
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4722
Case Report(ISSN: 2637-4722) 
Calcification is Not Always a Specific Marker for Malign Thyroglossal Duct Cysts Volume 4 - Issue 3
Suzen A1*, Karakus SC2, Ortanca A3, Erturk N2 and Dere Y4
- 1Department of Pediatric Surgery, Mugla Sıtkı Kocman University Research and Training Hospital, Mugla, Turkey
- 2Department of Pediatric Surgery, Mugla Sıtkı Kocman University, Faculty of Medicine, Mugla, Turkey
- 3Department of Pediatrics, Mugla Sıtkı Kocman University, Faculty of Medicine, Mugla, Turkey
- 4Department of Pathology, Mugla Sıtkı Kocman University, Faculty of Medicine, Mugla, Turkey
Received: April 27, 2023 Published: May 08, 2023
Corresponding author: John R. Bach, Department of Physical Medicine and Rehabilitation, Rutgers New Jersey Medical School, Newark, NJ, USA
DOI: 10.32474/PAPN.2024.04.000186
Abstract
Calcification in a thyroglossal duct cyst is known as a hallmark for malignancy. Although rare, benign calcified thyroglossal cyst may be kept in mind to retain surgeon from additional surgical procedures. Since 3 of 4 cases of benign thyroglossal duct cyst and calcification comorbidity were reported under 21 years old, unlike adults, calcification cannot be accepted as a specific marker for malignancy in childhood. To our knowledge, our patient is the first reported recurrent and the third pediatric benign calcified thyroglossal duct cyst in the literature.
Keywords: Calcification; thyroglossal duct cyst; malignancy
Introduction
Thyroglossal duct cysts (TDCs) are the most common congenital anomalies of the midline cervical region. They rise from unobliterated epithelial remnants of the thyroglossal duct that are present during the descent of the thyroid gland in embryological development. Carcinoma arising within a TDC has been reported to occur in approximately 0.7 to 1.4 % of cases, with papillary thyroid carcinoma being the most common type [1,2]. Discrimination of carcinoma from benign TDC with clinical findings is usually not possible [3]. Calcification determined by ultrasonography or computed tomography in TDC is asserted to be a specific marker for preoperative diagnosis for malignancy, which is seen %1 of TDCs [4]. We here aim to demonstrate that all calcifications in TDCs are not hallmark for malignancy by presenting the first benign recurrent TDC case whose histopathological examination revealed calcification of the cyst wall.
Case Presentation
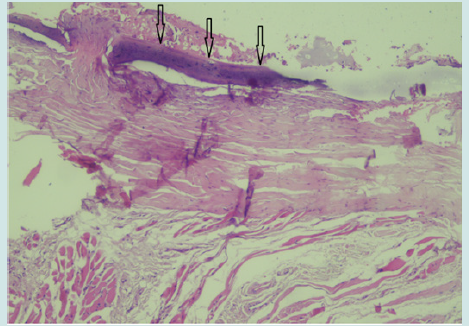
A 5-year-old boy presented with troublesome discharge, tenderness, and redness in front of his neck. An operation had been performed for TDC at another clinic a year ago, records of which were not available. He had the history of midline neck abscess three times since that. The rest of his medical history was unremarkable. Following the resolution of the infection with antibiotic treatment, physical examination revealed a cystic swelling which situated below the hyoid in the midline. It is harder than the TDCs that we treated before. Fixation to surrounding tissues was not let to movement of the mass with deglutition and tongue protrusion. Thyroid gland was normal by palpation. Ultrasound scan of the neck showed a subpharyngeal subcutaneous cyst in size of 24x12 mm with anechoic content located below the hyoid bone. No calcifications or mural nodules were noted in the cyst. There was no significant cervical lymphadenopathy. The thyroid gland was normal. A standard Sistrunk procedure was performed with resection of the cyst in continuity with the central section of the hyoid bone and excision of the duct up to foramen caecum for recurrent TDC. The histopathological findings confirmed fibrocartilages tissue and calcified cyst wall (Figure 1). No malignant cells were seen. Lymphocytes and plasma cells were reported. The cyst was interpreted as calcified benign TDC. The patient had an uneventful postoperative course. Two-year clinical follow up is uneventful without any complication or recurrence.
Figure 1: Microscopic examination revealed calcified cyst wall (arrow) with lymphocytes and plasma cells (hematoxylin-eosin, x 100).
Discussion
Thyroglossal duct occurs during embryonic development of the thyroid gland. It evolves as a tract during caudal migration of thyroid gland from the foramen cecum of the tongue to its final peritracheal position in the inferior neck. Persistent remnants of thyroglossal duct may manifest TDCs which may present at any level, from the base of the tongue to the thyroid isthmus. It is classically located anterior midline or slightly to one side and below the hyoid bone and moves with swallowing and tongue protrusion. The two most common complications of TDC are infection and malignancy [5]. Thyroglossal duct cyst carcinomas are encountered predominantly in adults, typically in the third and fourth decades of life and rarely in childhood. The clinical presentation of TDC carcinoma may be indistinguishable from a benign TDC [6]. The suspicious clinical features of TDC carcinomas are dysphasia, dysphonia, presence of palpable cervical lymph nodes, a rapidly enlarging, hard and fixed neck mass, and older age. However, in our benign case, the mass is not moving freely with deglutition and tongue protrusion due to fixation to surrounding tissues secondary to recurrent infections. The presence of a solid component, mural nodule or calcification on ultrasonography or computed tomography are signs that point to the possibility of TDC carcinoma.
We only performed ultrasonography in our child due to its lack of reliance on ionizing radiation or the need for sedation and it reveals no calcification. Glastonbury et al. [3] investigated CT and MR imaging’s of 21 cases of adult TDCs and determined that four of six (66%) malignant cases had shown calcifications and any benign cases has shown calcifications. Finally, they suggested that calcification, which is seen best on CT scans, was a specific imaging feature of carcinoma in TDC, especially in adults. In another study, Thompson et al [7] noted the presence of calcifications in 3 of 22 patients with TDC carcinomas in imaging studies. To our knowledge, there have been only 4 reports of a TDC with calcification, 2 of whom are in the pediatric age group. Calcification of the wall of benign TDC was first reported by Monzen in 1991 in a 52-year-old man, and then Kervancıoğlu et al. in a 20-year-old girl [8,9]. Ayala et al. [6] reported psammomata’s calcifications with a benign TDC in a 3-year-old-boy which is defined as the most likely to occur in papillary thyroid gland. The other pediatric case of benign calcified TDC was reported in 2017 by Al-Yahya et al. [10]. To our knowledge, our patient is the first reported recurrent and the third pediatric benign calcified TDC. Chronic inflammations are known to trigger cellular events that can promote malignant transformation of cells and carcinogenesis [11].
Afterwards, chronic inflammation is presumably associated with the progressive calcifications [12]. It is speculated that the calcifications in benign TDCs may thus be secondary to chronic inflammation. History of previous surgery, recurrent infections and reported lymphocytes and plasma cells which were the signs of chronic inflammation support this opinion in our case. Thompson et al. analyzed 59 cases of TDC carcinoma affecting patients aged 6-20 years in the English literature [13]. Histologically, papillary thyroid carcinomas are the only malignancy determined in TDCs. Thyroidectomy (n=29) and lymph node dissection (n=20) were performed in addition to Sistrunk procedures. They also reported administration of postoperative radioactive iodine in 20 patients and 4 recurrences. As it can be seen from this review in pediatric population, although the universally recommended management for TDC carcinoma is a Sistrunk procedure, the management of TDC carcinomas in the pediatric population is controversial. Thus, preoperative findings of calcification on imaging studies can lead surgeons to perform thyroidectomy or lymph node dissection. With further reports, although benign calcified TDC is rarely documented, the presence of calcification on imaging is not accepted as the hallmark of an associated carcinoma which can lead to unnecessary surgical procedures. This case proves that not all calcified TDCs are malignant.
Conclusion
Thyroglossal duct cyst carcinoma is highly suspected in the presence of calcification on imaging. However, like the calcification in our case, it may develop secondary to previous surgery and recurrent infections. Although rare, benign calcified thyroglossal cyst may be kept in mind to retain surgeon from additional procedures. Since most cases of benign TDC and calcification comorbidity were reported under 21 years old, unlike adults, calcification cannot be accepted as a specific marker for malignancy in childhood.
Conflicts of interest
None.
Funding
No financial support for the study.
References
- HM Heshmati, V Fatourechi, JA van Heerden, ID Hay, JR Goellner (1997) Thyroglossal duct carcinoma: report of 12 cases. Mayo Clin Proc 72(4): 315-319.
- J de Tristan, J Zenk, J Künzel, G Psychogios, H Iro (2015) Thyroglossal duct cysts: 20 years’ experience (1992-2011). Eur Arch Otorhinolaryngol 272(9): 2513-2519.
- CM Glastonbury, HC Davidson, JR Haller, HR Harnsberger (2000) The CT and MR imaging features of carcinoma arising in thyroglossal duct remnants. AJNR Am J Neuroradiol 21(4): 770-774.
- S Smiti, NS Mahmood (2009) Papillary carcinoma arising from a thyroglossal duct cyst. Indian J Radiol Imaging 19(2): 120-122.
- V Mondin, A Ferlito, E Muzzi, CE Silver, JJ Fagan, et al. (2008) Thyroglossal duct cyst: Personal experience and literature review. Auris Nasus Larynx 35(1): 11-25.
- C Ayala, GB Healy, CD Robson, SO Vargas (2003) Psammomatous calcification in association with a benign thyroglossal duct cyst, Arch. Otolaryngol. Head Neck Surg 129(2): 241-243.
- LDR Thompson, HB Herrera, SK Lau (2017) Thyroglossal Duct Cyst Carcinomas: A Clinicopathologic Series of 22 Cases with Staging Recommendations. Head Neck Pathol 11(2): 175-185.
- Y Monzen, T Watanabe, K Nakanishi, K Iwasaki, H Mori, et al. (1991) Ultrasonography and CT of thyroglossal duct cysts. Nihon Igaku Hoshasen Gakkai Zasshi 51(4): 400-405.
- R Kervancioğlu, MM Bayram, A Ozkur, K Bakir (2000) A thyroglossal duct cyst with calcification. Neuroradiology 42(12): 923-925.
- SN Al-Yahya, MH Lye, CP Loo, MB Marina (2017) Benign Calcified Thyroglossal Duct Cyst, –Defying the Hallmark of Papillary Carcinoma, 4th Case Reported in Literature. Int Med J Malay 16(2): 117-120.
- G Landskron, M De la Fuente, P Thuwajit, C Thuwajit, MA Hermoso (2014) Chronic inflammation and cytokines in the tumor microenvironment. J Immunol Res 2014: 49185.
- K Mineda, S Kuno, H Kato, K Kinoshita, K Doi, et al. (2014) Chronic Inflammation and Progressive Calcification as a Result of Fat Necrosis: The Worst Outcome in Fat Grafting. Plast Reconstr Surg 133(5): 1064-1072.
- LDR Thompson, HB Herrera, SK Lau (2017) Thyroglossal Duct Cyst Carcinomas in Pediatric Patients: Report of Two Cases with a Comprehensive Literature Review. Head Neck Pathol 11(4): 442-449.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




