Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4722
Research Article(ISSN: 2637-4722) 
Continuous Remote Monitoring of Newborn Babies Using I vital Monitoring System is Better Than Intermittent Monitoring – A Pilot Study Volume 3 - Issue 5
Santosh Kumar Kamalakannan1*, J Kumutha2 and Prithiviraj Manohran3
- 1Associate professor, Department of Neonatology, Saveetha medical college and hospital, India
- 2Professor in Neonatology, Department of Neonatology, Saveetha medical college and hospital, India
- 3Marketing manager, HELYXON private limited, India
Received: November 11, 2022 Published: November 23, 2022
Corresponding author: Santosh Kumar Kamalakannan, Associate professor in Neonatology, Department of Neonatology, Saveetha medical college and hospital, Thandalam, Chennai, India
DOI: 10.32474/PAPN.2022.03.000172
Abstract
Introduction
Monitoring of vital parameters in a sick neonate is an important aspect in their management. Monitoring of vital parameters helps in early identification and early intervention which would result in better neonatal outcomes with respect to mortality and morbidity. Traditionally monitoring is done by Staff nurses intermittently. The concept of enabling the parents to monitor the vital parameters of there is a new concept. The digitalization of information has the advantage of reducing documentation error. One such monitoring system is the iVital system of monitoring which aims at continuously monitoring the vital parameters namely saturation, heart rate and temperature of the neonate which needs to be validated before it can be used as a routine for neonatal monitoring.
Materials and Methods
a) Study Design: Pilot study (observational study).
b) Study Population: Neonates delivering at Saveetha medical college and hospital, Thandalam.
c) Study Period: Dec 2017 to August 2018.
d) Sample Size: Convenient sample size.
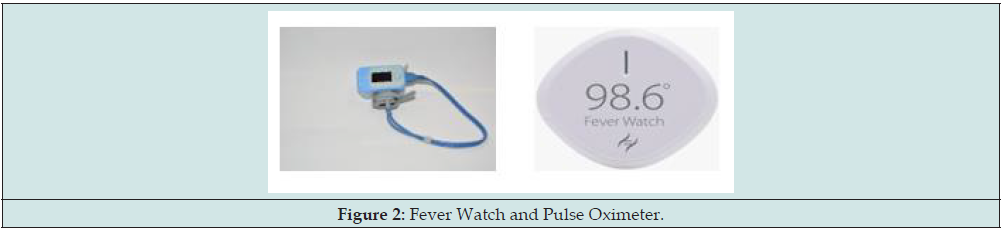
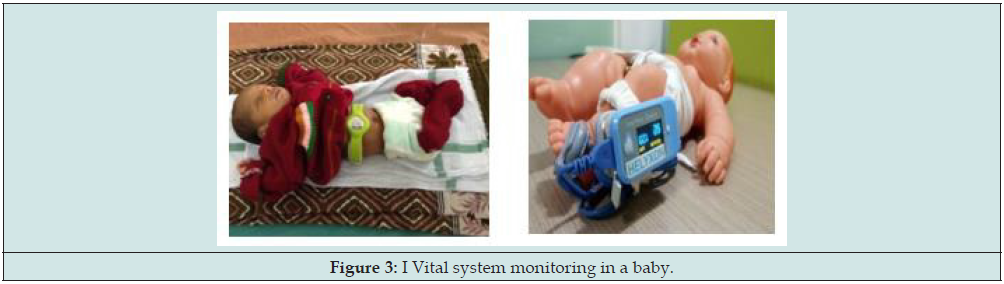
The I Vital system consists of recording the heart rate and saturation by using Pulse-Oximeter connected to the to the left lower limb or the right lower limb (in case of an IV cannula in the left lower limb) to record the post ductal saturation and heart rate. The temperature is recorded simultaneously using a Fever Watch instrument which was attached to the right upper quadrant of the abdomen using the Fever Watch Band. The neonates were classified into two groups namely Term Babies and Preterm Babies and were monitored for 24 to 48 hours using the I Vital system. The end points of the study were detection of any derangements in the vital parameters which were not due to probe displacement and represented true illness in the neonate.
Results: Babies were monitored using the I Vital system for a period of 2188 hours (91 babies were monitored for a period of 24 hours and one bay was monitored for 4 hours). The total number of events recorded were 1,31,100. Preterm babies included in the study were monitored for 618 hours resulting in recording of 37,080 events and term babies included were studied for 1570 hours resulting in recording of 94,020 events .The I Vital system had a sensitivity of 95.1%,Specificity of 99.9%,with the Positive Predictive value of 42.34% and Negative Predictive value of 100%.When temperature alone was studied Sensitivity was 100.0%,Specificity was 100.0%,Positive predictive value was 88.2% and Negative predictive value was 100%,similarly when saturation alone was studied Sensitivity was 100.0%,Specificity was 99.95%, with the Positive predictive value of31.91% : 95% CI (23.36 – 41.89)and Negative predictive value of100%.While the Sensitivity was 85%, Specificity was 99.9%, Positive predictive value was 54.84%and Negative predictive value was 100% when heart rate was studied alone.
Conclusion: I Vital system is effective in early identification of sickness when compared to routine monitoring with an overall sensitivity of 95 % and specificity of 99.9%.
Keywords: Neonate; I Vital system; continuous monitoring; heart rate; saturation; temperature
Introduction
All sick and at-risk babies need monitoring of the vital parameters. Neonates need to be monitored during the NICU stay and when interventions are performed. Monitoring of vital signs is usually done using equipment like multipara monitor with ability to continuously measure multiple parameters and raise alarm when abnormal measurement is sensed. Continuous monitoring of vital signs is a useful tool to detect clinical deterioration in an earlier stage of derangement and allows the clinicians to take corrective steps at right time. The subtle changes in vital signs often are present 8 to 24 hours ahead of a life-threatening event such as Cardio / Respiratory failure [1-3]. However, once the babies recover from initial sickness, they are moved to stepdown nursery, where usually the nurses monitor the babies intermittently. Though these babies are shifted to step down nursery they are at a risk of clinical worsening and may need continuous monitoring for extended period until discharge. Continuous monitoring using the conventional equipment may not be possible in the step-down nursery and could be resource intense [4]. Hence, we need to look at an alternate option of continuous monitoring beyond the standard equipment which can work even at less resource intensive scenario.
Advancements in latest technology is offering miniaturized wireless remote continuous monitoring systems which can enable early identification of physiological derangements and familyoriented care, ultimately reducing the duration of hospital stay and financial burden of the parents [5-8]. Ideally, such systems should be convenient to use and should be capable of providing reliable monitoring of infants in any setting, including home. There should be ease while fixing the device to the neonate. The presence of the monitoring device should not evoke any undue anxiety to the parents and should not undermine the confidence of the mother in handling her baby [9,10]. However, the traditional sensors and medical instruments cannot be used for monitoring, as they are bulky in size, with dangling wires and more expensive when compared to such innovative, compact, wireless and affordable devices. Continued use of conventional systems creates an impression among parents that their babies are still sick and require higher level of care.
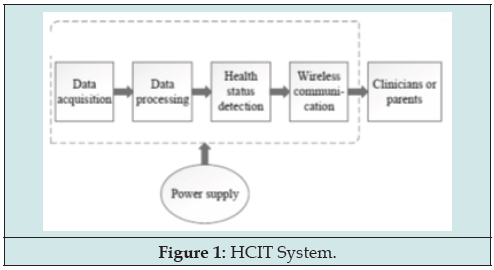
Recent technology offers the use of Healthcare Internet of Things (HCIT) devices for continuous monitoring which could be an answer to the requirement of continued monitoring in some of the babies beyond the NICU. One such system is I Vital (Developed by HELYXON Healthcare solutions pvt ltd) which helps in remote monitoring of neonate’s heart rate, saturation and temperature using two sensors. However, it has not been studied and validated in neonates previously. This study aims at studying the feasibility of using the I Vital system for neonates. This HCIT system uses nanotechnology sensors, low power consuming microcontrollers and simplified wireless communication technology. The HCIT systems could be produced at an affordable cost and can be scaled up for mass adoption. Further use of wireless sensors and skin friendly casing of the device effectively avoids the disturbance to infants caused by conventional sensor techniques which include skin irritation, hampering due to wires, interruption of sleep (Figure 1).
These wireless devices function on the concept of data acquisition by use of sensors attached to the neonate’s body which is the processed using software and the vital parameters are recorded continuously and are available remotely anytime, anywhere for interpretation by the clinician at his convenience. The Clinician’s Laptop, Mobile Slate or his Smart Phone becomes his command centre to remotely monitor and interact with multiple patients simultaneously, while he is on the move. The advantages of these wireless devices include affordability for even poor patients, reduced patient disturbance, reduced workload for nurses, ease of use (fixing and removing), and more importantly it empowers the parents to be part of their infant care. Another aspect of these HCIT devices includes its utility in safe transport of neonates between wards, the operating room, radiology department and between t facilities (Figures 2-4).
Methods
Study Design
Pilot study (observational study).
Study Population
Neonates delivering at Saveetha medical college and hospital, Thandalam.
Study Period
December 2017 to August 2018.
Sample Size
Convenient sample size.
Objectives of the Study
Primary Objective
To evaluate if continuous remote monitoring of vitals using I Vital system has the capability to detect abnormal variation of the monitored during the observation period of 24-48 hours when compared to the intermittent monitoring using routine techniques.
Secondary Objective
To find out the sensitivity, specificity, positive and negative predictive value of I Vital system compared to routine monitoring using the Masimo pulse oximeter and radiant warmer.
Study Population
The study population included well term neonates and stable preterm neonates born in Saveetha medical college hospital.
Inclusion Criteria
Group I - Term and well newborn babies in the Postnatal ward.
Group II –Preterm babies after stabilization in NICU.
Exclusion Criteria
a) Babies with congenital malformations or syndromes
b) Babies with clinical sepsis or proven sepsis and on IV antibiotics
c) Babies who died.
Study Method
Babies were recruited consecutively once they fulfilled the inclusion criteria. The neonates born at Saveetha medical college between December 2017 and August 2018 were included in the study. Of the total number of deliveries during the study period was 462 of which 92 babies was included for the study purpose. The babies included were studied for a total period of 2188 hours, Majority of the babies were term babies who were monitored for 1570 hours while preterm babies were monitored 618 hours. We trained our staff nurses on the use of the I Vital system and how to record the findings. A special nurse was recruited for the study purpose for making data entry. 98.6 Fever-Watch was attached to the right upper quadrant of the anterior abdomen wall when baby is in supine and in the right flank when baby is in prone position using the Fever-Watch Band. The pulse oximetry sensors were attached to the left lower limb or the right lower limb (in case of an intravenous cannula in the left lower limb) to record the post ductal saturation and heart rate. The nurse appointed for the research study checked the interface fixation to the baby. Once the device is attached and the mobile application I Vital is turned on, 98.6 Fever-Watch starts recording baby temperature continuously and the pulse oximetry sensor records the saturation and heart rate continuously. The system has a lag time of 1 minute to record the events which could be modified if needed.
The data was collected from the device and stored in the log. This information was printed on to excel sheet for study purposes. Routine Intermittent vitals recording every 4 hours as per unit protocol was continued by staff nurse. The lower and higher alarm limits were set at 36.4o C and 37.5o C for Temperature and at 100 bpm and 160 bpm for Heart Rate (HR), below 91 for Blood Saturation (SpO2) respectively. If any recording were outside the range limit, the mobile device (Parent’s) which is connected to this I Vital system through Bluetooth or Wi-Fi system raises an alarm. Simultaneously the nurse would get the intimation in the central monitoring device (IPAD /TAB). The nurse then immediately checked for the device to be misplaced on the baby’s body. If the sensor found to be in right place and still the measurement readings are beyond the set alarm limits the vital parameters were counter checked manually using Digital Thermometer or on the patient monitoring system accordingly and recorded in the Event log form along with other details observed. If the vitals of the baby become normal the baby would continue to be in the study. If the vitals do not normalize, then study was deemed to have reached its end point and baby shifted to NICU.
End Points of the Study
The end point of the study for the participants was detection of derangements in the vital parameters or specified duration (24-48 hours) of the study for the baby.
Data Entry &Statistical Analysis
Data entry was done using Excel 2010 (Microsoft, Redmond, WA, USA). Analysis was done by using Excel 2010 for Windows. Data were analyzed for sensitivity, specificity, positive and negative predictive value.
Results
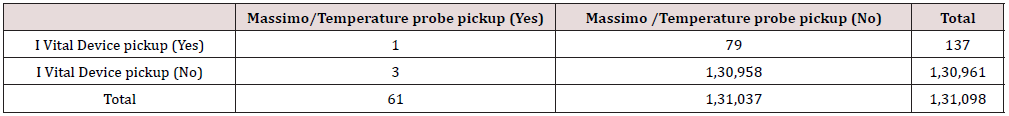
During the study period babies were monitored for a duration of 2188hours and findings were studied (91 babies were monitored for a period of 24 hours and one bay was monitored for 4 hours). The I Vital device was designed to record the events (Heart rate, Blood Oxygen Saturation and Temperature) continuously, but recordings were made with a lag time of 1 minute. Hence the total events that were recorded were 131,100 events. Preterm babies included in the study were monitored for 25 baby days and 18 hours resulting in recording of 37,080 events and term babies included were studied for 65 baby days and 10 hours resulting in recording of 94,020 events. The sensitivity, specificity positive and negative predictive values are as shown in the tables below (Figure 5) (Tables 1-4).
Sensitivity = 95.1%; 95% CI (86.51-98.30).
Specificity = 99.9%; 95% CI (99.94 – 99.95).
Positive predictive value = 42.34%: 95% CI (34.38 – 50.71).
Negative predictive value = 100%; 95% CI (99.9 – 100.0).
Table 2: I Vital System vs Routine Monitoring-Temperature. Temperature Monitoring for Term and Preterm Babies
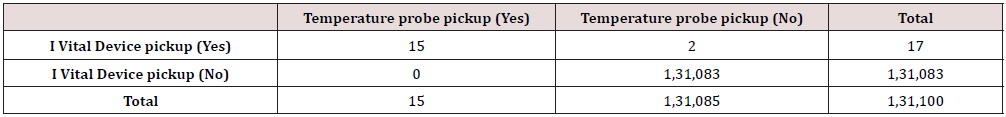
Sensitivity = 100.0%; 95% CI (79.61 – 100.0).
Specificity = 100.0%; 95% CI (99.9 – 100.0).
Positive predictive value = 88.2%: 95% CI (65.6 – 96.7).
Negative predictive value = 100%; 95% CI 100.0 – 100.0).
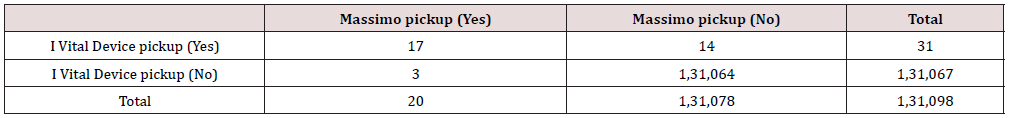
Table 3: I Vital system vs Routine Monitoring- SpO2. SpO2 Monitoring Parameters Combined Term and Preterm Babies

Sensitivity = 100.0%; 95% CI (88.65 – 100.0).
Specificity = 99.95%; 95% CI (99.94 – 99.96).
Positive predictive value = 31.91%: 95% CI (23.36 – 41.89).
Negative predictive value = 100%; 95% CI 100.0 – 100.0).
Table 4: I Vital system vs Routine Monitoring- HR For Preterm and Term. Heart Rate Monitoring Parameters for Preterm and Term Babies
Sensitivity = 85%; 95% CI (63.96 – 94.76).
Specificity = 99.9%; 95% CI (99.92 – 99.99).
Positive predictive value = 54.84%: 95% CI (37.77 – 70.84).
Negative predictive value = 100%; 95% CI 99.9 – 100.0).
Discussion
The study was done to assess the technical feasibility of using I Vital system for monitoring neonates in the level 1 NICU and postnatal ward and to demonstrate if I Vital system could help in early indication of sickness and to compare it with routine monitoring done by Masimo pulse oximeter and Thermistor probe.
Technical Feasibility
The method of using wireless sensors to monitor vital parameters of the neonates requites the need for a continuous Wi-Fi system, an android or an iOS supporting mobile phone and a central monitoring system in form of a desktop/laptop/IPAD. This kind of sophisticated equipment’s may be used in the in hospital setting but the use of the same in a home setting needs to be studied further before this can be adopted as a remote monitoring tool for neonates discharged to home. Previous studies which have used these kinds of wireless devices have also shown that this technology is technically feasible and an important addition to the treating physicians, aiding them in effective monitoring.
Vitals Monitoring
The I Vital system comprises of 2 devices fever watch 98.4 to monitor the temperature and pulse oximeter to demonstrate heart rate and Spo2 changes. Overall, the I Vital system had Sensitivity of 95.1%; 95% CI (86.51-98.30), Specificity of 99.9%; 95% CI (99.94 – 99.95), Positive predictive value of 42.34%: 95% CI (34.38 – 50.71) and Negative predictive value of 100%; 95% CI (99.9 – 100.0) when all parameters (Temperature, Heart rate and Spo2) were analyzed together for both term and preterm babies. There were 15 incidents were there was temperature variations were picked up by the temperature probe which were also picked up the Fever watch 98.4. There two instances of hypothermia which were recorded by Fever watch 98.4 which were missed /not picked up by routine monitoring. Overall, when temperature alone was used as the parameter to compare the I Vital system and conventional monitoring it was observed that the I Vital system had a Sensitivity = 100.0%; 95% CI (79.61 – 100.0) Specificity = 100.0%; 95% CI (99.9 – 100.0) Positive predictive value = 88.2%: 95% CI (65.6 – 96.7) Negative predictive value = 100%; 95% CI 100.0 – 100.0).
Since the preterm babies were under strict monitoring in the NICU there was no documented hypothermia among the preterm subgroups. Further it was noticed that among the term babies who were nursed with the mothers the fever watch 98.4 was able to pick up 2 instances of hypothermia earlier than the conventional monitoring system helping in initiation of early intervention. The Spo2 and heart rate parameters were analyzed using the I Vital pulse oximeter. With respect to Spo2 there were 64 instances where the I Vital system gave a false alarm similarly there were 14 occasions where a false alarm in Heart rate variations were noticed. Analysis of the reason for these false alarms was made and it was determined that the Spo2 monitoring by the I Vital system was affected by movement artifacts. Another possible factor which interfered with the I Vital monitoring was the use of phototherapy.
It was noticed that among babies who were on phototherapy the Spo2 and heart rate pick up by the I Vital system was erroneous possibly due to interference of phototherapy light with the Infrared light of the pulse oximeter which resulted in the false alarms when the babies where on phototherapy. An attempt was made during the study process to overcome this short come by using opaque cloth to cover the sensor probe site used for measuring the saturation. There were 3 instances where the I Vital system failed to pick up Heart rate changes which were picked up by conventional monitoring. These were instances of sleeping bradycardia which recovered within 10 seconds and I Vital system did not pick this possibly due to the response time of pulse oximeter being longer than this 10 second. There were few instances where the alarm raised by I Vital system were missed by the staff nurse managing the neonate this was particularly observed in the heart rate parameter.
Variations Among Term and Preterm Babies
Subgroup analysis of vital parameters for preterm babies showed sensitivity of100.0%; 95% CI (75.75 – 100.0), Specificity of 99.95%; 95% CI (99.92 – 99.97), Positive predictive value of 38.71%: 95% CI (23.73 – 56.18) and Negative predictive value of 100%; 95% CI 100.0 – 100.0). Similarly, when term babies were analyzed separately the monitoring using I Vital system showed Sensitivity of 93.88%; 95% CI (83.48 – 97.9), Specificity of 99.94%; 95% CI (99.92 – 99.95), Positive predictive value of 43.4%: 95% CI (34.36 – 52.9) and Negative predictive value of 100%; 95% CI 100.0 – 100.0). No major differences were noted compared to the overall results in the subgroup analysis.
Similarly, subgroup analysis was done for different parameters namely Heart rate, Saturation and Temperature. No major differences were noted in the results. The statistical analysis of performance I Vital system when compared to conventional monitoring system indicates that it can be used as an alternative to routine monitoring in places where it is technically feasible. The positive predictive value of the system is hampered by the false alarms due to movement and light interaction and it is suggested that few improvements could be made to the existing system like use of opaque cloth to cover the probe site, use of better sensors which use signal extraction technology which have been found to be associated with lesser incidence of movement and light artifacts.
Satisfaction of the Users
Though no formal efforts were made to study this parameter objectively, but on discussing with the staff and the parents the overall satisfaction of the staff using the system was good as they were able to pick up alarms earlier which they said would have missed otherwise. Similarly, mothers felt that they were able to give Kangaroo mother care comfortably while the neonate was monitored using the I Vital system. This Zero separation of the mother and babies could possibly help in better breastfeeding, faster weight gain, earlier discharge which in turn would be an important factor in reducing the health care associated cost and morbidity of the neonates. Previous studies using these wireless monitors also show similar parental and nursing experiences with use of this kind of technology. Another aspect of this system is that it helps to monitor the babies during transport for hearing screening, Radiological investigations, and Echocardiogram this I Vital system helped in monitoring their babies easily when compared to the conventional monitoring system.
Adverse Effects
No major adverse effects were noted by using these wearable sensors, a log of the adverse events was made to look at the adverse effects like probe site skin damage, erythema, burns. Long term effects like sleep disturbances, effect of Wi-Fi system on neonates’ growth and behavior need further studies [11-13].
Conclusions
I Vital system of monitoring the neonates could be an alternate to routine monitoring in places where it is technically feasible. No major adverse effects were noticed while using the sensors but its effect in the long term needs to be followed up. The system of monitoring is shown to be as effective in identifying illness in neonates as routine monitoring and can be used for monitoring neonates during transportation and in the postnatal wards and possibly at home.
Funding
The health care devices and monitoring devices used in the study were provided by HELYXON Healthcare solutions Pvt Ltd, IIT Madras Research Park. Taramani, Chennai, India.
Competing Interests
None declared.
Patient Consent
Obtained.
Ethics Approval
The study received ethical approval from the University Research Ethics Committee.
References
- Weenk M, van Goor H, Frietman B, Engelen LJ, van Laarhoven CJ, et al. (2017) Continuous Monitoring of Vital Signs Using Wearable Devices on the General Ward: Pilot Study. JMIR Mhealth Uhealth 5(7): e91.
- Nangalia V, Prytherch DR, Smith GB (2010) Health technology assessment review: Remote monitoring of vital signs - current status and future challenges. Crit Care 14(5): 233.
- Zhu Z, Liu T, Li G, Li T, Inoue Y (2015) Wearable sensor systems for infants. Sensors (Basel, Switzerland) 15(2): 3721-3749.
- Mohajerani S, Moosavi AH, Rihawi RA, Ahmed B, Bhat AN, et al. (2015) A cloud-based system for real-time, remote physiological monitoring of infants. 2015 IEEE International Symposium on Signal Processing and Information Technology (ISSPIT) pp. 565-569.
- Rimet Y, Brusquet Y, Ronayette D, Dageville C, Lubrano M, et al. (2007) Evaluation of a new, wireless pulse oximetry monitoring system in infants: the BBA bootee. In: Leonhardt S., Falck T., Mähönen P. (eds) 4th International Workshop on Wearable and Implantable Body Sensor Networks (BSN 2007). IFMBE Proceedings 13: 143-148.
- Petersen CL, Chen TP, Ansermino JM, Dumont GA (2013) Design and evaluation of a low-cost smartphone pulse oximeter. Sensors (Basel, Switzerland) 13(12): 16882-16893.
- Bonner O, Beardsall K, Crilly N, Lasenby J (2017) 'There were more wires than him': the potential for wireless patient monitoring in neonatal intensive care. BMJ Innov 3(1): 12-18.
- Jämsä K, Jämsä T (1998) Technology in neonatal intensive care--a study on parents’ experiences. Technol Health Care 6(4): 225-230.
- Chen W, Nguyễn ST, Coops R, Oetomo SB, Feijs L (2009) Wireless transmission design for health monitoring at neonatal intensive care units. 2nd International Symposium on Applied Sciences in Biomedical and Communication Technologies p. 1-6.
- Cleveland LM (2008) Parenting in the neonatal intensive care unit. J Obstet Gynecol Neonatal Nurs 37(6): 666-691.
- Russell G, Sawyer A, Rabe H, Abbott J, Gyte G, et al. (2014) Parents’ views on care of their very premature babies in neonatal intensive care units: a qualitative study. Bmc Pediatr 14: 230.
- Wikström AC, Cederborg AC, Johanson M (2007) The meaning of technology in an intensive care unit--an interview study. Intensive Crit Care Nurs 23(4): 187-195.
- Valberg PA, van Deventer TE, Repacholi MH (2006) Workgroup report: base stations and wireless networks-radiofrequency (RF) exposures and health consequences. Environ Health Perspect 115(3): 416-424.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...