, Coss Bu JA (2015) Body composition during growth in children:limitations and perspectives of bioelectrical impedance analysis. Eur J Clin Nutr 69(12): 1298-1305.
- Pöppelmeyer C, Helk O, Mehany S, Hauer R, Pachinger O (2016) Die Wiener Preventionsstudie EDDY - Erste Ergebnisse. Pediatrician Pedolog Austria 51(3): 104-108.
- Widhalm K, Helk O, Pachinger O (2018) The Viennese EDDY Study as a Role Model for Obesity:Prevention by Means of Nutritional and Lifestyle Interventions. Obesity Facts 3(11): 247-256.
- Santos LP, Santos IS, Matijasevich A (2019) Changes in overall and regional body fatness from childhood to early adolescence. Sci Rep 9(1): 1888.
- Lobstein T, Brinsden H (2019) Atlas of childhood obesity. World Obesity Federation.
- De Ruyter JC, Olthof MR, Seidell JC, Katan MB (2012) A trial of sugar-free or sugar-sweetened beverages and body weight in children. The New England journal of medicine 367(15): 1397-1406.
- Luger M, Lafontan M, Bes Rastrollo M, Winzer E, Yumuk V (2017) Sugar-Sweetened Beverages and Weight Gain in Children and Adults: A Systematic Review from 2013 to 2015 and a Comparison with Previous Studies. Obesity facts 10(6): 674-693.
- Keller A, Bucher Della Torre S (2015) Sugar-Sweetened Beverages and Obesity among Children and Adolescents: A Review of Systematic Literature Reviews. Childhood obesity (Print) 11(4): 338-346.
- Truthmann J, Mensink GB, Richter A (2011) Relative validation of the KiGGS Food Frequency Questionnaire among adolescents in Germany. Nutrition Journal 10(1): 133.
- McCarthy HD, Cole TJ, Fry T, Jebb SA, Prentice AM (2006) Body fat reference curves for children. Int J Obes (Lond) 30(4): 598-602.
- Kromeyer Hauschild K, Wabitsch M, Kunze D, Geller F, Geiß HC, Hesse V (2001) Permanent Firden Body-mass-Index for Dies Kindes- and Jugendalter with Hiranziehung versions of deutscher Stichproben. Monatsschr Kinderheilkd 149(8): 807-18.
- Zhou Y, von Lengerke T, Walter U, Dreier M (2018) Migration background and childhood overweight in the Hannover Region in 2010-2014: a population-based secondary data analysis of school entry examinations. Eur J Pediatr 177(5): 753-763.
- Will B, Zeeb H, Baune BT (2005) Overweight and obesity at school entry among migrant and German children: a cross-sectional study. BMC Public Health 5: p.45.
- Segna D, Widhalm H, Pandey MP, Zehetmayer S, Dietrich S (2012) Impact of mother tongue and gender on overweight, obesity and extreme obesity in 24,989 Viennese children/adolescents (2-16 years). Wien Klin Wochenschr 124(21-22): 782-788.
- Schaefer A, Winkel K, Finne E, Kolip P, Reinehr T (2011) An effective lifestyle intervention in overweight children: one-year follow-up after the randomized controlled trial on Obeldicks light. Clin Nutr 30(5): 629-633.
- Nemet D, Barkan S, Epstein Y, Friedland O, Kowen G (2005) Short- and long-term beneficial effects of a combined dietary-behavioral-physical activity intervention for the treatment of childhood obesity. Pediatrics 115(4): e443-449.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...